BOTSWANA Country Operational Plan 2016 Strategic Direction Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Working Paper CBMS-2020-09
working paper CBMS-2020-09 Sustainable Development Goals, Botswana: A Case Study of Gabane Village in Kweneng District Happy Siphambe Malebogo Bakwena Lexi Setlhare Mavis Kolobe Itumeleng Oageng Keamogetse Setlhare Tshegofatso Motswagae May 2020 Sustainable Development Goals, Botswana: A Case Study of Gabane Village in Kweneng District Abstract The main objective of the research paper was to use the Community Based Monitoring System (CBMS) methodology to determine progress on achievement of Sustainable Development Goals (SDGs) with a view of localising SDGs to Gabane village. Generally, the results reveal that poverty is prevalent amongst women, youth and children. Specifically, the working poor constitute 40.8% of the people leaving below the poverty line. Noteworthy, is that 50% of children under 5 years of age have no access to pre-primary education. Gabane residents are reluctant to participate in poverty-targeted government programmes as evidenced by a low participation rate. Last but not least, the results show a higher unemployment rate of 23.3 %( ILO or narrow definition) and 29.44% (broad definition) in Gabane. The majority of the unemployed were youth and women. The policy implications of the results are that the government of Botswana should review the current minimum wage legislation to ensure that the minimum wage is aligned to the cost of living so as to ensure decent wages. Finally, in order to ensure that early childhood is rolled out for all under 5s, the government should expedite the implementation of the Education and Training Strategy Sector Plan (ETSSP) of 2015-2020. JEL: I32, I33, J88 Keywords: Poverty analysis, poverty, welfare and wellbeing. -

Malejane Unpublished (MSW) 2017
Faculty of Social Sciences School of Graduate Studies Department of Social Work Masters of social work (Social Policy and Administration) Topic: Assessing the Perceptions of the Beneficiaries of the Presidential Housing Appeal in Botswana: A Case Study of Gabane Village By; Mr Aobakwe Bacos Malejane ID Number; 201103575 A Dissertation Submitted in Partial Fulfilment of the Requirements for the Award of a Master’s Degree in Social Work (Social Policy and Administration) Assessing the Perceptions of the Beneficiaries of the Presidential Housing Appeal in Botswana: A Case Study of Gabane Village By Mr Aobakwe Bacos Malejane Student Number; 201103575 A Dissertation Submitted in Partial Fulfilment of the Requirements for the Award of a Master’s Degree in Social Work (Social Policy and Administration) SUPERVISED BY; Dr. O. Jankey Prof. L.K. Mwansa STATEMENT OF ORIGINALITY This dissertation was undertaken from August 2016 to May 2017. The contents of the dissertation are the original work of the student except where reference have been made. __________________________ _________________________ Student’s signature Date DEDICATION This dissertation is dedicated to Mr. Mahia Ooke, Mrs. Gakedumele Tshimong Ooke, Mr. Thomas Malejane and Mrs. Ntlhabololang Malejane who are a true inspiration in my quest of being a humanitarian through their selfless and compassion in promotion of lives of those less fortunate in remote areas. ACKNOWLEDGEMENTS For this master piece to be complete, I would like to express my sincere gratitude to my research supervisor Dr. O. Jankey and Prof. L. K. Mwansa for the continuous support of my master’s degree study and research, for their patience, motivation, enthusiasm, and immense knowledge. -

LIST of LAW FIRMS NAME of FIRM ADDRESS TEL # FAX # Ajayi Legal
THE LAW SOCIETY OF BOTSWANA - LIST OF LAW FIRMS NAME OF FIRM ADDRESS TEL # FAX # Ajayi Legal Chambers P.O.Box 228, Sebele 3111321 Ajayi Legal Chambers P.O.Box 10220, Selebi Phikwe 2622441 2622442 Ajayi Legal Chambers P.O.Box 449, Letlhakane 2976784 2976785 Akheel Jinabhai & Associates P.O.Box 20575, Gaborone 3906636/3903906 3906642 Akoonyatse Law Firm P.O. Box 25058, Gaborone 3937360 3937350 Antonio & Partners Legal Practice P.O.Box HA 16 HAK, Maun 6864475 6864475 Armstrong Attorneys P.O.Box 1368, Gaborone 3953481 3952757 Badasu & Associates P.O.Box 80274, Gaborone 3700297 3700297 Banyatsi Mmekwa Attorneys P.O.Box 2278 ADD Poso House, Gaborone 3906450/2 3906449 Baoleki Attorneys P.O.Box 45111 Riverwalk, Gaborone 3924775 3924779 Bayford & Botha Attorneys P.O.Box 390, Lobatse 5301369 5301370 B. Maripe & Company P.O.Box 1425, Gaborone 3903258 3181719 B.K.Mmolawa Attorneys P.O.Box 30750, Francistown 2415944 2415943 Bayford & Associates P.O.Box 202283, Gaborone 3956877 3956886 Begane & Associates P.O. Box 60230, Gaborone 3191078 Benito Acolatse Attorneys P.O.Box 1157, Gaborone 3956454 3956447 Bernard Bolele Attorneys P.O.Box 47048, Gaborone 3959111 3951636 Biki & Associates P.O.Box AD 137ABE, Gaborone 3952559 Bogopa Manewe & Tobedza Attorneys P.O.Box 26465, Gaborone 3905466 3905451 Bonner Attorneys Bookbinder Business Law P/Bag 382, Gaborone 3912397 3912395 Briscoe Attorneys P.O.Box 402492, Gaborone 3953377 3904809 Britz Attorneys 3957524 3957062 Callender Attorneys P.O.Box 1354, Francistown 2441418 2446886 Charles Tlagae Attorneys P.O.Box -

2011 Population and Housing Census
2011 POPULATION AND HOUSING CENSUS Ministry of Finance and Development Planning 2011 Census Slogan: Palo yame, tsela ya ditlhabololo My count, a guide to developments August 2009 CSO in Collaboration with UNFPA PROJECT DOCUMENT 2011 POPULATION AND HOUSING CENSUS Published by Central Statistics Office Private Bag 0024, Gaborone Telephone: 33671300 Fax: 3952201 E-mail:[email protected] Website: www.cso.gov.bw Contact Unit : Census Secretariat Telephone: 3671300 Ext. 1305 August 2009 COPYRIGHT RESERVED Extracts may be published if source is duly acknowledged i CONTENTS PREFACE .................................................................................................................... 1 LIST OF ABBREVIATIONS AND ACRONYMS ....................................................... 2 EXECUTIVE SUMMARY ........................................................................................... 4 1. BACKGROUND AND JUSTIFICATION ................................................................ 5 1.1 Background of the 2011 Census Taking .............................................................. 5 1.2 Justification ......................................................................................................... 5 1.2.1 Evidence-based decision making, policy-making, planning and administration ....................................................................................................... 5 1.2.2 Research .................................................................................................... 5 1.2.3 Service to stakeholders -

HIV/AIDS Beh Dukw Haviour Wi Refug Ral Surv Gee Cam Veillanc
HIV/AIDS Behavioural Surveillance Survey (BSS) Dukwi Refugee Camp, Botswana May 2013 UNHCR & Botswana Ministry of Health 1 Acknowledgements The 2012 Botswana Behavioural Surveillance Survey (BSS) was a joint effort of UNHCR and the Botswana Ministry of Health, with funding from UNAIDS and WHO, and the support of Botswana Red Cross Society. The BSS was initiated and coordinated by Ms. Marian Schilperoord of UNHCR Geneva, and Dr. Njogu Patterson of UNHCR Pretoria, whose depth of experience overseeing similar surveys was incredibly valuable. Dr. Emmanuel Baingana of UNAIDS and Dr. Eugene Nyarko of WHO lent invaluable advice and support during critical phases of the project, and we are exceptionally grateful. The investigation team was led by the Principal Investigator Ms. Aimee Rose who managed the adaptation of the protocol and tools, field work, analysis and reporting. Dr. Marina Anderson, Co‐ Principal Investigator from the Ministry of Health, provided excellent technical oversight and coordination with the Ministry of Health. Three Investigators from the Ministry of Health, Ms. Lumba Nchunga, Ms. Betty Orapeleng and Ms. Bene Ntwayagae, provided input in each phase of the survey, from protocol development, pre‐planning missions to Dukwi Camp, monitoring of training and field work, and report compilation. The team benefitted from the dedicated support of UNHCR Country Representative Lynn Ngugi. We give special appreciation to UNHCR Program Officer Galefele Beleme for her tireless work on recruiting, finance, and logistics, and numerous other issues. UNHCR Head of Field Office Jane Okello facilitated the survey’s success at Dukwi Camp, with superb assistance from UNHCR staff Niroj Shrestha, Gracias Atwine, and Onkemetse Leburu. -

Botswana Environment Statistics Water Digest 2018
Botswana Environment Statistics Water Digest 2018 Private Bag 0024 Gaborone TOLL FREE NUMBER: 0800600200 Tel: ( +267) 367 1300 Fax: ( +267) 395 2201 E-mail: [email protected] Website: http://www.statsbots.org.bw Published by STATISTICS BOTSWANA Private Bag 0024, Gaborone Phone: 3671300 Fax: 3952201 Email: [email protected] Website: www.statsbots.org.bw Contact Unit: Environment Statistics Unit Phone: 367 1300 ISBN: 978-99968-482-3-0 (e-book) Copyright © Statistics Botswana 2020 No part of this information shall be reproduced, stored in a Retrieval system, or even transmitted in any form or by any means, whether electronically, mechanically, photocopying or otherwise, without the prior permission of Statistics Botswana. BOTSWANA ENVIRONMENT STATISTICS WATER DIGEST 2018 Statistics Botswana PREFACE This is Statistics Botswana’s annual Botswana Environment Statistics: Water Digest. It is the first solely water statistics annual digest. This Digest will provide data for use by decision-makers in water management and development and provide tools for the monitoring of trends in water statistics. The indicators in this report cover data on dam levels, water production, billed water consumption, non-revenue water, and water supplied to mines. It is envisaged that coverage of indicators will be expanded as more data becomes available. International standards and guidelines were followed in the compilation of this report. The United Nations Framework for the Development of Environment Statistics (UNFDES) and the United Nations International Recommendations for Water Statistics were particularly useful guidelines. The data collected herein will feed into the UN System of Environmental Economic Accounting (SEEA) for water and hence facilitate an informed management of water resources. -

Migrant Labour in the Bukalanga Area, 1934-1985: the Unfinished Story
Historia, 63, 1, May 2018, pp 130-149 Skills acquisition and investments by Batswana migrants from southern Botswana to South Africa, 1970–2010 Wazha G. Morapedi* Abstract This paper focuses on migrant labour from southern Botswana to South Africa. The main thrust of this article is its emphasis on the positive contribution of migration to the migrants and their communities. It is argued here that although migrant labour has been blamed for having negative socio-economic effects in southern Botswana, just as in other parts of the country, it also contributed, and continues to contribute positively to the wellbeing of some households and their communities at large. Through the use of case studies from different villages in the district, the article demonstrates that poor, uneducated and unskilled young men who migrated to South Africa managed to accumulate and invest in agriculture and commercial enterprises and rose up the social ladder. In this area, migrant wages were critical in forming the basis of some enterprises, several of which are still flourishing. It also argues that some migrants acquired on-the-job skills which were later utilised productively when the migrants returned to Botswana. A similar study, but one which did not emphasise the acquisition of skills was undertaken by the author in the Bukalanga region of north-eastern Botswana in 2004. Key Words: Botswana; South Africa; migration; agriculture; labourers. Opsomming Hierdie artikel fokus op trekarbeid van suidelike Botswana na Suid-Afrika. Die artikel poog om die positiewe bydrae wat migrasie vir migrante en hul gemeenskappe inhou, te beklemtoon. Ten spyte daarvan dat trekarbeid vir verskeie negatiewe sosio- ekonomiese uitwerkings in Botswana blameer is, word hier geargumenteer dat trekarbeid positief bydrae tot die welstand van sekere huishoudings en gemeenskappe in die breë. -

Ÿþm I C R O S O F T W O R
E WL E WL REGISTERED WITH THE DIRECTOR OF POSTS AND TELEGRAPHS AS A NEWSPAPER Volume V No. 7 Organ of the Botswana Democratic Party JULY, 1967. LOETO LA TONA YA 'TEMO MO dikgweding tse di fitileng Tona ya Temo, Morena Tsheko T~sheko o ne a tsamaya thata mo mafelong a mantsi a Botswana, go bona balemi le barua-kgomo le go bona ditiro tsa ba Lephata la Temo le ba Lephata la Leruo. Mo mafelong otihe o ne a ntse a buisanya le babusi le magosi le merafe mo kgotleng le balemi ba basweu le ba bantsho. Me go itumedisa thata go bolela gore mo mafelong otlhe a a a tsamaileng pula e nele sentle mabele a teng le phulo e ntsi. Tota mo mafelong a mangwe pula e nele go feta selekanyo mo ebileng e ntshofaditse mabele ya bodisa dinawa le dithotse. Puo e o neng a e bua le batho bogolo e ne e le ya go ba kgothatsa go lema thata go katolosa masimo le go a epa disana le gore batho ba dire mo masimong a bone ngwaga otlhe eseng go ntsha dijo mo masismo go tswa foo batho ba bo ba siela kwa magaeng a matona goya go nna ba sa dire sepe. 0 ne a tlhalosa ka gore Goromente o lemoga gore temo le leruo mo Bot.swana ke tsone tse di tshetsang batho ka go sena mekoti le ditiro. Me a bolela ka gore Goromente o aga sekwele se segolo kwa Gaborone se se tla rutang makau a Botswana temo le tlhokomelo ya leruo gore ba gasiwe le lefatshe la Botswana go ruta batho ka bontsi go lema mo go tla ba tswelang molemo. -

Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM
Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 1 Table 1: Overview Executive Summary None uploaded. Country Program Strategic Overview Will you be submitting changes to your country's 5-Year Strategy this year? If so, please briefly describe the changes you will be submitting. X Yes No Description: test Ambassador Letter File Name Content Type Date Uploaded Description Uploaded By Letter from Ambassador application/pdf 11/14/2008 TSukalac Nolan.pdf Country Contacts Contact Type First Name Last Name Title Email PEPFAR Coordinator Thierry Roels Associate Director GAP-Botswana [email protected] DOD In-Country Contact Chris Wyatt Chief, Office of Security [email protected] Cooperation HHS/CDC In-Country Contact Thierry Roels Associate Director GAP-Botswana [email protected] Peace Corps In-Country Peggy McClure Director [email protected] Contact USAID In-Country Contact Joan LaRosa USAID Director [email protected] U.S. Embassy In-Country Phillip Druin DCM [email protected] Contact Global Fund In-Country Batho C Molomo Coordinator of NACA [email protected] Representative Global Fund What is the planned funding for Global Fund Technical Assistance in FY 2009? $0 Does the USG assist GFATM proposal writing? Yes Does the USG participate on the CCM? Yes Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 2 Table 2: Prevention, Care, and Treatment Targets 2.1 Targets for Reporting Period Ending September 30, 2009 National 2-7-10 USG USG Upstream USG Total Target Downstream (Indirect) -
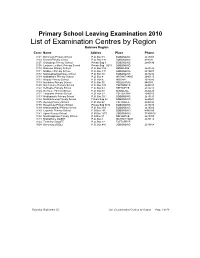
List of Examination Centres by Region Bobirwa Region Centr Name Addres Place Phone 0101 Bobonong Primary School P.O
Primary School Leaving Examination 2010 List of Examination Centres by Region Bobirwa Region Centr Name Addres Place Phone 0101 Bobonong Primary School P.O. Box 48 BOBONONG 2619207 0103 Borotsi Primary School P.O. Box 136 BOBONONG 819208 0107 Gobojango Primary School Private Bag 8 BOBONONG 2645436 0108 Lentswe-Le-Moriti Primary School Private Bag 0019 BOBONONG 0110 Mabolwe Primary School P.O. Box 182 SEMOLALE 2645422 0111 Madikwe Primary School P.O. Box 131 BOBONONG 2619221 0112 Mafetsakgang primary school P.O. Box 46 BOBONONG 2619232 0114 Mathathane Primary School P.O. Box 4 MATHATHANE 2645110 0117 Mogapi Primary School P.O. Box 6 MOGAPI 2618545 0119 Molalatau Primary School P.O. Box 50 MOLALATAU 845374 0120 Moletemane Primary School P.O. Box 176 TSETSEBYE 2646035 0123 Sefhophe Primary School P.O. Box 41 SEFHOPHE 2618210 0124 Semolale Primary School P.O. Box 10 SEMOLALE 2645422 0131 Tsetsejwe Primary School P.O. Box 33 TSETSEJWE 2646103 0133 Modisaotsile Primary School P.O. Box 591 BOBONONG 2619123 0134 Motlhabaneng Primary School Private Bag 20 BOBONONG 2645541 0135 Busang Primary School P.O. Box 47 TSETSEBJE 2646144 0138 Rasetimela Primary School Private Bag 0014 BOBONONG 2619485 0139 Mabumahibidu Primary School P.O. Box 168 BOBONONG 2619040 0140 Lepokole Primary School P O Box 148 BOBONONG 4900035 0141 Agosi Primary School P O Box 1673 BOBONONG 71868614 0142 Motsholapheko Primary School P O Box 37 SEFHOPHE 2618305 0143 Mathathane DOSET P.O. Box 4 MATHATHANE 2645110 0144 Tsetsebye DOSET P.O. Box 33 TSETSEBYE 3024 Bobonong DOSET P.O. Box 483 BOBONONG 2619164 Saturday, September 25, List of Examination Centres by Region Page 1 of 39 Boteti Region Centr Name Addres Place Phone 0201 Adult Education Private Bag 1 ORAPA 0202 Baipidi Primary School P.O. -

Botswana Country Report-Annex-4 4Th Interim Techical Report
PROMOTING PARTNERSHIPS FOR CRIMEPREVENTION BETWEEN THE STATE AND PRIVATE SECURITY PROVIDERS IN BOTSWANA BY MPHO MOLOMO AND ZIBANI MAUNDENI Introduction Botswana stands out as the only African country to have sustained an unbroken record of liberal democracy and political stability since independence. The country has been dubbed the ‘African Miracle’ (Thumberg Hartland, 1978; Samatar, 1999). It is widely regarded as a success story arising from its exploitation and utilisation of natural resources, establishing a strong state, institutional and administrative capacity, prudent macro-economic stability and strong political leadership. These attributes, together with the careful blending of traditional and modern institutions have afforded Botswana a rare opportunity of political stability in the Africa region characterised by political and social strife. The expectation is that the economic growth will bring about development and security. However, a critical analysis of Botswana’s development trajectory indicates that the country’s prosperity has it attendant problems of poverty, unemployment, inequalities and crime. Historically crime prevention was a preserve of the state using state security agencies as the police, military, prisons and other state apparatus, such as, the courts and laws. However, since the late 1980s with the expanded definition of security from the narrow static conception to include human security, it has become apparent that state agencies alone cannot combat the rising levels of crime. The police in recognising that alone they cannot cope with the crime levels have been innovative and embarked on other models of public policing, such as, community policing as a public society partnership to combat crime. To further cater for the huge demand on policing, other actors, which are non-state actors; in particular private security firms have come in, especially in the urban market and occupy a special niche to provide a service to those who can afford to pay for it. -

The Parliamentary Constituency Offices
REPUBLIC OF BOTSWANA THE PARLIAMENTARY CONSTITUENCY OFFICES Parliament of Botswana P O Box 240 Gaborone Tel: 3616800 Fax: 3913103 Toll Free; 0800 600 927 e - mail: [email protected] www.parliament.gov.bw Introduction Mmathethe-Molapowabojang Mochudi East Mochudi West P O Box 101 Mmathethe P O Box 2397 Mochudi P O Box 201951 Ntshinoge Representative democracy can only function effectively if the Members of Tel: 5400251 Fax: 5400080 Tel: 5749411 Fax: 5749989 Tel: 5777084 Fax: 57777943 Parliament are accessible, responsive and accountable to their constituents. Mogoditshane Molepolole North Molepolole South The mandate of a Constituency Office is to act as an extension of Parliament P/Bag 008 Mogoditshane P O Box 449 Molepolole P O Box 3573 Molepolole at constituency level. They exist to play this very important role of bringing Tel: 3915826 Fax: 3165803 Tel: 5921099 Fax: 5920074 Tel: 3931785 Fax: 3931785 Parliament and Members of Parliament close to the communities they serve. Moshupa-Manyana Nata-Gweta Ngami A constituency office is a Parliamentary office located at the headquarters of P O Box 1105 Moshupa P/Bag 27 Sowa Town P/Bag 2 Sehithwa Tel: 5448140 Fax: 5448139 Tel: 6213756 Fax: 6213240 Tel: 6872105/123 each constituency for use by a Member of Parliament (MP) to carry out his or Fax: 6872106 her Parliamentary work in the constituency. It is a formal and politically neutral Nkange Okavango Palapye place where a Member of Parliament and constituents can meet and discuss P/Bag 3 Tutume P O Box 69 Shakawe P O Box 10582 Palapye developmental issues. Tel: 2987717 Fax: 2987293 Tel: 6875257/230 Tel: 4923475 Fax: 4924231 Fax: 6875258 The offices must be treated strictly as Parliamentary offices and must therefore Ramotswa Sefhare-Ramokgonami Selibe Phikwe East be used for Parliamentary business and not political party business.