Corporate Medical Policy Pharmacogenetics Testing AHS – M2021 “Notification”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pindolol of the Activation of Postsynaptic 5-HT1A Receptors
Potentiation by (-)Pindolol of the Activation of Postsynaptic 5-HT1A Receptors Induced by Venlafaxine Jean-Claude Béïque, Ph.D., Pierre Blier, M.D., Ph.D., Claude de Montigny, M.D., Ph.D., and Guy Debonnel, M.D. The increase of extracellular 5-HT in brain terminal regions antagonist WAY 100635 (100 g/kg, i.v.). A short-term produced by the acute administration of 5-HT reuptake treatment with VLX (20 mg/kg/day ϫ 2 days) resulted in a inhibitors (SSRI’s) is hampered by the activation of ca. 90% suppression of the firing activity of 5-HT neurons somatodendritic 5-HT1A autoreceptors in the raphe nuclei. in the dorsal raphe nucleus. This was prevented by the The present in vivo electrophysiological studies were coadministration of (-)pindolol (15 mg/kg/day ϫ 2 days). undertaken, in the rat, to assess the effects of the Taken together, these results indicate that (-)pindolol coadministration of venlafaxine, a dual 5-HT/NE reuptake potentiated the activation of postsynaptic 5-HT1A receptors inhibitor, and (-)pindolol on pre- and postsynaptic 5-HT1A resulting from 5-HT reuptake inhibition probably by receptor function. The acute administration of venlafaxine blocking the somatodendritic 5-HT1A autoreceptor, but not and of the SSRI paroxetine (5 mg/kg, i.v.) induced a its postsynaptic congener. These results support and extend suppression of the firing activity of dorsal hippocampus CA3 previous findings providing a biological substratum for the pyramidal neurons. This effect of venlafaxine was markedly efficacy of pindolol as an accelerating strategy in major potentiated by a pretreatment with (-)pindolol (15 mg/kg, depression. -

ZHONG-THESIS-2016.Pdf
ANTIDEPRESSANTMINING AZ AMAZ DESIGNING A WEBBASED ALGORITHM AND VISUAL LANGUAGE FOR ANTIDEPRESSANT DRUG SELECTION TO EDUCATE PRIMARY CARE PRACTITIONERS By Amy Zhong A thesis submitted to Johns Hopkins University in conformity with the requirements for the degree of Master of Arts Baltimore, Maryland March, 2016 © 2016 Amy Zhong All Rights Reserved ABSTRACT Depression is a common mental disorder that affects approximately 14.8 million American adults each year. In addition to being a debilitating condition, depression often occurs in tandem with other medical conditions such as diabetes, heart disease, and cancer. While psychiatric professionals are essential for the management of mental health, majority of patients seek care from their primary care practitioners. This phenomenon is of great concern because diagnosis of depression within primary care settings has only been accurate 25-50% of the time. The antidepressant drug selection algorithm utilizes a unique formula to integrate patient and family medical histories, patient symptoms, and patient preferences to make optimal treatment selections. The development of a visual language explores the use of graphic elements to improve understanding of major pharmacological mechanisms, knowledge essential to making rational DQWLGHSUHVVDQWGUXJVHOHFWLRQV,QFUHDWLQJWKLVPRELOHZHEEDVHGDSSOLFDWLRQZHKRSHWR¿OOD void in resources available to primary care practitioners, and improve management of mental health within the primary care setting. By Amy Zhong Chairpersons of the Supervisory Committee Adam I. Kaplin, M.D., Ph.D., esis Preceptor Assistant Professor, Departments of Psychiatry and Neurology e Johns Hopkins University School of Medicine Kristen Rahn Hollinger, Ph.D., esis Preceptor Instructor, Departments of Psychiatry and Neurology e Johns Hopkins University School of Medicine Jennifer E. -

Strategies for Managing Sexual Dysfunction Induced by Antidepressant Medication
King’s Research Portal DOI: 10.1002/14651858.CD003382.pub3 Document Version Publisher's PDF, also known as Version of record Link to publication record in King's Research Portal Citation for published version (APA): Taylor, M. J., Rudkin, L., Bullemor-Day, P., Lubin, J., Chukwujekwu, C., & Hawton, K. (2013). Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database of Systematic Reviews, (5). https://doi.org/10.1002/14651858.CD003382.pub3 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

M2021: Pharmacogenetic Testing
Pharmacogenetic Testing Policy Number: AHS – M2021 – Pharmacogenetic Prior Policy Name and Number, as applicable: Testing • M2021 – Cytochrome P450 Initial Presentation Date: 06/16/2021 Revision Date: N/A I. Policy Description Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome (CYP) P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. CYP P450 are essential to produce many biochemical building blocks, such as cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in CYP P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased levels of toxic substances in the body. Approximately 58 CYP genes are in humans (Bains, 2013; Tantisira & Weiss, 2019). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. Azathioprine and mercaptopurine are used for treatment of nonmalignant immunologic disorders; mercaptopurine is used for treatment of lymphoid malignancies; and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011). Dihydropyrimidine dehydrogenase (DPD), encoded by the gene DPYD, is a rate-limiting enzyme responsible for fluoropyrimidine catabolism. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors, such as colorectal, breast, and aerodigestive tract tumors (Amstutz et al., 2018). A variety of cell surface proteins, such as antigen-presenting molecules and other proteins, are encoded by the human leukocyte antigen genes (HLAs). -

Flibanserin (Addyi)
STEPS New Drug Reviews Flibanserin (Addyi) for Hypoactive Sexual Desire Disorder in Premenopausal Women HARRY HOLT, MD, and JEFFREY TINGEN, PharmD, MBA, University of Virginia Health System, Charlottesville, Virginia STEPS new drug reviews Flibanserin (Addyi) is labeled for the treatment of acquired, generalized hypoactive sexual cover Safety, Tolerability, desire disorder (HSDD) in premenopausal women. It is a nonhormonal medication that Effectiveness, Price, and 1 Simplicity. Each indepen- affects serotonin receptors to increase libido. dent review is provided by authors who have no financial association with Drug Dosage Dose form Cost* the drug manufacturer. Flibanserin (Addyi) 100 mg per day at bedtime 100-mg tablet $830 This series is coordinated by Allen F. Shaughnessy, *—Estimated retail price of one month’s treatment based on information obtained at http://www.goodrx.com PharmD, MMedEd, (accessed April 1, 2016). Contributing Editor. A collection of STEPS pub- lished in AFP is available at http://www.aafp.org/ SAFETY EFFECTIVENESS afp/steps. The main risks of flibanserin are hypoten- Flibanserin has been evaluated in three ran- sion (2%) and syncope (0.4%), which are domized, double-blind, placebo-controlled more likely to occur in patients who have studies of 2,375 premenopausal women also ingested alcohol. For this reason, women with acquired, generalized HSDD, defined should not drink alcohol when taking fliban- as low sexual desire causing marked dis- serin; about one in six persons taking this tress or interpersonal difficulties.2 Women combination will experience clinically signif- in monogamous, heterosexual relationships icant hypotension and syncope.1 Flibanserin with no known cause of HSDD reported should not be taken by women with hepatic an average increase of 1.6 to 2.5 additional impairment or women who are also taking satisfying sexual events per month with treat- moderate or strong cytochrome P450 3A4 ment, from a baseline of 2.5 to 3.0 per month. -
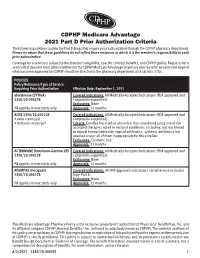
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

Dosing and Monitoring: Children and Adolescents
Dosing and Monitoring: Children and Adolescents Glenn S. Hirsch, MD Keith S. Ditkowski, MD Child & Adolescent Dosing.indd 1 08-01-2018 14:56:52 Adapted from Child & Adolescent Dosing.indd 76 08-01-2018 14:56:50 DISCLAIMER This pocket reference is provided as a service to medicine by the publisher, Medworks Media Inc. This review does not imply the publisher’s agreement with the views expressed herein. Although every effort has been made to ensure that drug doses and other information are presented accurately in this publication, the ultimate responsibility rests with the prescribing physician. Neither the publisher, nor the authors can be held responsible for errors or for any consequences arising from the use of information contained herein. Readers are strongly urged to consult any relevant primary literature. No claims or endorsements are made for any drug or compound currently under clinical investigation. In an effort to allow for the widest distribution of these guidelines, the authors have modified the originally printed material to more closely conform to the limitations of product labeling. For many of the drugs discussed herein, initiation at lower doses may increase tolerability and efficacy. Copyright ©2018, MedWorks Media Inc., 2205 Rockefeller Lane, Redondo Beach, CA 90278. Printed in the USA. All rights reserved, including the right of reproduction, in whole or in part, in any form. Child & Adolescent Dosing.indd 2 08-01-2018 14:56:52 Dosing and Monitoring: Children and Adolescents Glenn S. Hirsch, MD Keith S. Ditkowski, MD Dr. Hirsch is the deputy director of the New York University Child Study Center, the medical director in the Division of Child and Adolescent Psychiatry, and the assistant professor of psychiatry at the New York University School of Medicine. -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

(Flibanserin) (Flibanserin) Tablets
™ MEDICATION GUIDE addyi ADDYI™ (add-ee) (flibanserin) (flibanserin) Tablets Read this Medication Guide before you start taking ADDYI™ and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor. What is the most important information I should know about ADDYI? Your risk of severe low blood pressure and fainting (loss of consciousness) is increased if you take ADDYI and: • drink alcohol. Do not drink alcohol if you take ADDYI. • take certain prescription medicines, over-the-counter medicines, or herbal supplements. Do not take or start taking any prescription medicines, over-the-counter medicines, or herbal supplements while taking ADDYI until you have talked with your doctor. Your doctor will tell you if it is safe to take other medicines or herbal supplements while you are taking ADDYI. • have liver problems. Do not take ADDYI if you have liver problems. If you take ADDYI and you feel lightheaded or dizzy, lie down right away. Get emergency medical help or ask someone to get emergency medical help for you if the symptoms do not go away or if you faint (lose consciousness). If you faint (lose consciousness), tell your doctor as soon as you can. ADDYI is only available through the ADDYI Risk Evaluation and Mitigation Strategy (REMS) Program because of the increased risk of severe low blood pressure and fainting (loss of consciousness) with alcohol use. You can only get ADDYI from pharmacies that are enrolled in the ADDYI REMS Program. For more information about the Program and a list of pharmacies that are enrolled in the ADDYI REMS Program, go to www.AddyiREMS.com or call 1-844-PINK-PILL (1-844- 746-5745). -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

(12) United States Patent (10) Patent No.: US 7,776,345 B2 Dudhara Et Al
USOO7776345B2 (12) United States Patent (10) Patent No.: US 7,776,345 B2 Dudhara et al. (45) Date of Patent: Aug. 17, 2010 (54) GASTRIC RETENTION CONTROLLED DRUG 4,996,058 A 2f1991 Sinnreich DELIVERY SYSTEM 5,091, 184 A 2, 1992 Khanna ...................... 424/435 5,096,714 A 3, 1992 Kuhrts (75) Inventors: Kamlesh Mohanlal Dudhara, Baroda 5,651,985 A 7/1997 Penners et al. 5,654,005 A * 8/1997 Chen et al. .................. 424/480 (IN); Nitin Bhalachandra 6,261,601 B1* 7/2001 Talwar et al. ... ... 424/469 Dharmadhikari, Mumbai (IN); Vaishali 6,340.475 B2 * 1/2002 Shell et al. .................. 424/469 Vijay Dhavse, Mumbai (IN) 6,960,356 B1 1 1/2005 Talwar et al. 7,109,239 B2 * 9/2006 Gallop et al. ............... 514,533 (73) Assignee: Sun Pharma Advanced Research 2007/0265343 A1 11/2007 Dharmadhikari et al. Company Ltd, Andheri (East) (IN) FOREIGN PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this EP 1095650 5, 2001 patent is extended or adjusted under 35 JP 630.14715 1, 1988 U.S.C. 154(b) by 1759 days. WO WO 98.51408 11, 1998 WO 99.47 128 A1 9, 1999 (21) Appl. No.: 10/482,770 WO OO15198 A1 3, 2000 WO WOOOf 15198 3, 2000 (22) PCT Filed: Jul. 4, 2002 WO WOOO, 23045 4/2000 WO WOOO,386.50 * 7/2OOO (86). PCT No.: PCT/NO2AOO144 WO 01/08670 A2 2, 2001 WO WO 01/10417 A1 2, 2001 S371 (c)(1), WO WO 01/10419 A1 2, 2001 (2), (4) Date: Dec.