The Effects of Valbenazine in Participants with Tardive Dyskinesia: Results of the 1-Year KINECT 3 Extension Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
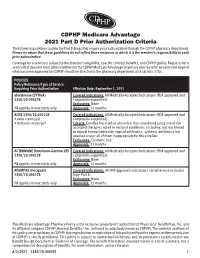
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Central Nervous System (CNS) Agents
Clinical Policy: Central Nervous System (CNS) Agents: Movement Disorders Reference Number: OH.PHAR.PPA.96 Effective Date: 01.01.2021 Last Review Date: 11.20 Line of Business: Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. MOVEMENT DISORDERS CLINICAL PA REQUIRED “PREFERRED” PA REQUIRED “NON-PREFERRED” AUSTEDO ® (deutetrabenazine)† INGREZZA® (valbenazine) TETRABENAZINE (generic of Xenazine®) † Quantity limit of 4 tablets per day Description Deutetrabenazine (Austedo®), tetrabenazine (Xenazine®) and valbenazine (Ingrezza®) are vesicular monoamine transporter 2 (VMAT2) inhibitors. FDA Approved Indication(s) Austedo is indicated for the treatment of: • Chorea associated with Huntington’s disease • Tardive dyskinesia (TD) in adults Ingrezza is indicated for the treatment of adults with tardive dyskinesia. Xenazine is indicated for the treatment of chorea associated with Huntington’s disease. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Austedo, Xenazine or Ingrezza are medically necessary when the following criteria are met: I. Initial Approval Criteria A. Chorea Associated with Huntington Disease (must meet all): Page 1 of 7 CLINICAL POLICY Central Nervous System (CNS) Agents: Movement Disorders 1. Diagnosis of chorea associated with Huntington disease; 2. Requested medication is either Austedo or Xenazine; 3. Member must meet labeled age requirements for requested medication; 4. If requested medication is Austedo member has had a trial and failure of tetrabenazine at maximally tolerated doses up to 100 mg per day, unless contraindicated or clinically significant adverse effects are experienced; 5. -

Medications to Be Avoided Or Used with Caution in Parkinson's Disease
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease This medication list is not intended to be complete and additional brand names may be found for each medication. Every patient is different and you may need to take one of these medications despite caution against it. Please discuss your particular situation with your physician and do not stop any medication that you are currently taking without first seeking advice from your physician. Most medications should be tapered off and not stopped suddenly. Although you may not be taking these medications at home, one of these medications may be introduced while hospitalized. If a hospitalization is planned, please have your neurologist contact your treating physician in the hospital to advise which medications should be avoided. Medications to be avoided or used with caution in combination with Selegiline HCL (Eldepryl®, Deprenyl®, Zelapar®), Rasagiline (Azilect®) and Safinamide (Xadago®) Medication Type Medication Name Brand Name Narcotics/Analgesics Meperidine Demerol® Tramadol Ultram® Methadone Dolophine® Propoxyphene Darvon® Antidepressants St. John’s Wort Several Brands Muscle Relaxants Cyclobenzaprine Flexeril® Cough Suppressants Dextromethorphan Robitussin® products, other brands — found as an ingredient in various cough and cold medications Decongestants/Stimulants Pseudoephedrine Sudafed® products, other Phenylephrine brands — found as an ingredient Ephedrine in various cold and allergy medications Other medications Linezolid (antibiotic) Zyvox® that inhibit Monoamine oxidase Phenelzine Nardil® Tranylcypromine Parnate® Isocarboxazid Marplan® Note: Additional medications are cautioned against in people taking Monoamine oxidase inhibitors (MAOI), including other opioids (beyond what is mentioned in the chart above), most classes of antidepressants and other stimulants (beyond what is mentioned in the chart above). -

Drug Interactions Mechanisms and Clinical Relevance Jonathan E
Drug Interactions Mechanisms and Clinical Relevance Jonathan E. Alpert, MD, PhD Dorothy and Marty Silverman Department Chair Department of Psychiatry and Behavioral Sciences Professor of Psychiatry, Neuroscience, and Pediatrics Montefiore Medical Center Albert Einstein College of Medicine Psychopharmacology 2020 www.mghcme.org Disclosures Speaker’s honoraria: American Society of Clinical Psychopharmacology, American Psychiatric Association, Eli Lilly & Co., LIJ/Zucker-Hillside, Nevada Psychiatric Association, New York University, North Shore Medical Center, Organon Inc., Psicofarma, Primedia, Reed Medical Education, University of Louisville, Xian-Janssen Royalties: Belvoir Publishing, Marcel Dekker, Institut la Conference Hippocrate Consultant fees: Consulting Medical Associates, Luye Pharmaceuticals, PamLab LLC, Pharmavite Research support: Abbott Labs, Alkermes, Aspect Medical Systems, Astra- Zeneca, Axsome Therapeutics, Bristol-Myers Squibb, Cephalon, Eli Lilly & Co., Forest Pharmaceuticals, GlaxoSmithKline, J&J Pharmaceuticals, Lichtwer Pharma, Lorex Pharmaceuticals, NARSAD, NIH, Novartis, Organon, Otsuka, PamLab LLC, PCORI, Pharmavite, Roche Laboratories, Solvay Pharma, Sanofi/Synthelabo, Wyeth-Ayerst Laboratories www.mghcme.org Drug Interactions • Ubiquitous polypharmacy • Treatment of psychiatric conditions among medically ill • Use of dietary health supplements/OTCs • Focus on preventable drug errors • Advances in pharmacokinetics and pharmacodynamics and in bioinformatics • Application of bioinformatics to large populations • -

Movement Disorders Therapeutic Class Review (TCR)
Movement Disorders Therapeutic Class Review (TCR) April 3, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. Movement -

Corporate Medical Policy Pharmacogenetics Testing AHS – M2021 “Notification”
Corporate Medical Policy Pharmacogenetics Testing AHS – M2021 “Notification” File Name: pharmacogenetics_testing Origination: 01/01/2019 Last CAP Review: n/a Next CAP Review: 01/01/2020 Last Review: 01/01/2019 Policy Effective April 1, 2019 Description of Procedure or Service Definitions Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. Cytochrome P450 are essential for the production of many molecules including steroid hormones and certain fats, including cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in cytochrome P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased possibility of toxic substance levels in the body. There are approximately 57 CYP genes in humans (Bains, 2013; National Institutes of Health, 2017). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. The azathioprine and mercaptopurine is used for treatment of nonmalignant immunologic disorders, mercaptopurine is used for treatment of lymphoid malignancies and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011) . Dihydropyrimidine dehydrogenase (DPYD) gene is encoding for dihydropyrimidine dehydrogenase (DPD) enzyme responsible for fluoropyrimidine catabolism. It is a rate-limiting enzyme. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors such as colorectal, breast and aerodigestive tract tumors (Amstutz et al., 2018). -

Valbenazine) Capsules, for Oral Use Biosciences, Inc
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------ADVERSE REACTIONS------------------------------ These highlights do not include all the information needed to use Most common adverse reaction (≥5% and twice the rate of placebo): INGREZZA safely and effectively. See full prescribing information for somnolence. (6.1) INGREZZA. To report SUSPECTED ADVERSE REACTIONS, contact Neurocrine INGREZZATM (valbenazine) capsules, for oral use Biosciences, Inc. at 877-641-3461 or FDA at 1-800-FDA-1088 or Initial U.S. Approval: 2017 www.fda.gov/medwatch. -----------------------------INDICATIONS AND USAGE-------------------------- ------------------------------DRUG INTERACTIONS------------------------------- INGREZZA is a vesicular monoamine transporter 2 (VMAT2) inhibitor Dose adjustments due to drug interactions (2.3, 7): indicated for the treatment of adults with tardive dyskinesia. (1) Factors Dose Adjustments for INGREZZA ------------------------DOSAGE AND ADMINISTRATION---------------------- Use of MAOIs with INGREZZA Avoid concomitant use with The initial dose is 40 mg once daily. After one week, increase the dose to MAOIs. the recommended dose of 80 mg once daily. (2.1) Use of strong CYP3A4 inducers Concomitant use is not Can be taken with or without food. (2.1) with INGREZZA recommended. The recommended dose for patients with moderate or severe hepatic Use of strong CYP3A4 inhibitors Reduce dose to 40 mg. impairment is 40 mg once daily. (2.2) with INGREZZA Consider dose reduction based on tolerability in known CYP2D6 poor Use of strong CYP2D6 inhibitors Consider dose reduction based on metabolizers. (2.2) with INGREZZA tolerability. ---------------------DOSAGE FORMS AND STRENGTHS---------------------- --------------------------USE IN SPECIFIC POPULATIONS--------------------- Capsules: 40 mg. (3) Pregnancy: May cause fetal harm. (8.1) Lactation: Advise not to breastfeed. (8.2) -------------------------------CONTRAINDICATIONS------------------------------ Renal Impairment: No dosage adjustment is necessary for patients with None. -

2017 New Drug Update
Financial Disclosures • Mark S. Johnson, Pharm.D., BCPS • Name of commercial interest(s) NEW DRUG UPDATE • Stockholder in Merck and various mutual funds Mark S. Johnson, Pharm.D., BCPS Professor of Pharmacy Practice Director of Postgraduate Education Bernard J. Dunn School of Pharmacy Shenandoah University Objectives FDA Approvals • Identify the new drugs approved by the FDA that are most • 2015 clinically relevant to general practice in 2017 • 45 New Molecular Entities / New Biologics • Discuss relevant indications, efficacy, pharmacokinetics, • 35 New Dosage Forms safety, and dosing of the new drugs • Discuss how the new drugs differ from existing drugs on • 2016 the market • 22 New Molecular Entities / New Biologics • 41 New Dosage Forms • Describe how to best incorporate the new drugs into clinical practice using a case-based format • 2017 to date • 20 New Molecular Entities / 14 New Biologics • 25 New Dosage Forms • 1 Withdrawal Withdrawals • Oxymorphone (Opana ER™)—Endo • Requested by FDA to be withdrawn due to concern of benefits no longer outweighing the risks • First time FDA has taken steps to remove a currently marketed opioid from sale due to the public health consequences of abuse • Post marketing data demonstrated increase in the route of abuse from nasal to injection following reformulation in 2012 (original approval in 2006), intended to make the drug resistant to physical and chemical manipulation for abuse by snorting or injecting • Injection abuse of reformulation associated with HIV, hepatitis C, thrombotic microangiopathy http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DrugInnovation/ucm534863.htm 1 Self Assessment Questions 1. Betrixaban (Bevyxxa™) is FDA-approved for which of the following indications? SIGNIFICANT NEW MOLECULAR A. -

Valbenazine for Tardive Dyskinesia
Out of the Pipeline Valbenazine for tardive dyskinesia Jonathan M. Meyer, MD Valbenazine espite improvements in the toler- Table 1 reduces tardive ability of antipsychotic medica- Fast facts about valbenazine tions, the development of tardive dyskinesia severity D Brand name: Ingrezza dyskinesia (TD) still is a significant area of with once-daily Class: VMAT2 antagonist concern; however, clinicians have had few dosing and Indication: Tardive dyskinesia treatment options. Valbenazine, a vesicu- Approval date: April 11, 2017 no CYP2D6 lar monoamine transport type 2 (VMAT2) Availability date: May 1, 2017 monitoring inhibitor, is the only FDA-approved medi- Manufacturer: Neurocrine Biosciences cation for TD (Table 1).1 By modulating Dosing forms: 40-mg and 80-mg capsules dopamine transport into presynaptic Recommended dosage: 40 mg in the vesicles, synaptic dopamine release is morning, increasing to 80 mg/d after 1 week decreased, thereby reducing the post- synaptic stimulation of D2 receptors and the severity of dyskinetic movements. In the pivotal 6-week clinical trial, val- does not have tetrabenazine’s kinetic limi- benazine significantly reduced TD sever- tations, adverse effect profile, or CYP2D6 ity as measured by Abnormal Involuntary monitoring requirements represents an Movement Scale (AIMS) ratings.2 Study enormous advance in the treatment of TD. completion rates were high (87.6%), with only 2 dropouts because of adverse Clinical implications events in each of the placebo (n = 78) and Tardive dyskinesia remains a signifi- 40-mg (n = 76) arms, and 3 in the 80-mg cant public health concern because of the group (n = 80). increasing use of antipsychotics for disor- Before the development of valbenazine, ders beyond the core indication for schizo- tetrabenazine was the only effective option phrenia.