Movement Disorders Therapeutic Class Review (TCR)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tardive Dyskinesia
Tardive Dyskinesia Tardive Dyskinesia Checklist The checklist below can be used to help determine if you or someone you know may have signs associated with tardive dyskinesia and other movement disorders. Movement Description Observed? Rhythmic shaking of hands, jaw, head, or feet Yes Tremor A very rhythmic shaking at 3-6 beats per second usually indicates extrapyramidal symptoms or side effects (EPSE) of parkinsonism, even No if only visible in the tongue, jaw, hands, or legs. Sustained abnormal posture of neck or trunk Yes Dystonia Involuntary extension of the back or rotation of the neck over weeks or months is common in tardive dystonia. No Restless pacing, leg bouncing, or posture shifting Yes Akathisia Repetitive movements accompanied by a strong feeling of restlessness may indicate a medication side effect of akathisia. No Repeated stereotyped movements of the tongue, jaw, or lips Yes Examples include chewing movements, tongue darting, or lip pursing. TD is not rhythmic (i.e., not tremor). These mouth and tongue movements No are the most frequent signs of tardive dyskinesia. Tardive Writhing, twisting, dancing movements Yes Dyskinesia of fingers or toes Repetitive finger and toe movements are common in individuals with No tardive dyskinesia (and may appear to be similar to akathisia). Rocking, jerking, flexing, or thrusting of trunk or hips Yes Stereotyped movements of the trunk, hips, or pelvis may reflect tardive dyskinesia. No There are many kinds of abnormal movements in individuals receiving psychiatric medications and not all are because of drugs. If you answered “yes” to one or more of the items above, an evaluation by a psychiatrist or neurologist skilled in movement disorders may be warranted to determine the type of disorder and best treatment options. -
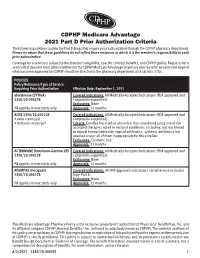
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -
Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

New Zealand Data Sheet 1
New Zealand Data Sheet 1. PRODUCT NAME Motetis 25 mg tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each Motetis 25 mg tablets contains 25 mg of tetrabenazine. Excipient(s) with known effect Contains lactose monohydrate. For the full list of excipients, see Section 6.1. 3. PHARMACEUTICAL FORM Yellow, round, flat tablet with a score line on one side. The tablet can be divided into equal halves. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Movement disorders associated with organic central nervous system conditions, such as Huntington's chorea, hemiballismus and senile chorea. Tetrabenazine is also indicated for the treatment of moderate to severe tardive dyskinesia, which is disabling and/or socially embarrassing. The condition should be persistent despite withdrawal of antipsychotic therapy, or in cases where withdrawal of antipsychotic medication is not a realistic option; also, where the condition persists despite reduction in dosage of antipsychotic medication or switching to atypical antipsychotic medication. 4.2. Dose and method of administration Dose Proper dosing of tetrabenazine involves careful titration of therapy to determine an individualised dose for each patient. When first prescribed, tetrabenazine therapy should be titrated slowly over several weeks to allow the identification of a dose for chronic use that reduces chorea and is well tolerated. Movement disorders Dosage and administration are variable and only a guide is given. An initial starting dose of 25 mg three times a day is recommended. This can be increased by 25 mg a day every three (3) or four (4) days until 200 mg per day is being given or the limit of tolerance, as dictated by unwanted effects, is reached, whichever is the lower dose. -

Drug-Induced Movement Disorders
Medical Management of Early PD Samer D. Tabbal, M.D. May 2016 Associate Professor of Neurology Director of The Parkinson Disease & Other Movement Disorders Program Mobile: +961 70 65 89 85 email: [email protected] Conflict of Interest Statement No drug company pays me any money Outline So, you diagnosed Parkinson disease .Natural history of the disease .When to start drug therapy? .Which drug to use first for symptomatic treatment? ● Levodopa vs dopamine agonist vs MAOI Natural History of Parkinson Disease Before levodopa: Death within 10 years After levodopa: . “Honeymoon” period (~ 5-7 years) . Motor (ON/OFF) fluctuations & dyskinesias: ● Drug therapy effective initially ● Surgical intervention by 10-15 years - Deep brain stimulation (DBS) therapy Motor Response Dyskinesia 5-7 yrs >10 yrs Dyskinesia ON state ON state OFF state OFF state time time Several days Several hours 1-2 hour Natural History of Parkinson Disease Prominent gait impairment and autonomic symptoms by 20-25 years (Merola 2011) Behavioral changes before or with motor symptoms: . Sleep disorders . Depression . Anxiety . Hallucinations, paranoid delusions Dementia at anytime during the illness . When prominent or early: diffuse Lewy body disease Symptoms of Parkinson Disease Motor Symptoms Sensory Symptoms Mental Symptoms: . Cognitive and psychiatric Autonomic Symptoms Presenting Symptoms of Parkinson Disease Mood disorders: depression and lack of motivation Sleep disorders: “acting out dreams” and nightmares Early motor symptoms: Typically Unilateral . Rest tremor: chin, arms or legs or “inner tremor” . Bradykinesia: focal and generalized slowness . Rigidity: “muscle stiffness or ache” Also: (usually no early postural instability) . Facial masking with hypophonia: “does not smile anymore” or “looks unhappy all the time” . -

2009 Paris, France the Movement Disorder Society’S 13Th International Congress of Parkinson’S Disease and Movement Disorders
FINAL PROGRAM The Movement Disorder Society’s 13th International Congress OF PARKINSon’S DISEASE AND MOVEMENT DISORDERS JUNE 7-11, 2009 Paris, France The Movement Disorder Society’s 13th International Congress of Parkinson’s Disease and Movement Disorders Claiming CME Credit To claim CME credit for your participation in the MDS 13th International Congress of Parkinson’s Disease and Movement Disorders, International Congress participants must complete and submit an online CME Request Form. This Form will be available beginning June 10. Instructions for claiming credit: • After June 10, visit www.movementdisorders.org/congress/congress09/cme • Log in following the instructions on the page. You will need your International Congress Reference Number, located on the upper right of the Confirmation Sheet found in your registration packet. • Follow the on-screen instructions to claim CME Credit for the sessions you attended. • You may print your certificate from your home or office, or save it as a PDF for your records. Continuing Medical Education The Movement Disorder Society is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Credit Designation The Movement Disorder Society designates this educational activity for a maximum of 30.5 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. Non-CME Certificates of Attendance were included with your on- site registration packet. If you did not receive one, please e-mail [email protected] to request one. The Movement Disorder Society has sought accreditation from the European Accreditation Council for Continuing Medical Education (EACCME) to provide the following CME activity for medical specialists. -

Tourette's Syndrome
Tourette’s Syndrome CHRISTOPHER KENNEY, MD; SHENG-HAN KUO, MD; and JOOHI JIMENEZ-SHAHED, MD Baylor College of Medicine, Houston, Texas Tourette’s syndrome is a movement disorder most commonly seen in school-age children. The incidence peaks around preadolescence with one half of cases resolving in early adult- hood. Tourette’s syndrome is the most common cause of tics, which are involuntary or semi- voluntary, sudden, brief, intermittent, repetitive movements (motor tics) or sounds (phonic tics). It is often associated with psychiatric comorbidities, mainly attention-deficit/hyperac- tivity disorder and obsessive-compulsive disorder. Given its diverse presentation, Tourette’s syndrome can mimic many hyperkinetic disorders, making the diagnosis challenging at times. The etiology of this syndrome is thought to be related to basal ganglia dysfunction. Treatment can be behavioral, pharmacologic, or surgical, and is dictated by the most incapacitating symp- toms. Alpha2-adrenergic agonists are the first line of pharmacologic therapy, but dopamine- receptor–blocking drugs are required for multiple, complex tics. Dopamine-receptor–blocking drugs are associated with potential side effects including sedation, weight gain, acute dystonic reactions, and tardive dyskinesia. Appropriate diagnosis and treatment can substantially improve quality of life and psychosocial functioning in affected children. (Am Fam Physician. 2008;77(5):651-658, 659-660. Copyright © 2008 American Academy of Family Physicians.) ▲ Patient information: n 1885, Georges Gilles de la Tourette normal context or in inappropriate situa- A handout on Tourette’s described the major clinical features tions, thus calling attention to the person syndrome, written by the authors of this article, is of the syndrome that now carries his because of their exaggerated, forceful, and provided on p. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Substituted 3-Isobutyl-9, 10-Dimethoxy-1,3,4,6,7,11B
(19) TZZ Z_ 9B_T (11) EP 2 081 929 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 471/04 (2006.01) 09.01.2013 Bulletin 2013/02 (86) International application number: (21) Application number: 07864160.2 PCT/US2007/084176 (22) Date of filing: 08.11.2007 (87) International publication number: WO 2008/058261 (15.05.2008 Gazette 2008/20) (54) SUBSTITUTED 3-ISOBUTYL-9, 10-DIMETHOXY-1,3,4,6,7,11B-HEXAHYDRO-2H-PYRIDO[2,1-A] ISOQUINOLIN-2-OL COMPOUNDS AND METHODS RELATING THERETO SUBSTITUIERTE 3-ISOBUTYL-9,10-DIMETHOXY-1,3,4,6,7,11B-HEXAHYDRO-2H-PYRIDO[2,1-A] ISOCHINOLIN-2-OLVERBINDUNGEN UND DIESE BETREFFENDE VERFAHREN COMPOSÉS 3-ISOBUTYL-9, 10-DIMÉTHOXY-1,3,4,6,7,11B-HEXAHYDRO-2H-PYRIDO[2,1-A] ISOQUINOLIN-2-OL SUBSTITUÉS ET PROCÉDÉS ASSOCIÉS (84) Designated Contracting States: (56) References cited: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • BROSSIA ET AL: "SYNTHESEVERSUCHE IN DER HU IE IS IT LI LT LU LV MC MT NL PL PT RO SE EMETIN-REIHE 3. MITTEILUNG 2-HYDROXY- SI SK TR HYDROBENZOÄAÜCHINOLIZINE" HELVETICA Designated Extension States: CHIMICA ACTA, VERLAG HELVETICA CHIMICA AL BA HR MK RS ACTA. BASEL, CH, vol. 41, no. 4, 1958, pages 1793-1806, XP008047475 ISSN: 0018-019X (30) Priority: 08.11.2006 US 864944 P • KILBOURN M R ET AL: "Absolute Configuration of (+)-alpha-Dihydrotetrabenazine, an Active (43) Date of publication of application: Metabolite of Tetrabenazine" CHIRALITY, WILEY- 29.07.2009 Bulletin 2009/31 LISS, NEW YORK, US, vol. -

Tetrabenazine: the First Approved Drug for the Treatment of Chorea in US Patients with Huntington Disease
Neuropsychiatric Disease and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW 7HWUDEHQD]LQHWKHÀUVWDSSURYHGGUXJ for the treatment of chorea in US patients with Huntington disease Samuel Frank Abstract: Huntington disease (HD) is a dominantly inherited progressive neurological disease Boston University School of Medicine, characterized by chorea, an involuntary brief movement that tends to flow between body regions. Boston, Massachusetts, USA HD is typically diagnosed based on clinical findings in the setting of a family history and may be confirmed with genetic testing. Predictive testing is available to those at risk, but only experienced clinicians should perform the counseling and testing. Multiple areas of the brain degenerate mainly involving the neurotransmitters dopamine, glutamate, and G-aminobutyric acid. Although pharmacotherapies theoretically target these neurotransmitters, few well-conducted trials for symptomatic or neuroprotective interventions yielded positive results. Tetrabenazine (TBZ) is a dopamine-depleting agent that may be one of the more effective agents for reducing chorea, although it has a risk of potentially serious adverse effects. Some newer antipsychotic agents, such as olanzapine and aripiprazole, may have adequate efficacy with a more favorable adverse-effect profile than older antipsychotic agents for treating chorea and psychosis. This review will address the epidemiology and diagnosis of HD as background for understanding potential pharmacological treatment options. Because TBZ is the only US Food and Drug Administration-approved medication in the United States for HD, the focus of this review will be on its pharmacology, efficacy, safety, and practical uses. There are no current treatments to change the course of HD, but education and symptomatic therapies can be effective tools for clinicians to use with patients and families affected by HD.