Drug Interactions Mechanisms and Clinical Relevance Jonathan E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Postmortem Distribution of Vardenafil (Levitra | in an Aviation
Journal of Analytical Toxicology, Vol. 31, July/August 2007 The Postmortem Distribution of Vardenafil (Levitra| in an Aviation Accident Victim with an Unusually High Blood Concentration* Robert D. Johnson ~, Russell J. Lewis, and Mike K. Angler Downloaded from https://academic.oup.com/jat/article/31/6/328/682815 by guest on 27 September 2021 Civil Aerospace Medical Institute, Federal Aviation Administration, Analytical Toxicology and Accident Research Laboratory, AAM-610, CAMI Building, 6500 S. MacArthur Blvd., Oklahoma City, Oklahoma 73169-6901 I Abstract phodiesterase type 5 enzyme (PDE5) found predominantly in the penile corpus cavernosum (2-7). Vardenafil (tevitra) is one of the most widely prescribed Vardenafil undergoes hepatic metabolism, producing the treatments for erectile dysfunction. This report presents a active desethyl metabolite M1. M1 contributes to the ob- rapid and reliable method for the identification and quantification served pharmacological effects provided by vardenafil, as M1 of vardenafil in postmortem fluids and tissues, applies this method exhibits approximately 30% of the potency of the parent to a postmortem case, and describes the distribution of vardenafil in various fluids and tissues.This procedure utilizes sildenafil-d8, drug (1). Under steady-state conditions, the plasma concen- which is structurally closely related to vardenafil, as an tration of M1 is approximately 26% of that seen for vardenafil internal standard for more accurate and reliable quantitation. (1). After oral administration of vardenafil, peak plasma con- The method incorporates solid-phaseextraction and liquid centrations are obtained within 30-60 min (1). Vardenafil chromatography-tandem mass spectrometry (MS) and and its active metabolite have a terminal half-life of approx- MS-MS-MS utilizing an atmospheric pressure chemical imately 4-5 h (1). -

M2021: Pharmacogenetic Testing
Pharmacogenetic Testing Policy Number: AHS – M2021 – Pharmacogenetic Prior Policy Name and Number, as applicable: Testing • M2021 – Cytochrome P450 Initial Presentation Date: 06/16/2021 Revision Date: N/A I. Policy Description Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome (CYP) P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. CYP P450 are essential to produce many biochemical building blocks, such as cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in CYP P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased levels of toxic substances in the body. Approximately 58 CYP genes are in humans (Bains, 2013; Tantisira & Weiss, 2019). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. Azathioprine and mercaptopurine are used for treatment of nonmalignant immunologic disorders; mercaptopurine is used for treatment of lymphoid malignancies; and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011). Dihydropyrimidine dehydrogenase (DPD), encoded by the gene DPYD, is a rate-limiting enzyme responsible for fluoropyrimidine catabolism. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors, such as colorectal, breast, and aerodigestive tract tumors (Amstutz et al., 2018). A variety of cell surface proteins, such as antigen-presenting molecules and other proteins, are encoded by the human leukocyte antigen genes (HLAs). -
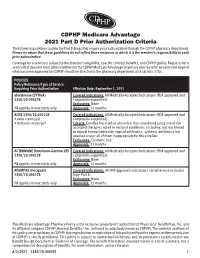
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

Deutetrabenazine
PATIENT & CAREGIVER EDUCATION Deutetrabenazine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Austedo Warning This drug may raise the chance of depression and suicidal thoughts or actions in people with Huntington’s disease. If you have ever had depression or suicidal thoughts or actions, talk with your doctor. This drug may not be right for you. People who take this drug must be watched closely. Call your doctor right away if you have signs like depression, nervousness, restlessness, grouchiness, panic attacks, or any other changes in feelings, mood, or behavior. Call your doctor right away if you have any thoughts or actions of suicide. What is this drug used for? It is used to treat disabling involuntary movements in Huntington’s chorea. It is used to treat tardive dyskinesia. What do I need to tell my doctor BEFORE I take this drug? If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have or have ever had depression or thoughts of suicide. Deutetrabenazine 1/6 If you have liver disease. If you have ever had a long QT on ECG or other heartbeat that is not normal. If you have taken certain drugs for depression or Parkinson’s disease in the last 14 days. This includes isocarboxazid, phenelzine, tranylcypromine, selegiline, or rasagiline. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

Vardenafil Better Choice for Premature Ejaculation
August 15, 2005 • www.familypracticenews.com Men’s Health 47 Vardenafil Better Choice for Premature Ejaculation BY ROBERT FINN (24%) of the men and was secondary (in On a self-rating scale of 0-8, where 0 Center but is now at the University of San Francisco Bureau most cases to erectile dysfunction) in the means PE almost never, 4 means PE about Hamburg. remaining 26 men (77%). half the time, and 8 means PE almost al- Self-ratings of sexual satisfaction, on a 0- S AN A NTONIO — Vardenafil improved After a 4-week run-in period, 17 men ways, the mean score was 6.14 at baseline, 5 scale, where 0 means not at all satisfied premature ejaculation more than sertra- were given 10-mg vardenafil 10 minutes 4.28 with sertraline, and 3.2 with varde- and 5 means extremely satisfied, averaged line, Frank Sommer, M.D., reported at the before intercourse for 6 weeks. The other nafil. 1.4 at baseline, 3.2 with sertraline, and 4.2 annual meeting of the American Urolog- 17 received 50 mg of sertraline 4 hours be- IVELT, as measured by a stopwatch, with vardenafil. In addition, the partners’ ical Association. fore intercourse. averaged 0.54 minutes at baseline, 2.87 sexual satisfaction showed significant in- Both vardenafil (Levitra), a phosphodi- After a 1-week washout period, the men minutes with sertraline, and 5.23 minutes creases for sertraline and even more so for esterase-5 inhibitor, and sertraline (Zoloft), who had been receiving sertraline with vardenafil, reported Dr. Sommer, vardenafil. -

LEVITRA (Vardenafil Hcl) Tablets
LEVITRA (vardenafil HCl) Tablets DESCRIPTION LEVITRA® is an oral therapy for the treatment of erectile dysfunction. This monohydrochloride salt of vardenafil is a selective inhibitor of cyclic guanosine monophosphate (cGMP)-specific phosphodiesterase type 5 (PDE5). Vardenafil HCl is designated chemically as piperazine, 1-[[3-(1,4-dihydro-5- methyl-4-oxo-7-propylimidazo[5,1-f][1,2,4]triazin-2-yl)-4- ethoxyphenyl]sulfonyl]-4-ethyl-, monohydrochloride and has the following structural formula: O O HN N x HCl x 3H2O N N O S O N N Vardenafil HCl is a nearly colorless, solid substance with a molecular weight of 579.1 g/mol and a solubility of 0.11 mg/mL in water. LEVITRA is formulated as orange, round, film-coated tablets with "BAYER" cross debossed on one side and "2.5", "5", "10", and "20" on the other side corresponding to 2.5 mg, 5 mg, 10 mg, and 20 mg of vardenafil, respectively. In addition to the active ingredient, vardenafil HCl, each tablet contains microcrystalline cellulose, crospovidone, colloidal silicon dioxide, magnesium stearate, hypromellose, polyethylene glycol, titanium dioxide, yellow ferric oxide, and red ferric oxide. CLINICAL PHARMACOLOGY Mechanism of Action Penile erection is a hemodynamic process initiated by the relaxation of smooth muscle in the corpus cavernosum and its associated arterioles. During sexual stimulation, nitric oxide is released from nerve endings and endothelial cells in the corpus cavernosum. Nitric oxide activates the enzyme guanylate cyclase resulting in increased synthesis of cyclic guanosine monophosphate (cGMP) in the smooth muscle cells of the corpus cavernosum. The cGMP in turn triggers smooth muscle relaxation, allowing increased blood flow into the penis, resulting in erection. -

Austedo (Deutetrabenazine)
Market Applicability/Effective Date FL & FL FL Market GA KS KY LA MD NJ NV NY TN TX WA FHK MMA LTC Applicable X N/A N/A X N/A X X X X X X N/A N/A NA *FHK- Florida Healthy Kids Austedo (deutetrabenazine) Override(s) Approval Duration Prior Authorization 1 year Medications Quantity Limit Austedo (deutetrabenazine) May be subject to quantity limit APPROVAL CRITERIA Initial requests for Austedo (deutetrabenazine) may be approved for individuals who meet the following criteria: I. Individual is 18 years of age or older; AND II. Individual has a diagnosis of chorea associated with Huntington’s disease; OR III. Individual has a diagnosis of tardive dyskinesia (TD) confirmed by the following (DSM-5): A. At least 60 days of stable (drug, dose) medication exposure (either typical or first generation antipsychotic agents [such as, chlorpromazine, haloperidol, fluphenazine], atypical or second-generation antipsychotic agents [such as, clozapine, risperidone, olanzapine, quetiapine, aripiprazole], or certain dopamine receptor-blocking drugs used in treatment of nausea and gastroparesis [such as, prochlorperazine, promethazine, metoclopramide]); AND B. Presence of involuntary athetoid or choreiform movements lasting at least 30 days. Requests for continuation of therapy for Austedo (deutetrabenazine) may be approved for individuals who meet the following criteria: I. Individual has experienced an improvement in symptoms deemed to be clinically significant by the provider. Requests for Austedo (deutetrabenazine) may not be approved for individuals who meet the following criteria: I. Individual is suicidal or has untreated/inadequately treated depression; OR II. Individual has hepatic impairment; OR III. Individual is currently utilizing monoamine oxidase inhibitors (MAOIs), reserpine, or tetrabenazine. -

Review of Deutetrabenazine: a Novel Treatment for Chorea Associated with Huntington’S Disease
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2018 Volume: 12 Drug Design, Development and Therapy Dovepress Running head verso: Dean and Sung Running head recto: Review of deutetrabenazine for treatment of chorea in HD open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S138828 Open Access Full Text Article REVIEW Review of deutetrabenazine: a novel treatment for chorea associated with Huntington’s disease Marissa Dean Abstract: Deutetrabenazine was recently approved for the treatment of chorea in Huntington’s Victor W Sung disease (HD) and is the first deuterated medication that has been US Food and Drug Adminis- tration (FDA)-approved for therapeutic use. In this article, we review deutetrabenazine’s drug Department of Neurology, Division of Movement Disorders, University of design, pharmacokinetics, drug interactions, efficacy, adverse events, comparison with tetra- Alabama at Birmingham, Birmingham, benazine, dosage, and administration. Deutetrabenazine is a deuterated form of tetrabenazine AL, USA and is a vesicular monoamine transporter 2 (VMAT2) inhibitor. The substitution of deuterium for hydrogen at key positions in the tetrabenazine molecule allows a longer drug half-life and less frequent daily dosing. Deutetrabenazine is administered twice daily up to a maximum daily dose of 48 mg, which corresponds to a similar daily dose of 100 mg of tetrabenazine. In a Phase III clinical trial (First-HD), there was a statistically significant improvement of chorea in HD subjects, as well as improvements in global impression of change as assessed by both patients and clinicians. This improvement was seen without significant adverse effects as the overall tolerability profile of deutetrabenazine was similar to placebo. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented.