Botswana COVID-19 Guideline 5: Quarantine and Isolation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LIST of LAW FIRMS NAME of FIRM ADDRESS TEL # FAX # Ajayi Legal
THE LAW SOCIETY OF BOTSWANA - LIST OF LAW FIRMS NAME OF FIRM ADDRESS TEL # FAX # Ajayi Legal Chambers P.O.Box 228, Sebele 3111321 Ajayi Legal Chambers P.O.Box 10220, Selebi Phikwe 2622441 2622442 Ajayi Legal Chambers P.O.Box 449, Letlhakane 2976784 2976785 Akheel Jinabhai & Associates P.O.Box 20575, Gaborone 3906636/3903906 3906642 Akoonyatse Law Firm P.O. Box 25058, Gaborone 3937360 3937350 Antonio & Partners Legal Practice P.O.Box HA 16 HAK, Maun 6864475 6864475 Armstrong Attorneys P.O.Box 1368, Gaborone 3953481 3952757 Badasu & Associates P.O.Box 80274, Gaborone 3700297 3700297 Banyatsi Mmekwa Attorneys P.O.Box 2278 ADD Poso House, Gaborone 3906450/2 3906449 Baoleki Attorneys P.O.Box 45111 Riverwalk, Gaborone 3924775 3924779 Bayford & Botha Attorneys P.O.Box 390, Lobatse 5301369 5301370 B. Maripe & Company P.O.Box 1425, Gaborone 3903258 3181719 B.K.Mmolawa Attorneys P.O.Box 30750, Francistown 2415944 2415943 Bayford & Associates P.O.Box 202283, Gaborone 3956877 3956886 Begane & Associates P.O. Box 60230, Gaborone 3191078 Benito Acolatse Attorneys P.O.Box 1157, Gaborone 3956454 3956447 Bernard Bolele Attorneys P.O.Box 47048, Gaborone 3959111 3951636 Biki & Associates P.O.Box AD 137ABE, Gaborone 3952559 Bogopa Manewe & Tobedza Attorneys P.O.Box 26465, Gaborone 3905466 3905451 Bonner Attorneys Bookbinder Business Law P/Bag 382, Gaborone 3912397 3912395 Briscoe Attorneys P.O.Box 402492, Gaborone 3953377 3904809 Britz Attorneys 3957524 3957062 Callender Attorneys P.O.Box 1354, Francistown 2441418 2446886 Charles Tlagae Attorneys P.O.Box -

2011 Population and Housing Census
2011 POPULATION AND HOUSING CENSUS Ministry of Finance and Development Planning 2011 Census Slogan: Palo yame, tsela ya ditlhabololo My count, a guide to developments August 2009 CSO in Collaboration with UNFPA PROJECT DOCUMENT 2011 POPULATION AND HOUSING CENSUS Published by Central Statistics Office Private Bag 0024, Gaborone Telephone: 33671300 Fax: 3952201 E-mail:[email protected] Website: www.cso.gov.bw Contact Unit : Census Secretariat Telephone: 3671300 Ext. 1305 August 2009 COPYRIGHT RESERVED Extracts may be published if source is duly acknowledged i CONTENTS PREFACE .................................................................................................................... 1 LIST OF ABBREVIATIONS AND ACRONYMS ....................................................... 2 EXECUTIVE SUMMARY ........................................................................................... 4 1. BACKGROUND AND JUSTIFICATION ................................................................ 5 1.1 Background of the 2011 Census Taking .............................................................. 5 1.2 Justification ......................................................................................................... 5 1.2.1 Evidence-based decision making, policy-making, planning and administration ....................................................................................................... 5 1.2.2 Research .................................................................................................... 5 1.2.3 Service to stakeholders -

Botswana Environment Statistics Water Digest 2018
Botswana Environment Statistics Water Digest 2018 Private Bag 0024 Gaborone TOLL FREE NUMBER: 0800600200 Tel: ( +267) 367 1300 Fax: ( +267) 395 2201 E-mail: [email protected] Website: http://www.statsbots.org.bw Published by STATISTICS BOTSWANA Private Bag 0024, Gaborone Phone: 3671300 Fax: 3952201 Email: [email protected] Website: www.statsbots.org.bw Contact Unit: Environment Statistics Unit Phone: 367 1300 ISBN: 978-99968-482-3-0 (e-book) Copyright © Statistics Botswana 2020 No part of this information shall be reproduced, stored in a Retrieval system, or even transmitted in any form or by any means, whether electronically, mechanically, photocopying or otherwise, without the prior permission of Statistics Botswana. BOTSWANA ENVIRONMENT STATISTICS WATER DIGEST 2018 Statistics Botswana PREFACE This is Statistics Botswana’s annual Botswana Environment Statistics: Water Digest. It is the first solely water statistics annual digest. This Digest will provide data for use by decision-makers in water management and development and provide tools for the monitoring of trends in water statistics. The indicators in this report cover data on dam levels, water production, billed water consumption, non-revenue water, and water supplied to mines. It is envisaged that coverage of indicators will be expanded as more data becomes available. International standards and guidelines were followed in the compilation of this report. The United Nations Framework for the Development of Environment Statistics (UNFDES) and the United Nations International Recommendations for Water Statistics were particularly useful guidelines. The data collected herein will feed into the UN System of Environmental Economic Accounting (SEEA) for water and hence facilitate an informed management of water resources. -

Bank of Botswana
PAPER 4 BANK OF BOTSWANA DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA AS AT DECEMBER 31, 2009 PREPARED AND DISTRIBUTED BY THE BANKING SUPERVISION DEPARTMENT BANK OF BOTSWANA Foreword This directory is compiled and distributed by the Banking Supervision Department of the Bank of Botswana. While every effort has been made to ensure the accuracy of the information contained in this directory, such information is subject to frequent revision, and thus the Bank accepts no responsibility for the continuing accuracy of the information. Interested parties are advised to contact the respective financial institutions directly for any information they require. This directory excludes Collective Investment Undertakings and International Financial Services Centre non-bank entities, whose regulation and supervision have been transferred to the Non-Bank Financial Institutions Regulatory Authority. Oabile Mabusa DIRECTOR BANKING SUPERVISION DEPARTMENT 1 DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA TABLE OF CONTENTS 1. CENTRAL BANK ............................................................................................................................................. 4 2. COMMERCIAL BANKS ................................................................................................................................... 6 2.1 ABN AMRO BANK (B OTSWANA ) LIMITED ..................................................................................................... 6 2.2 ABN AMRO BANK (B OTSWANA ) OBU LIMITED ........................................................................................... -

Department of Road Transport and Safety Offices
DEPARTMENT OF ROAD TRANSPORT AND SAFETY OFFICES AND SERVICES MOLEPOLOLE • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate Tel: 5920148 Fax: 5910620 P/Bag 52 Molepolole Next to Molepolole Police MOCHUDI • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate P/Bag 36 Mochudi Tel : 5777127 Fax : 5748542 White House GABORONE Headquarters BBS Mall Plot no 53796 Tshomarelo House (Botswana Savings Bank) 1st, 2nd &3rd Floor Corner Lekgarapa/Letswai Road •Registration & Licensing of vehicles and drivers •Road safety (Public Education) Tel: 3688600/62 Fax : Fax: 3904067 P/Bag 0054 Gaborone GABORONE VTS – MARUAPULA • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Vehicle Examination Tel: 3912674/2259 P/Bag BR 318 B/Hurst Near Roads Training & Roads Maintenance behind Maruapula Flats GABORONE II – FAIRGROUNDS • Registration & Licensing of vehicles and drivers • Driver Examination : Theory Tel: 3190214/3911540/3911994 Fax : P/Bag 0054 Gaborone GABORONE - OLD SUPPLIES • Registration & Licensing of vehicles and drivers • Transport Permits • Transport Inspectorate Tel: 3905050 Fax :3932671 P/Bag 0054 Gaborone Plot 1221, Along Nkrumah Road, Near Botswana Power Corporation CHILDREN TRAFFIC SCHOOL •Road Safety Promotion for children only Tel: 3161851 P/Bag BR 318 B/Hurst RAMOTSWA •Registration & Licensing of vehicles and drivers •Driver Examination (Theory & Practical -

The Big Governance Issues in Botswana
MARCH 2021 THE BIG GOVERNANCE ISSUES IN BOTSWANA A CIVIL SOCIETY SUBMISSION TO THE AFRICAN PEER REVIEW MECHANISM Contents Executive Summary 3 Acknowledgments 7 Acronyms and Abbreviations 8 What is the APRM? 10 The BAPS Process 12 Ibrahim Index of African Governance Botswana: 2020 IIAG Scores, Ranks & Trends 120 CHAPTER 1 15 Introduction CHAPTER 2 16 Human Rights CHAPTER 3 27 Separation of Powers CHAPTER 4 35 Public Service and Decentralisation CHAPTER 5 43 Citizen Participation and Economic Inclusion CHAPTER 6 51 Transparency and Accountability CHAPTER 7 61 Vulnerable Groups CHAPTER 8 70 Education CHAPTER 9 80 Sustainable Development and Natural Resource Management, Access to Land and Infrastructure CHAPTER 10 91 Food Security CHAPTER 11 98 Crime and Security CHAPTER 12 108 Foreign Policy CHAPTER 13 113 Research and Development THE BIG GOVERNANCE ISSUES IN BOTSWANA: A CIVIL SOCIETY SUBMISSION TO THE APRM 3 Executive Summary Botswana’s civil society APRM Working Group has identified 12 governance issues to be included in this submission: 1 Human Rights The implementation of domestic and international legislation has meant that basic human rights are well protected in Botswana. However, these rights are not enjoyed equally by all. Areas of concern include violence against women and children; discrimination against indigenous peoples; child labour; over reliance on and abuses by the mining sector; respect for diversity and culture; effectiveness of social protection programmes; and access to quality healthcare services. It is recommended that government develop a comprehensive national action plan on human rights that applies to both state and business. 2 Separation of Powers Political and personal interests have made separation between Botswana’s three arms of government difficult. -

Envhydrogeology Francistown
Bundesanstalt für Geowissenschaften und Rohstoffe Environmental Hydrogeology of Francistown Effects of Mining and Urban Expansion on Groundwater Quality by Benjamin Mafa Edited by Dr. H. Vogel March 2003 TABLE OF CONTENTS Page 1 INTRODUCTION ........................................................................................................1 2 THE FRANCISTOWN STUDY AREA ............................................................................2 2.1 The climate in the study area ......................................................................................2 2.2 The topography and drainage pattern in the study area ...............................................3 2.3 The geology in the study area .....................................................................................3 2.4 The hydrogeology in the study area ............................................................................5 2.5 Potential groundwater hazards in the study area ..........................................................7 3 METHODS AND MATERIALS ....................................................................................10 4 RESULTS ..................................................................................................................12 6.1 Environmental hydrogeology maps .............................................................................12 6.2 Groundwater pollution zones .....................................................................................14 5 DISCUSSION .............................................................................................................18 -

BOTSWANA July 2004 WHO Estimate of Number of People Requiring Treatment – End 2005: 60 000 Antiretroviral Therapy Target Declared by Country: 55 000 by 2005
BOTSWANA July 2004 WHO estimate of number of people requiring treatment – end 2005: 60 000 Antiretroviral therapy target declared by country: 55 000 by 2005 treat HIV sentinel surveillance Million Angola Zambia Kasane Livingstone in pregnant women Latest available year for 2001−2003 3by Percent seropositive 2005 Less than 1 1 − 4.9 Gweru Zimbabwe 5 − 9.9 Maun 10 − 14.9 Bulawayo 15 − 19.9 Francistown 20 − 29.9 Namibia Ghanzi 30 and more Gobabis Botswana Serowe Cities and towns Main roads Population density (pers./sq.Km) Less than 10 10 − 49 MolepololeMochudi Gaborone 50 − 99 Kanye 100 − 249 Lobatse 250 − 499 South Africa 500 − 749 Pretoria Tsabong 750 and more Johannesburg Map data sources: WHO/UNAIDS Epidemiological Fact Sheets and the United States Census Bureau Map production: WHO 0 62.5 125 250 Kilometers 1. Demographic and socioeconomic data 2. HIV indicators Date Estimate Source Date Estimate Source United 35.5 – WHO/ Total population (millions) 2004 1.8 Adult prevalence of HIV/AIDS (15–49 years) 2003 Nations 39.1% UNAIDS United Estimated number of people living with 330 000 – WHO/ Population in urban areas (%) 2003 51.3 2003 Nations HIV/AIDS (0–49 years) 380 000 UNAIDS WHO/ Life expectancy at birth (years) 2002 40.4 WHO Cumulative number of reported AIDS cases 2001 10 178 UNAIDS United Reported number of people receiving June Gross domestic product per capita (US$ ) 2001 2 872 18 000 WHO Nations antiretroviral therapy (15–49 years) 2004 Estimated total number needing antiretroviral WHO/ Government budget spent on health care (%) 2001 7.6 WHO 2003 60 000 therapy in 2005 UNAIDS HIV testing and counselling sites: number of not Per capita expenditure on health (US$) 2001 190 WHO sites available HIV testing and counselling sites: number of not Human Development Index 2001 0.614 UNDP people tested at all sites available Prevalence of HIV among adults with 2002 79% WHO 3. -
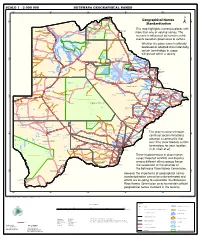
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe -

BNSC Annual Report 2018
1 Board & Department Affiliates Financial Management Reports Reports Report 2 CONTENTS BNSC Vision 2028 BOARD & MANAGEMENT 2 - 11 The Vision statement captures the “desired future state” Board Members 2 - 3 of the Statement By The Chairman 4 - 5 Organisation - what the BNSC aspires Chief Executive Officer’s Report 6 - 9 to be in the future. Management 10 - 11 The basis for the 16 year Strategy Horizon is as follows; DEPARTMENTAL REPORTS 14 - 23 Games Department 12 - 17 The period aligns to the 4 year Olympic Games Human Resources And Administration Department 18 - 20 cycle. Sport Development Department Report 19 - 20 Internal Audit Department 21 The period takes into consideration the time Lands & Facilities Department 22 - 23 required to develop athletes from the grass Business Development Department 24 - 25 roots level at an appropriate young age (6 year Sport Development Department 26 - 28 old) to elite and professional levels. NATIONAL SPORT ASSOCIATION 30 - 91 The BNSC vision statement embodies the following strategic aspirations; FINANCIAL REPORT 92 - 134 • Sport for ALL- All Batswana actively participating in sports and/or physical activity • Sport for Excellence- Professional and elite athletes achieving sustained superior performance on the world stage. • Sport for Prosperity- Sport as a development partner contributing significantly to economic diversification. Botswana hosting prestigious sporting events that contribute to national pride and contribute significant socio-economic benefits. 3 Board & Department Affiliates Financial Management Reports Reports Report Board Members 1 2 3 4 5 6 1. Solly Reikeletseng 4. Gift Nkwe Chairman Member 2. Prof. Martin Mokgwathi 5. Kago Ramokate Member Member 3. Shirley Keoagile 6. -

Mineralogy of Tailings Dump Around Selebi Phikwe Nickel-Copper Plant, Botswana
J. Appl. Sci. Environ. Mgt. 2004 JASEM ISSN 1119-8362 Available Online at All rights reserved http:// www.bioline.org.br/ja Vol. 8 (1) 37 - 44 Mineralogy of Tailings Dump around Selebi Phikwe Nickel-Copper Plant, Botswana 1*EKOSSE, G; 2VAN DEN HEEVER, D J; 3DE JAGER, L; 4TOTOLO, O 1*Department of Geology, University of Botswana, P/Bag 0022 Gaborone, Botswana 2VDH Industrial Hygiene CC.PO. Box 26792 Langenhoven Park, 9330, Free State, South Africa 3Department of Environmental Health, Technikon Free State, P/Bag X20539 Bloemfontein, Free State, South Africa 4Department of Environmental Science, University of Botswana, P/Bag 0022 Gaborone, Botswana ABSTRACT: This study aimed at mineralogically characterizing the tailings dump emanating from the mining and smelting of nickel-copper (Ni-Cu) at Selebi Phikwe, Botswana, Southern Africa. Samples of tailings dump around the Selebi Phikwe Ni-Cu plant were studied using petrographic microscopy and X-ray Powder Diffraction (XRPD) technique. The tailings dump comprised of the following minerals: nickelblodite, pyrrhotite, quartz, pentlandite, malachite, chalcopyrite, actinolite, cristobalite, tremolite, kaolinite, mica and albite. Nickelblodite and malachite were mineralized from the primary ore minerals in the tailings dump. The sulfur-rich minerals contained in the tailings dump serve as principal promoting sources for acid mine drainage in the immediate surrounding environment. Consequently, aspects of pollution management such as phytoremediation and phytomining, and environmental desulfurization could be introduced as pollution control measures at Selebi Phikwe. @JASEM Botswana is one of Africa's top three mineral some possible environmental implications resulting producers by value, including South Africa and the from the mining and extraction activities. -

Botswana Non-Profits
Botswana Non-Profits Note that other than the Botswana-UPenn Partnership, we do not endorse any of the following agencies. They are listed for information purposes only as non-profit organizations that may accept volunteers. Botswana-UPenn Partnership Location: Gaborone, Botswana Mission: To help build capacity in, clinical care, education, and research. Volunteer positions: clinical researchers Contact: Andrew Steenhoff, MD [email protected] Bana ba Keletso Orphan Day Care Centre Location: Molepolole, Botswana Mission: The broad based goal of the Centre is to support the children in the community who are orphaned. This involves providing them with the necessary skills, information, and training to reduce the psychological and social effects of being orphaned, and to reduce the risk of HIV/AIDS infection. The Centre's serves as a feeding centre, preschool and centre for school going children where they can receive counseling, as well as support for school work and mentorship. Volunteer positions: Contact: http://www.orfundfoundation.com/programs/ Elephants Without Borders Location: Kasane, Botswana Mission: Elephants Without Borders is a charitable organization dedicated to conserving wildlife and natural resources; through innovative research, education, and information sharing with all people. Volunteer positions: Contact: Michael Chase Phone/Fax: ++267 625-0202 New York State Affiliate office: EWB, Inc. 168 S. Marlin Rd., Grand Island, NY 14072, USA Phone: 001 (716) 773-1012 http://www.elephantswithoutborders.org/ Flying Mission Location: Gaborone, Botswana Mission: Flying mission serves by facilitating the spread of the Gospel of Jesus Christ through aviation, training and care ministries in Botswana, Zambia, and surrounding areas. Volunteer positions: Nurses / Fundraising / IT / Web design / Support / HR / Marketing etc.