Central Nervous System (CNS) Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
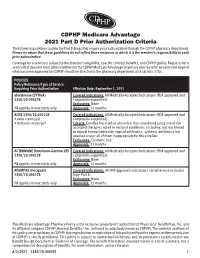
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

Formulary (List of Covered Drugs)
3ODQ<HDU 202 Formulary (List of Covered Drugs) PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THE FOLLOWING PLAN: $0 Cost Share AI/AN HMO Minimum Coverage HMO Silver 70 HMO Active Choice PPO Silver Opal 25 Gold HMO Silver 70 OFF Exchange HMO Amber 50 HMO Silver Opal 50 Silver HMO Silver 73 HMO Bronze 60 HDHP HMO Platinum 90 HMO Silver 87 HMO Bronze 60 HMO Ruby 10 Platinum HMO Silver 94 HMO Gold 80 HMO Ruby 20 Platinum HMO Jade 15 HMO Ruby 40 Platinum HMO This formulary was last updated on8//20. This formulary is VXEMHFWto change and all previous versions of the formulary no longer apply. For more recent information or other questions, please contact Chinese Community Health Plan Member Services at 1-888-775-7888 or, for TTY users, 1-877-681-8898, seven days a week from 8:00 a.m. to 8:00 p.m., or visit www.cchphealthplan.com/family-member -,-ϭ -,-ϭ"&* !#" + 5 5 ),-$+" %(%'.')/"+#" %&/"+ -%/"$)% "%&/"+ *& )&! %&/"+ 0 $(#" '"+ %&/"+ *& %&/"+ %&/"+ +)(2" &-%(.' %&/"+ +)(2" .1&-%(.' %&/"+ )&! .1&-%(.' !" .1&-%(.' dŚŝƐĨŽƌŵƵůĂƌLJǁĂƐůĂƐƚƵƉĚĂƚĞĚ8ͬϭͬϮϬϮϭ͘dŚŝƐĨŽƌŵƵůĂƌLJŝƐƐƵďũĞĐƚƚŽ ĐŚĂŶŐĞĂŶĚĂůůƉƌĞǀŝŽƵƐǀĞƌƐŝŽŶƐŽĨƚŚĞĨŽƌŵƵůĂƌLJŶŽůŽŶŐĞƌĂƉƉůLJ͘&ŽƌŵŽƌĞ ƌĞĐĞŶƚŝŶĨŽƌŵĂƚŝŽŶŽƌŽƚŚĞƌƋƵĞƐƚŝŽŶƐ͕ƉůĞĂƐĞĐŽŶƚĂĐƚŚŝŶĞƐĞŽŵŵƵŶŝƚLJ ,ĞĂůƚŚWůĂŶDĞŵďĞƌ^ĞƌǀŝĐĞƐĂƚϭͲϴϴϴͲϳϳϱͲϳϴϴϴŽƌ͕ĨŽƌddzƵƐĞƌƐ͕ ϭͲϴϳϳͲϲϴϭͲϴϴϵϴ͕ƐĞǀĞŶĚĂLJƐĂǁĞĞŬĨƌŽŵϴ͗ϬϬĂ͘ŵ͘ƚŽϴ͗ϬϬƉ͘ŵ͕͘ŽƌǀŝƐŝƚ ǁǁǁ͘ĐĐŚƉŚĞĂůƚŚƉůĂŶ͘ĐŽŵͬĨĂŵŝůLJͲŵĞŵďĞƌ !! %+)&,+ &%+&+&)$,#)0),# *+666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I % + &%*6666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I -

Antipsychotics (Part-4) FLUOROBUTYROPHENONES
Antipsychotics (Part-4) FLUOROBUTYROPHENONES The fluorobutyrophenones belong to a much-studied class of compounds, with many compounds possessing high antipsychotic activity. They were obtained by structure variation of the analgesic drug meperidine by substitution of the N-methyl by butyrophenone moiety to produce the butyrophenone analogue which has similar activity as chlorpromazine. COOC2H5 N H3C Meperidine COOC2H5 N O Butyrophenone analog The structural requirements for antipsychotic activity in the group are well worked out. General features are expressed in the following structure. F AR Y O N • Optimal activity is seen when with an aromatic with p-fluoro substituent • When CO is attached with p-fluoroaryl gives optimal activity is seen, although other groups, C(H)OH and aryl, also give good activity. • When 3 carbons distance separates the CO from cyclic N gives optimal activity. • The aliphatic amino nitrogen is required, and highest activity is seen when it is incorporated into a cyclic form. • AR is an aromatic ring and is needed. It should be attached directly to the 4-position or occasionally separated from it by one intervening atom. • The Y group can vary and assist activity. An example is the hydroxyl group of haloperidol. The empirical SARs suggest that the 4-aryl piperidino moiety is superimposable on the 2-- phenylethylamino moiety of dopamine and, accordingly, could promote affinity for D2 receptors. The long N-alkyl substituent could help promote affinity and produce antagonistic activity. Some members of the class are extremely potent antipsychotic agents and D2 receptor antagonists. The EPS are extremely marked in some members of this class, which may, in part, be due to a potent DA block in the striatum and almost no compensatory striatal anticholinergic block. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Diphenylbutylpiperidine Antipsychotic Drugs Inhibit Prolactin Receptor
Gastroenterology 2020;158:1433–1449 Diphenylbutylpiperidine Antipsychotic Drugs Inhibit Prolactin Receptor Signaling to Reduce Growth of Pancreatic Ductal Adenocarcinoma in Mice Prasad Dandawate,1 Gaurav Kaushik,2 Chandrayee Ghosh,1 David Standing,1 Afreen Asif Ali Sayed,1 Sonali Choudhury,1 Dharmalingam Subramaniam,1 Ann Manzardo,3 Tuhina Banerjee,4 Santimukul Santra,4 Prabhu Ramamoorthy,1 Merlin Butler,3 Subhash B. Padhye,1,5 Joaquina Baranda,6 Anup Kasi,6 Weijing Sun,6 Ossama Tawfik,7 Domenico Coppola,8 Mokenge Malafa,8 Shahid Umar,2 Michael J. Soares,7,9,10,11 Subhrajit Saha,12 Scott J. Weir,1,13 Animesh Dhar,1 Roy A. Jensen,1,7 Sufi Mary Thomas,1,14 and Shrikant Anant1,2,5 1Department of Cancer Biology, University of Kansas Medical Center, Kansas City, Kansas; 2Department of Surgery, University of Kansas Medical Center, Kansas City, Kansas; 3Department of Psychiatry and Behavioral Sciences, University of Kansas Medical Center, Kansas City, Kansas; 4Department of Chemistry, Pittsburg State University, Pittsburg, Kansas; 5Interdisciplinary Science and Technology Research Academy, Abeda Inamdar College, University of Pune, Pune; 6Department of Internal Medicine, University of Kansas Medical Center, Kansas City, Kansas; 7Department of Pathology and Laboratory Medicine, University of Kansas Medical Center, Kansas City, Kansas; 8Department of Gastrointestinal Oncology, H. Lee Moffitt Cancer Center and Research Institute, Tampa, Florida; 9Department of Obstetrics and Gynecology, University of Kansas Medical Center, Kansas City, Kansas; 10Department -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Repurposing Diphenylbutylpiperidine-Class Antipsychotic Drugs for Host
bioRxiv preprint doi: https://doi.org/10.1101/2021.06.05.447191; this version posted June 6, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Repurposing diphenylbutylpiperidine-class antipsychotic drugs for host- 2 directed therapy of Mycobacterium tuberculosis and Salmonella enterica 3 infections 4 Heemskerk MT1, Korbee CJ1, Esselink J1, Carvalho dos Santos C1,2, van Veen S1, Gordijn IF1, 5 Vrieling F1, Walburg KV1, Engele CG1, Dijkman K3, Wilson L1, Verreck FAW3, Ottenhoff 6 THM1* and Haks MC1*. 7 1Department of Infectious Diseases, Leiden University Medical Center, Leiden, The 8 Netherlands. 2Laboratório Especial de Desenvolvimento de Vacinas, Instituto Butantan, São 9 Paulo, Brazil. 3TB research group, Department of Parasitology, Biomedical Primate Research 10 Centre, Rijswijk, The Netherlands. 11 * contributed equally. 12 13 14 15 Corresponding author: Tom HM Ottenhoff 16 Dept. of Infectious Diseases 17 Leiden University Medical Center (LUMC) 18 Albinusdreef 2 19 2333 ZA Leiden 20 The Netherlands 21 Tel: +31 71 526 2620 22 E-mail: [email protected] 23 ORCID ID: 0000-0003-3706-3403 24 25 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.06.05.447191; this version posted June 6, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. -

Current Topics in Medicinal Chemistry, 2016, 16, 3385-3403 REVIEW ARTICLE
Send Orders for Reprints to [email protected] 3385 Cur rent Topics in Medicinal Chemistry, 2016, 16, 3385-3403 REVIEW ARTICLE ISSN: 1568-0266 eISSN: 1873-5294 Dopamine Targeting Drugs for the Treatment of Schizophrenia: Past, Impact Factor: 2.9 The international Present and Future journal for in-depth reviews on Current Topics in Medicinal Chemistry BENTHAM SCIENCE Peng Li*, Gretchen L. Snyder and Kimberly E. Vanover Intra-Cellular Therapies Inc, 430 East 29th Street, Suite 900, New York, NY 10016, USA Abstract: Schizophrenia is a chronic and debilitating neuropsychiatric disorder affecting approxi- mately 1% of the world’s population. This disease is associated with considerable morbidity placing a major financial burden on society. Antipsychotics have been the mainstay of the pharmacological treatment of schizophrenia for decades. The traditional typical and atypical antipsychotics demon- strate clinical efficacy in treating positive symptoms, such as hallucinations and delusions, while are A R T I C L E H I S T O R Y largely ineffective and may worsen negative symptoms, such as blunted affect and social withdrawal, as well as cognitive function. The inability to treat these latter symptoms may contribute to social Received: April 07, 2016 Revised: May 20, 2016 function impairment associated with schizophrenia. The dysfunction of multiple neurotransmitter Accepted: May 23, 2016 systems in schizophrenia suggests that drugs selectively targeting one neurotransmission pathway DOI: 10.2174/1568026616666160608 are unlikely to meet all the therapeutic needs of this heterogeneous disorder. Often, however, the un- 084834 intentional engagement of multiple pharmacological targets or even the excessive engagement of in- tended pharmacological targets can lead to undesired consequences and poor tolerability. -

Medications to Be Avoided Or Used with Caution in Parkinson's Disease
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease This medication list is not intended to be complete and additional brand names may be found for each medication. Every patient is different and you may need to take one of these medications despite caution against it. Please discuss your particular situation with your physician and do not stop any medication that you are currently taking without first seeking advice from your physician. Most medications should be tapered off and not stopped suddenly. Although you may not be taking these medications at home, one of these medications may be introduced while hospitalized. If a hospitalization is planned, please have your neurologist contact your treating physician in the hospital to advise which medications should be avoided. Medications to be avoided or used with caution in combination with Selegiline HCL (Eldepryl®, Deprenyl®, Zelapar®), Rasagiline (Azilect®) and Safinamide (Xadago®) Medication Type Medication Name Brand Name Narcotics/Analgesics Meperidine Demerol® Tramadol Ultram® Methadone Dolophine® Propoxyphene Darvon® Antidepressants St. John’s Wort Several Brands Muscle Relaxants Cyclobenzaprine Flexeril® Cough Suppressants Dextromethorphan Robitussin® products, other brands — found as an ingredient in various cough and cold medications Decongestants/Stimulants Pseudoephedrine Sudafed® products, other Phenylephrine brands — found as an ingredient Ephedrine in various cold and allergy medications Other medications Linezolid (antibiotic) Zyvox® that inhibit Monoamine oxidase Phenelzine Nardil® Tranylcypromine Parnate® Isocarboxazid Marplan® Note: Additional medications are cautioned against in people taking Monoamine oxidase inhibitors (MAOI), including other opioids (beyond what is mentioned in the chart above), most classes of antidepressants and other stimulants (beyond what is mentioned in the chart above). -

Drug Interactions Mechanisms and Clinical Relevance Jonathan E
Drug Interactions Mechanisms and Clinical Relevance Jonathan E. Alpert, MD, PhD Dorothy and Marty Silverman Department Chair Department of Psychiatry and Behavioral Sciences Professor of Psychiatry, Neuroscience, and Pediatrics Montefiore Medical Center Albert Einstein College of Medicine Psychopharmacology 2020 www.mghcme.org Disclosures Speaker’s honoraria: American Society of Clinical Psychopharmacology, American Psychiatric Association, Eli Lilly & Co., LIJ/Zucker-Hillside, Nevada Psychiatric Association, New York University, North Shore Medical Center, Organon Inc., Psicofarma, Primedia, Reed Medical Education, University of Louisville, Xian-Janssen Royalties: Belvoir Publishing, Marcel Dekker, Institut la Conference Hippocrate Consultant fees: Consulting Medical Associates, Luye Pharmaceuticals, PamLab LLC, Pharmavite Research support: Abbott Labs, Alkermes, Aspect Medical Systems, Astra- Zeneca, Axsome Therapeutics, Bristol-Myers Squibb, Cephalon, Eli Lilly & Co., Forest Pharmaceuticals, GlaxoSmithKline, J&J Pharmaceuticals, Lichtwer Pharma, Lorex Pharmaceuticals, NARSAD, NIH, Novartis, Organon, Otsuka, PamLab LLC, PCORI, Pharmavite, Roche Laboratories, Solvay Pharma, Sanofi/Synthelabo, Wyeth-Ayerst Laboratories www.mghcme.org Drug Interactions • Ubiquitous polypharmacy • Treatment of psychiatric conditions among medically ill • Use of dietary health supplements/OTCs • Focus on preventable drug errors • Advances in pharmacokinetics and pharmacodynamics and in bioinformatics • Application of bioinformatics to large populations •