FY 2015 Botswana Country Operational Plan (COP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LIST of LAW FIRMS NAME of FIRM ADDRESS TEL # FAX # Ajayi Legal
THE LAW SOCIETY OF BOTSWANA - LIST OF LAW FIRMS NAME OF FIRM ADDRESS TEL # FAX # Ajayi Legal Chambers P.O.Box 228, Sebele 3111321 Ajayi Legal Chambers P.O.Box 10220, Selebi Phikwe 2622441 2622442 Ajayi Legal Chambers P.O.Box 449, Letlhakane 2976784 2976785 Akheel Jinabhai & Associates P.O.Box 20575, Gaborone 3906636/3903906 3906642 Akoonyatse Law Firm P.O. Box 25058, Gaborone 3937360 3937350 Antonio & Partners Legal Practice P.O.Box HA 16 HAK, Maun 6864475 6864475 Armstrong Attorneys P.O.Box 1368, Gaborone 3953481 3952757 Badasu & Associates P.O.Box 80274, Gaborone 3700297 3700297 Banyatsi Mmekwa Attorneys P.O.Box 2278 ADD Poso House, Gaborone 3906450/2 3906449 Baoleki Attorneys P.O.Box 45111 Riverwalk, Gaborone 3924775 3924779 Bayford & Botha Attorneys P.O.Box 390, Lobatse 5301369 5301370 B. Maripe & Company P.O.Box 1425, Gaborone 3903258 3181719 B.K.Mmolawa Attorneys P.O.Box 30750, Francistown 2415944 2415943 Bayford & Associates P.O.Box 202283, Gaborone 3956877 3956886 Begane & Associates P.O. Box 60230, Gaborone 3191078 Benito Acolatse Attorneys P.O.Box 1157, Gaborone 3956454 3956447 Bernard Bolele Attorneys P.O.Box 47048, Gaborone 3959111 3951636 Biki & Associates P.O.Box AD 137ABE, Gaborone 3952559 Bogopa Manewe & Tobedza Attorneys P.O.Box 26465, Gaborone 3905466 3905451 Bonner Attorneys Bookbinder Business Law P/Bag 382, Gaborone 3912397 3912395 Briscoe Attorneys P.O.Box 402492, Gaborone 3953377 3904809 Britz Attorneys 3957524 3957062 Callender Attorneys P.O.Box 1354, Francistown 2441418 2446886 Charles Tlagae Attorneys P.O.Box -

HIV/AIDS Beh Dukw Haviour Wi Refug Ral Surv Gee Cam Veillanc
HIV/AIDS Behavioural Surveillance Survey (BSS) Dukwi Refugee Camp, Botswana May 2013 UNHCR & Botswana Ministry of Health 1 Acknowledgements The 2012 Botswana Behavioural Surveillance Survey (BSS) was a joint effort of UNHCR and the Botswana Ministry of Health, with funding from UNAIDS and WHO, and the support of Botswana Red Cross Society. The BSS was initiated and coordinated by Ms. Marian Schilperoord of UNHCR Geneva, and Dr. Njogu Patterson of UNHCR Pretoria, whose depth of experience overseeing similar surveys was incredibly valuable. Dr. Emmanuel Baingana of UNAIDS and Dr. Eugene Nyarko of WHO lent invaluable advice and support during critical phases of the project, and we are exceptionally grateful. The investigation team was led by the Principal Investigator Ms. Aimee Rose who managed the adaptation of the protocol and tools, field work, analysis and reporting. Dr. Marina Anderson, Co‐ Principal Investigator from the Ministry of Health, provided excellent technical oversight and coordination with the Ministry of Health. Three Investigators from the Ministry of Health, Ms. Lumba Nchunga, Ms. Betty Orapeleng and Ms. Bene Ntwayagae, provided input in each phase of the survey, from protocol development, pre‐planning missions to Dukwi Camp, monitoring of training and field work, and report compilation. The team benefitted from the dedicated support of UNHCR Country Representative Lynn Ngugi. We give special appreciation to UNHCR Program Officer Galefele Beleme for her tireless work on recruiting, finance, and logistics, and numerous other issues. UNHCR Head of Field Office Jane Okello facilitated the survey’s success at Dukwi Camp, with superb assistance from UNHCR staff Niroj Shrestha, Gracias Atwine, and Onkemetse Leburu. -

Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM
Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 1 Table 1: Overview Executive Summary None uploaded. Country Program Strategic Overview Will you be submitting changes to your country's 5-Year Strategy this year? If so, please briefly describe the changes you will be submitting. X Yes No Description: test Ambassador Letter File Name Content Type Date Uploaded Description Uploaded By Letter from Ambassador application/pdf 11/14/2008 TSukalac Nolan.pdf Country Contacts Contact Type First Name Last Name Title Email PEPFAR Coordinator Thierry Roels Associate Director GAP-Botswana [email protected] DOD In-Country Contact Chris Wyatt Chief, Office of Security [email protected] Cooperation HHS/CDC In-Country Contact Thierry Roels Associate Director GAP-Botswana [email protected] Peace Corps In-Country Peggy McClure Director [email protected] Contact USAID In-Country Contact Joan LaRosa USAID Director [email protected] U.S. Embassy In-Country Phillip Druin DCM [email protected] Contact Global Fund In-Country Batho C Molomo Coordinator of NACA [email protected] Representative Global Fund What is the planned funding for Global Fund Technical Assistance in FY 2009? $0 Does the USG assist GFATM proposal writing? Yes Does the USG participate on the CCM? Yes Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 2 Table 2: Prevention, Care, and Treatment Targets 2.1 Targets for Reporting Period Ending September 30, 2009 National 2-7-10 USG USG Upstream USG Total Target Downstream (Indirect) -
Botswana COVID-19 Guideline 5: Quarantine and Isolation
Botswana COVID-19 Guideline 5: Quarantine and Isolation Version: 1.0 5th May 2020 Table of Contents FOREWORD ............................................................................. Error! Bookmark not defined. ACKNOWLEDGEMENTS ................................................................................................... 3 DEFINITION OF TERMS .................................................................................................. 5 ABBREVIATIONS AND ACRONYMS .............................................................................. 6 SCOPE OF THE DOCUMENT ............................................................................................ 7 CASE DEFINITIONS ......................................................................................................... 8 PRINCIPLES OF QUARANTINE...................................................................................... 9 INSTITUTIONAL QUARANTINE .................................................................................. 11 HOME QUARANTINE ...................................................................................................... 14 PRINCIPLES OF ISOLATION........................................................................................ 15 FACILITY ISOLATION OF COVID-19 CASES ............................................................ 16 HOME ISOLATION OF COVID-19 CASES ................................................................... 17 APPENDICES .................................................................................................................. -

Bank of Botswana
PAPER 4 BANK OF BOTSWANA DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA AS AT DECEMBER 31, 2009 PREPARED AND DISTRIBUTED BY THE BANKING SUPERVISION DEPARTMENT BANK OF BOTSWANA Foreword This directory is compiled and distributed by the Banking Supervision Department of the Bank of Botswana. While every effort has been made to ensure the accuracy of the information contained in this directory, such information is subject to frequent revision, and thus the Bank accepts no responsibility for the continuing accuracy of the information. Interested parties are advised to contact the respective financial institutions directly for any information they require. This directory excludes Collective Investment Undertakings and International Financial Services Centre non-bank entities, whose regulation and supervision have been transferred to the Non-Bank Financial Institutions Regulatory Authority. Oabile Mabusa DIRECTOR BANKING SUPERVISION DEPARTMENT 1 DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA TABLE OF CONTENTS 1. CENTRAL BANK ............................................................................................................................................. 4 2. COMMERCIAL BANKS ................................................................................................................................... 6 2.1 ABN AMRO BANK (B OTSWANA ) LIMITED ..................................................................................................... 6 2.2 ABN AMRO BANK (B OTSWANA ) OBU LIMITED ........................................................................................... -

Land Tenure Reforms and Social Transformation in Botswana: Implications for Urbanization
Land Tenure Reforms and Social Transformation in Botswana: Implications for Urbanization. Item Type text; Electronic Dissertation Authors Ijagbemi, Bayo, 1963- Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 06/10/2021 17:13:55 Link to Item http://hdl.handle.net/10150/196133 LAND TENURE REFORMS AND SOCIAL TRANSFORMATION IN BOTSWANA: IMPLICATIONS FOR URBANIZATION by Bayo Ijagbemi ____________________ Copyright © Bayo Ijagbemi 2006 A Dissertation Submitted to the Faculty of the DEPARTMENT OF ANTHROPOLOGY In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY In the Graduate College THE UNIVERSITY OF ARIZONA 2006 2 THE UNIVERSITY OF ARIZONA GRADUATE COLLEGE As members of the Dissertation Committee, we certify that we have read the dissertation prepared by Bayo Ijagbemi entitled “Land Reforms and Social Transformation in Botswana: Implications for Urbanization” and recommend that it be accepted as fulfilling the dissertation requirement for the Degree of Doctor of Philosophy _______________________________________________________________________ Date: 10 November 2006 Dr Thomas Park _______________________________________________________________________ Date: 10 November 2006 Dr Stephen Lansing _______________________________________________________________________ Date: 10 November 2006 Dr David Killick _______________________________________________________________________ Date: 10 November 2006 Dr Mamadou Baro Final approval and acceptance of this dissertation is contingent upon the candidate’s submission of the final copies of the dissertation to the Graduate College. I hereby certify that I have read this dissertation prepared under my direction and recommend that it be accepted as fulfilling the dissertation requirement. -

Department of Road Transport and Safety Offices
DEPARTMENT OF ROAD TRANSPORT AND SAFETY OFFICES AND SERVICES MOLEPOLOLE • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate Tel: 5920148 Fax: 5910620 P/Bag 52 Molepolole Next to Molepolole Police MOCHUDI • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate P/Bag 36 Mochudi Tel : 5777127 Fax : 5748542 White House GABORONE Headquarters BBS Mall Plot no 53796 Tshomarelo House (Botswana Savings Bank) 1st, 2nd &3rd Floor Corner Lekgarapa/Letswai Road •Registration & Licensing of vehicles and drivers •Road safety (Public Education) Tel: 3688600/62 Fax : Fax: 3904067 P/Bag 0054 Gaborone GABORONE VTS – MARUAPULA • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Vehicle Examination Tel: 3912674/2259 P/Bag BR 318 B/Hurst Near Roads Training & Roads Maintenance behind Maruapula Flats GABORONE II – FAIRGROUNDS • Registration & Licensing of vehicles and drivers • Driver Examination : Theory Tel: 3190214/3911540/3911994 Fax : P/Bag 0054 Gaborone GABORONE - OLD SUPPLIES • Registration & Licensing of vehicles and drivers • Transport Permits • Transport Inspectorate Tel: 3905050 Fax :3932671 P/Bag 0054 Gaborone Plot 1221, Along Nkrumah Road, Near Botswana Power Corporation CHILDREN TRAFFIC SCHOOL •Road Safety Promotion for children only Tel: 3161851 P/Bag BR 318 B/Hurst RAMOTSWA •Registration & Licensing of vehicles and drivers •Driver Examination (Theory & Practical -

The Big Governance Issues in Botswana
MARCH 2021 THE BIG GOVERNANCE ISSUES IN BOTSWANA A CIVIL SOCIETY SUBMISSION TO THE AFRICAN PEER REVIEW MECHANISM Contents Executive Summary 3 Acknowledgments 7 Acronyms and Abbreviations 8 What is the APRM? 10 The BAPS Process 12 Ibrahim Index of African Governance Botswana: 2020 IIAG Scores, Ranks & Trends 120 CHAPTER 1 15 Introduction CHAPTER 2 16 Human Rights CHAPTER 3 27 Separation of Powers CHAPTER 4 35 Public Service and Decentralisation CHAPTER 5 43 Citizen Participation and Economic Inclusion CHAPTER 6 51 Transparency and Accountability CHAPTER 7 61 Vulnerable Groups CHAPTER 8 70 Education CHAPTER 9 80 Sustainable Development and Natural Resource Management, Access to Land and Infrastructure CHAPTER 10 91 Food Security CHAPTER 11 98 Crime and Security CHAPTER 12 108 Foreign Policy CHAPTER 13 113 Research and Development THE BIG GOVERNANCE ISSUES IN BOTSWANA: A CIVIL SOCIETY SUBMISSION TO THE APRM 3 Executive Summary Botswana’s civil society APRM Working Group has identified 12 governance issues to be included in this submission: 1 Human Rights The implementation of domestic and international legislation has meant that basic human rights are well protected in Botswana. However, these rights are not enjoyed equally by all. Areas of concern include violence against women and children; discrimination against indigenous peoples; child labour; over reliance on and abuses by the mining sector; respect for diversity and culture; effectiveness of social protection programmes; and access to quality healthcare services. It is recommended that government develop a comprehensive national action plan on human rights that applies to both state and business. 2 Separation of Powers Political and personal interests have made separation between Botswana’s three arms of government difficult. -

Botswana Semiology Research Centre Project Seismic Stations In
BOTSWANA SEISMOLOGICAL NETWORK ( BSN) STATIONS 19°0'0"E 20°0'0"E 21°0'0"E 22°0'0"E 23°0'0"E 24°0'0"E 25°0'0"E 26°0'0"E 27°0'0"E 28°0'0"E 29°0'0"E 30°0'0"E 1 S 7 " ° 0 0 ' ' 0 0 ° " 7 S 1 KSANE Kasane ! !Kazungula Kasane Forest ReserveLeshomo 1 S Ngoma Bridge ! 8 " ! ° 0 0 ' # !Mabele * . MasuzweSatau ! ! ' 0 ! ! Litaba 0 ° Liamb!ezi Xamshiko Musukub!ili Ivuvwe " 8 ! ! ! !Seriba Kasane Forest Reserve Extension S 1 !Shishikola Siabisso ! ! Ka!taba Safari Camp ! Kachikau ! ! ! ! ! ! Chobe Forest Reserve ! !! ! Karee ! ! ! ! ! Safari Camp Dibejam!a ! ! !! ! ! ! ! X!!AUD! M Kazuma Forest Reserve ! ShongoshongoDugamchaRwelyeHau!xa Marunga Xhauga Safari Camp ! !SLIND Chobe National Park ! Kudixama Diniva Xumoxu Xanekwa Savute ! Mah!orameno! ! ! ! Safari Camp ! Maikaelelo Foreset Reserve Do!betsha ! ! Dibebe Tjiponga Ncamaser!e Hamandozi ! Quecha ! Duma BTLPN ! #Kwiima XanekobaSepupa Khw!a CHOBE DISTRICT *! !! ! Manga !! Mampi ! ! ! Kangara # ! * Gunitsuga!Njova Wazemi ! ! G!unitsuga ! Wazemi !Seronga! !Kaborothoa ! 1 S Sibuyu Forest Reserve 9 " Njou # ° 0 * ! 0 ' !Nxaunxau Esha 12 ' 0 Zara ! ! 0 ° ! ! ! " 9 ! S 1 ! Mababe Quru!be ! ! Esha 1GMARE Xorotsaa ! Gumare ! ! Thale CheracherahaQNGWA ! ! GcangwaKaruwe Danega ! ! Gqose ! DobeQabi *# ! ! ! ! Bate !Mahito Qubi !Mahopa ! Nokaneng # ! Mochabana Shukumukwa * ! ! Nxabe NGAMILAND DISTRICT Sorob!e ! XurueeHabu Sakapane Nxai National Nark !! ! Sepako Caecae 2 ! ! S 0 " Konde Ncwima ° 0 ! MAUN 0 ' ! ! ' 0 Ntabi Tshokatshaa ! 0 ° ! " 0 PHDHD Maposa Mmanxotai S Kaore ! ! Maitengwe 2 ! Tsau Segoro -
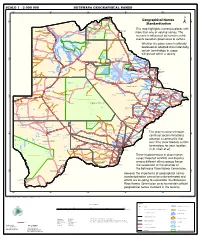
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe -

List of Schools Visited for Monitoring Visits
LIST OF SCHOOLS VISITED FOR MONITORING VISITS CENTRAL INSPECTORAL AREA LOCATION NAME OF SCHOOL MMADINARE Diloro Diloro MMADINARE Mmadinare Kelele MMADINARE Kgagodi Kgagodi MMADINARE Mmadinare Mmadinare MMADINARE Mmadinare Phethu Mphoeng MMADINARE Robelela Robelela MMADINARE Gojwane Sedibe MMADINARE Serule Serule MMADINARE Mmadinare Tlapalakoma BOTETI Rakops Etsile BOTETI Khumaga Khumaga BOTETI Khwee Khwee BOTETI Mopipi Manthabakwe BOTETI Mmadikola Mmadikola BOTETI Letlhakane Mokane BOTETI Mokoboxane Mokoboxane BOTETI Mokubilo Mokubilo BOTETI Moreomaoto Moreomaoto BOTETI Mosu Mosu BOTETI Motlopi Motlopi BOTETI Letlhakane Retlhatloleng Selibe Phikwe Selibe Phikwe Boitshoko Selibe Phikwe Selibe Phikwe Boswelakgomo Selibe Phikwe Selibe Phikwe Phikwe Selibe Phikwe Selibe Phikwe Tebogo BOBIRWA Bobonong Bobonong BOBIRWA Gobojango Gobojango BOBIRWA Bobonong Mabumahibidu BOBIRWA Bobonong Madikwe BOBIRWA Mogapi Mogapi BOBIRWA Molalatau Molalatau BOBIRWA Bobonong Rasetimela BOBIRWA Semolale Semolale BOBIRWA Tsetsebye Tsetsebye 1 | P a g e MAHALAPYE WEST Bonwapitse Bonwapitse MAHALAPYE WEST Mahalapye Leetile MAHALAPYE WEST Mokgenene Mokgenene MAHALAPYE WEST Moralane Moralane MAHALAPYE WEST Mosolotshane Mosolotshane MAHALAPYE WEST Otse Setlhamo MAHALAPYE WEST Mahalapye St James MAHALAPYE WEST Mahalapye Tshikinyega MHALAPYE EAST Mahalapye Flowertown MHALAPYE EAST Mahalapye Mahalapye MHALAPYE EAST Matlhako Matlhako MHALAPYE EAST Mmaphashalala Mmaphashalala MHALAPYE EAST Sefhare Mmutle PALAPYE NORTH Goo-Sekgweng Goo-Sekgweng PALAPYE NORTH Goo-Tau Goo-Tau -

SABONET Report No 18
ii Quick Guide This book is divided into two sections: the first part provides descriptions of some common trees and shrubs of Botswana, and the second is the complete checklist. The scientific names of the families, genera, and species are arranged alphabetically. Vernacular names are also arranged alphabetically, starting with Setswana and followed by English. Setswana names are separated by a semi-colon from English names. A glossary at the end of the book defines botanical terms used in the text. Species that are listed in the Red Data List for Botswana are indicated by an ® preceding the name. The letters N, SW, and SE indicate the distribution of the species within Botswana according to the Flora zambesiaca geographical regions. Flora zambesiaca regions used in the checklist. Administrative District FZ geographical region Central District SE & N Chobe District N Ghanzi District SW Kgalagadi District SW Kgatleng District SE Kweneng District SW & SE Ngamiland District N North East District N South East District SE Southern District SW & SE N CHOBE DISTRICT NGAMILAND DISTRICT ZIMBABWE NAMIBIA NORTH EAST DISTRICT CENTRAL DISTRICT GHANZI DISTRICT KWENENG DISTRICT KGATLENG KGALAGADI DISTRICT DISTRICT SOUTHERN SOUTH EAST DISTRICT DISTRICT SOUTH AFRICA 0 Kilometres 400 i ii Trees of Botswana: names and distribution Moffat P. Setshogo & Fanie Venter iii Recommended citation format SETSHOGO, M.P. & VENTER, F. 2003. Trees of Botswana: names and distribution. Southern African Botanical Diversity Network Report No. 18. Pretoria. Produced by University of Botswana Herbarium Private Bag UB00704 Gaborone Tel: (267) 355 2602 Fax: (267) 318 5097 E-mail: [email protected] Published by Southern African Botanical Diversity Network (SABONET), c/o National Botanical Institute, Private Bag X101, 0001 Pretoria and University of Botswana Herbarium, Private Bag UB00704, Gaborone.