Emergency Medical Services Program Policies – Procedures – Protocols
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
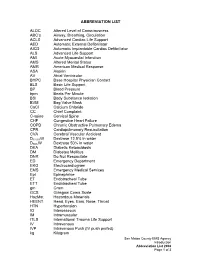
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Critical Care Nursing of Infants and Children Martha A
University of Pennsylvania ScholarlyCommons Miscellaneous Papers Miscellaneous Papers 1-1-2001 Critical Care Nursing of Infants and Children Martha A. Q. Curley University of Pennsylvania, [email protected] Patricia A. Moloney-Harmon The Children's Hospital at Sinai Copyright by the author. Reprinted from Critical Care Nursing of Infants and Children, Martha A.Q. Curley and Patricia A. Moloney-Harmon (Editors), (Philadelphia: W.B. Saunders Co., 2001), 1,128 pages. NOTE: At the time of publication, the author, Martha Curley was affiliated with the Children's Hospital of Boston. Currently, she is a faculty member in the School of Nursing at the University of Pennsylvania. This paper is posted at ScholarlyCommons. http://repository.upenn.edu/miscellaneous_papers/4 For more information, please contact [email protected]. Please Note: The full version of this book and all of its chapters (below) can be found on ScholarlyCommons (from the University of Pennsylvania) at http://repository.upenn.edu/miscellaneous_papers/4/ Information page in ScholarlyCommons Full book front.pdf - Front Matter, Contributors, Forward, Preface, Acknowledgements, and Contents Chapter 1.pdf - The Essence of Pediatric Critical Care Nursing Chapter 2.pdf - Caring Practices: Providing Developmentally Supportive Care Chapter_3.pdf - Caring Practices: The Impact of the Critical Care Experience on the Family Chapter_4.pdf - Leadership in Pediatric Critical Care Chapter 5.pdf - Facilitation of Learning Chapter_6.pdf - Advocacy and Moral Agency: A Road Map for -

Barbiturate Blood Levels Found at Necropsy in Proven Cases of Acute Barbiturate Poisoning
J. clin. Path., 1970, 23, 435-439 J Clin Pathol: first published as 10.1136/jcp.23.5.435 on 1 July 1970. Downloaded from Barbiturate blood levels found at necropsy in proven cases of acute barbiturate poisoning ROGER GILLETT AND FRANK G. WARBURTON From the Department ofPathology, Hope Hospital, Salford, Lancs SYNOPSIS In order to determine whether blood barbiturate levels could be used to ascertain that death had been caused by barbiturate overdose, samples of blood from 128 subjects of coroners' necropsies were examined for barbiturate content. Sixty of these were well authenti- cated cases of barbiturate overdosage, and barbiturates were implicated, together with other factors such as alcohol and carbon monoxide, in a further 16 cases. The remaining 52 cases were of an eliminatory nature, 10 of which had low barbiturate blood levels considered to be within the therapeutic range. The results indicate that when the accepted levels producing loss of consciousness are exceeded, and maintained, death will ensue if treatment is not given. These results may be of value in assessing findings in necropsies requested by the coroner, and are in no way applicable to the living patient in whom it is well established that recovery from higher blood levels http://jcp.bmj.com/ may take place if adequate treatment is available. Anatomical evidence of barbiturate poisoning but he notes that it must not be inferred that on September 23, 2021 by guest. Protected copyright. at necropsy is not specific, often amounting only finding these levels constitutes prima facie to signs of asphyxia. The presence of powder evidence of death from barbiturate poisoning. -

FIRST AID QUICK SHEET- Airway and Breathing
FIRST AID QUICK SHEET Airway and Breathing After you have checked to make sure the scene is safe and put on gloves to protect yourself (Danger) and checked if the patient is responsive (Response), if you find the patient is not responding, you should think: ABC. First check for an Airway and Breathing. Instructions for the A and B steps of the DR. ABC acronym for first aid priorities are below: How to Adjust Someone’s Airway (A): 1. Gently swipe the mouth with one finger to ensure that no objects are blocking the airway. 2. Place two fingers under the casualties chin and one hand on the forehead. 3. Gently lift the chin with two fingers, removing the tongue from the back of the throat. 4. If transport is delayed, roll the casualty onto their side in the recovery position to allow fluids to drain from the mouth Note: If someone is able to speak, their airway is open. Breathing (B): 1. Always remember to look, listen, and feel when checking for breathing. 2. LOOK to see the chest rise and fall. 3. LISTEN to hear breath sounds. 4. Place one hand on the stomach and FEEL for breathing movement and FEEL beneath the nose for air movement. After you have secured an airway and checked for breathing, you may move on to check for bleeding in the C (circulation) step of DR. ABC. *Please be safe and practice first aid at your own risk. LFR International is not liable for injuries resulting from any first aid attempts. . -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming -

Abdominal Pain 02/02/2021
Medical Control Board Approved Protocols ABDOMINAL PAIN 02/02/2021 Follow Assessment, General Procedures Protocol EMR • Assess and support ABCs • Position of comfort • Supine if: • Trauma • Hypotension • Syncope • NPO • Monitor vital signs • Oxygen indicated for: • Unstable vitals • Severity of pain • Suspected GI bleed EMT • 12-lead – See CARDIAC-ECG/12 Lead Procedure A-EMT • IV – NS with standard tubing • Titrate fluid to patient’s needs – See Shock Protocol EMT-I/ • Cardiac monitoring PARAMEDIC • Pain management – See Acute Pain Management Protocol 199 March, 2021 Medical Control Board Approved Protocols This page intentionally left blank 200 March, 2021 Medical Control Board Approved Protocols ACUTE ADRENAL INSUFFICIENCY PROTOCOL 02/02/2021 Follow Assessment, General Procedures Protocol • Acute adrenal insufficiency (crisis) can occur in the following settings: - During neonatal period (undiagnosed adrenal insufficiency) - In patients with known, pre-existing adrenal insufficiency (e.g., Addison’s disease) - In patients who are chronically steroid dependent (i.e., taking steroids daily, long- term, for any number of medical conditions) - Adrenal crisis can be triggered by any acute stressor (e.g., trauma or illness), as well as by abrupt cessation of steroid use (for any reason). • Signs/symptoms of adrenal crisis: Altered mental status, seizures; generalized weakness, hypotension, hypoglycemia, hyperkalemia. • Notify hospital you are transporting known/suspected adrenal crisis patient • Emergency transport for: ALOC, hypotension, hypoglycemia, suspected hyperkalemia. Acute adrenal crisis is an immediately life-threatening emergency, and must be treated aggressively EMR • PMH, Take thorough history of patient’s steroid use/dependence. Determine if the patient is on oral hydrocortisone. • Assess and support ABC’s • Oxygen therapy, as needed • Monitor vitals EMT • Check blood glucose • If blood glucose is <60: administer glucose solution orally if the patient is awake and able to protect own airway • Obtain 12 lead ECG; if time permitted. -

Triage and Scenario
Triage and Scenario By Bryan Lewis Triage Triage: Is a rapid approach to prioritizing a large number of patients Incident Casualty Collection Triage Site Point Officer/Treatment/Transport S imple T riage A nd R apid T reatment Triage ● Triage should be performed RAPIDLY ● Utilize START Triage to determine priority ● 30–60 seconds per patient ● Affix tag on left upper arm or leg – Triage 1. Scene Safety BSI and Identify number of patients, and types of injuries, communicate to EMS 2. Clear the “walking wounded” with verbal instruction: If you can hear me and you can move, walk to… (Use a PA System if Possible) 3. Direct patients to the casualty collection point (CCP) or treatment area for detailed assessment and medical care Green Minor Manager/Triage Officer will be the area to control patients and manage area 4. Green tag will be issued at the CCP These patients may be classified as MINOR START Triage Now use START to assess and categorize the remaining patients… USE Color System START-Triage Now categorize the patients by assessing each patient’s RPMs… ✓Respirations ✓Pulse ✓Mental Status START—RPM RESPIRATIONS Is the patient breathing? Yes Adult – respirations > 30 = Red/Immediate Pediatric – respirations < 15 or > 45 = Red/Immediate Adult – respirations < 30 = check pulse Pediatric – respirations > 15 and < 45 = check pulse START—RPM RESPIRATIONS Is the Patient Breathing? No Reposition the airway… Respirations begin = IMMEDIATE/RED If patient doesn’t breath . ▪ Adult – deceased = BLACK ▪ Pediatric: Pulse Present – give 5 rescue breaths -

Paramedic Update
PARAMEDIC UPDATE 2020 AGENDA Protocol format New medications Base contact requirements Against Medical Advice Pediatric King Airway Protocol changes New Policies Determination of death Online Certifications- Image trend NEW PROTOCOL FORMAT Public safety, EMT, and Public safety personal can Adults and Pediatric are on Paramedic protocols are in only perform skills in the top the same page. one document. canary yellow section Anything listed in the yellow EMT’s can perform any skills Paramedics will start with ALS section is a standing in the green BLS section the BLS section (BLS before order. Base contact must be located below the public ALS!) and move down into attempted for anything in the safety area. the ALS section as needed. red “base hospital contact required” section. NEW PROTOCOL FORMAT Adults Pediatrics (13 years and under) Public Safety First Aid Procedures: Only Public Safety First Aid Procedures: Only • Remove nearby objects to prevent injury to Patient. Place • Remove nearby objects to prevent injury to Patient. Place patient in recovery position on left side patient in recovery position on left side • Give Oxygen if available • Give Oxygen if available • Request Fire/EMS • Request Fire/EMS • Public safety will start here BLS Procedures: EMT’s and Paramedics start here BLS Procedures: EMT’s and Paramedics start here • Support ABC’s • Support ABC’s • Give Oxygen only if Spo2 < 94% or if in Respiratory Distress • Give Oxygen only if Spo2 <94% or if in Respiratory Distress • Blood Glucose Check, if hypoglycemic enter appropriate • Blood Glucose check, if hypoglycemic enter appropriate protocol protocol • EMT and Paramedic start here • If Focal seizure, place patient in position of comfort, rapid • If Focal seizure, place patient in position of comfort, rapid transport or ALS Rendezvous transport or ALS Rendezvous • If full body tonic/clonic seizure, prepare to support • If full body tonic/clonic seizure, prepare to support respirations, provide cooling measures if febrile respirations. -

First Aid & CPR Training Inc. “At a Glance”
First Aid & CPR Training Inc. REFERENCE MANUAL “At A Glance” 2 Introduction 3 Emergency Scene Management 13 Life Threatening Priorities 15 Levels of Consciousness and Shock 20 Heart Attacks, Strokes, and Heart-Smart Awareness 26 CPR 30 Automated External Defibrillation (AED) 32 Health Care Providers (HCP) 35 Choking 40 Wounds and Bleeding 46 Medical Conditions (Asthma, Allergies, Diabetes and Seizures) 54 Bone and Joint Injuries 58 Head and Spinal Injuries 62 Eye, Ear and Nose Injuries 65 Burns 68 Poisons 70 Opioid Overdoses 71 Cold and Heat Injuries 76 Rescue Carries 77 In Closing 78 Quiz ATTENTION Please pay extra attention when you see this symbol. Introduction Hello from all of us at Lifesaver 101 First Aid & CPR Training Inc. Thank you for selecting Lifesaver 101 to provide you with educational, enjoyable and effective First Aid and CPR training. This reference manual is to be used with the “hands- on” approach to our interactive training. Please enjoy your program. Learning objectives include clearly determining when to call 9-1-1 and what to do while waiting for help to arrive. Being confident in FIRST AID & CPR includes your ability to assess quickly and competently the components of an emergency situation. As a First Aider you will always follow the steps of Emergency Scene Management (ESM) by completing the Lifesaver 101 Rules of 123 & ABC and providing ongoing care. Any scene of a medical emergency can be overwhelming for a first aider. By taking a first aid course you are equipping yourself with the knowledge you will need to become and effective and confident first aider. -

Clinical Toxicology J.A
Postgrad Med J: first published as 10.1136/pgmj.69.807.19 on 1 January 1993. Downloaded from Postgrad Med J (1993) 69, 19 - 32 A) The Fellowship of Postgraduate Medicine, 1993 Reviews in Medicine Clinical toxicology J.A. Vale Director, National Poisons Information Service (Birmingham Centre), West Midlands Poisons Unit and Pesticide Monitoring Unit, Dudley Road Hospital, Birmingham B18 7QH, UK Introduction Selfpoisoning is the second most common cause of Much of the relevant literature relates to studies in acute medical presentation to hospital in the UK. volunteers given either a non-toxic marker or a However, as a result ofchanges over the last decade non-toxic dose ofa drug. As a result, the extrapola- both in the amount and type of agent ingested, the tion of many of these data to the poisoned patient majority of patients now suffer little if any adverse cannot be done with confidence. consequence and so require no active medical intervention. Nonetheless, a substantial minority Gastric lavage ofpoisoned patients do still require skilled medical management, often using the facilities of an inten- Although 'the idea of washing out the stomach sive care unit, if they are to survive without any with a syringe and tube, in cases where large important sequelae. Supportive therapy, including quantities oflaudanum and other poisons had been the correction of metabolic abnormalities, is of swallowed,' was first reported by Physick' in 1812 paramount importance in the care of such severely the value of gastric lavage remains controversial. by copyright. poisoned patients and this approach alone has Lavage performed 60 minutes after a therapeutic reduced the mortality significantly. -

Abc of Learning and Teaching in Medicine
AABBCC OFOF LEARNINGLEARNING ANDAND TEACHINGTEACHING ININ MEDICINEMEDICINE Edited by Peter Cantillon, Linda Hutchinson and Diana Wood ABC OF LEARNING AND TEACHING IN MEDICINE ABC OF LEARNING AND TEACHING IN MEDICINE Edited by PETER CANTILLON Senior lecturer in medical informatics and medical education, National University of Ireland, Galway, Republic of Ireland LINDA HUTCHINSON Director of education and workforce development and consultant paediatrician, University Hospital Lewisham and DIANA WOOD Director of medical education, University of Cambridge School of Clinical Medicine, Addenbrookes Hospital, Cambridge © 2003 BMJ Publishing Group All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording and/or otherwise, without the prior written permission of the publishers. First published in 2003 by BMJ Publishing Group Ltd, BMA House, Tavistock Square, London WC1H 9JR www.bmjbooks.com British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library ISBN 07279 16785 Typeset by BMJ Electronic Production Printed and bound in Spain by GraphyCems, Navarra Cover Image shows a stethoscope for listening to sounds within the body. With permission from Colin Cuthbert/Science Photo Library Contents Contributors vi Preface vii 1 Applying educational theory in practice 1 David M Kaufman 2 Curriculum design 5 David Prideaux 3 Problem based learning 8 Diana Wood 4 Evaluation -

The Efficiency of Bag-Valve Mask Ventilations by Medical First Responders and Basic Emergency Medical Technicians
California State University, San Bernardino CSUSB ScholarWorks Theses Digitization Project John M. Pfau Library 2003 The efficiency of bag-valve mask ventilations by medical first responders and basic emergency medical technicians John Vincent Commander Follow this and additional works at: https://scholarworks.lib.csusb.edu/etd-project Part of the Vocational Education Commons Recommended Citation Commander, John Vincent, "The efficiency of bag-valve mask ventilations by medical first responders and basic emergency medical technicians" (2003). Theses Digitization Project. 2310. https://scholarworks.lib.csusb.edu/etd-project/2310 This Project is brought to you for free and open access by the John M. Pfau Library at CSUSB ScholarWorks. It has been accepted for inclusion in Theses Digitization Project by an authorized administrator of CSUSB ScholarWorks. For more information, please contact [email protected]. THE EFFICIENCY OF BAG-VALVE MASK VENTILATIONS BY MEDICAL FIRST RESPONDERS AND BASIC EMERGENCY MEDICAL TECHNICIANS A Project Presented to the Faculty of California State University, San Bernardino In Partial Fulfillment of the Requirements for the Degree Master of Arts in Education: Career and Technical Education by John Vincent Commander September 2003 THE EFFICIENCY OF BAG-VALVE MASK VENTILATIONS BY MEDICAL FIRST RESPONDERS AND BASIC EMERGENCY MEDICAL TECHNICIANS A Project Presented to the Faculty of California State University, San Bernardino by John Vincent Commander September 2003 Approved by: © 2003 John Vincent Commander ABSTRACT• Bag-valve mask (BVM) ventilation maintains a patient's oxygenation and ventilation until a more definitive artificial airway can be established. In the prehospital setting of a traffic collision-or • medical aid scene this is performed by an Emergency Medical Technician or medical first responder.