2017 New Drug Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms and Clinical Significance of Pharmacokinetic-Based Drug-Drug Interactions With
DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Title Mechanisms and Clinical Significance of Pharmacokinetic-based Drug-drug Interactions with Drugs Approved by the U.S. Food and Drug Administration in 2017 Jingjing Yu, Ichiko D. Petrie, René H. Levy, and Isabelle Ragueneau-Majlessi Department of Pharmaceutics, School of Pharmacy, University of Washington, Seattle, WA, USA (J.Y., I.P., R.H.L. I.R-M.) Downloaded from dmd.aspetjournals.org at ASPET Journals on October 3, 2021 1 DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Running Title Page a) Running title: A review of clinical DDIs in 2017 NDAs b) Corresponding author: Jingjing Yu, Drug Interaction Database (DIDB) Program, Department of Pharmaceutics, School of Pharmacy, University of Washington, Box 357610, Seattle, WA 98195, Phone: 206.221.2856, Fax: 206.543.3204, E-mail: [email protected] c) Number of text pages: 18 Number of tables: 2 Downloaded from Number of figures: 2 Number of references: 38 Number of words in the Abstract: 242 dmd.aspetjournals.org Number of words in the Introduction: 227 Number of words in the Discussion: 619 d) Abbreviations: at ASPET Journals on October 3, 2021 AUC, area under the time-plasma concentration curve; BCRP, breast cancer resistance protein; Cmax, maximum plasma -

WHO Drug Information Vol
WHO Drug Information Vol. 31, No. 3, 2017 WHO Drug Information Contents Medicines regulation 420 Post-market monitoring EMA platform gains trade mark; Automated 387 Regulatory systems in India FDA field alert reports 421 GMP compliance Indian manufacturers to submit self- WHO prequalification certification 421 Collaboration 402 Prequalification process quality China Food and Drug Administration improvement initiatives: 2010–2016 joins ICH; U.S.-EU cooperation in inspections; IGDRP, IPRF initiatives to join 422 Medicines labels Safety news Improved labelling in Australia 423 Under discussion 409 Safety warnings 425 Approved Brimonidine gel ; Lactose-containing L-glutamine ; Betrixaban ; C1 esterase injectable methylprednisolone inhibitor (human) ; Meropenem and ; Amoxicillin; Azithromycin ; Fluconazole, vaborbactam ; Delafloxacin ; Glecaprevir fosfluconazole ; DAAs and warfarin and pibrentasvir ; Sofosbuvir, velpatasvir ; Bendamustine ; Nivolumab ; Nivolumab, and voxilaprevir ; Cladribine ; Daunorubicin pembrolizumab ; Atezolizumab ; Ibrutinib and cytarabine ; Gemtuzumab ozogamicin ; Daclizumab ; Loxoprofen topical ; Enasidenib ; Neratinib ; Tivozanib ; preparations ; Denosumab ; Gabapentin Guselkumab ; Benznidazole ; Ciclosporin ; Hydroxocobalamine antidote kit paediatric eye drops ; Lutetium oxodotreotide 414 Diagnostics Gene cell therapy Hightop HIV home testing kits Tisagenlecleucel 414 Known risks Biosimilars Warfarin ; Local corticosteroids Bevacizumab; Adalimumab ; Hydroquinone skin lighteners Early access 415 Review outcomes Idebenone -

Inbrija, INN-Levodopa
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Inbrija 33 mg inhalation powder, hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each hard capsule contains 42 mg levodopa. Each delivered dose contains 33 mg levodopa. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Inhalation powder, hard capsule. White opaque capsules containing white powder, with “A42” printed in black on the cap of the capsule and two black bands printed on the body of the capsule. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Inbrija is indicated for the intermittent treatment of episodic motor fluctuations (OFF episodes) in adult patients with Parkinson’s disease (PD) treated with a levodopa/dopa-decarboxylase inhibitor. 4.2 Posology and method of administration Posology Patients should be on a stable levodopa/dopa-decarboxylase inhibitor (e.g. carbidopa or benserazide) regimen before starting Inbrija. Patients selected for treatment with Inbrija should be able to recognize the onset of their 'OFF' symptoms and be capable of preparing the inhaler or else have a responsible care giver able to prepare the inhaler for them when required. Inbrija should be inhaled when symptoms, motor or non-motor, of an OFF period start to return. The recommended dose of Inbrija is 2 hard capsules up to 5 times per day each delivering 33 mg levodopa. The maximum daily dose of Inbrija should not exceed 10 capsules (330 mg). It is not recommended to take more than 2 capsules per OFF period. Exceeding the recommended dose may lead to increased levodopa associated adverse reactions. -

207145Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 207145Orig1s000 OTHER REVIEW(S) CSS Consult: NDA 207,145 Safinamide M E M O R A N D U M Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research * Date: March 8, 2017 To: Billy Dunn, M.D., Director Division of Neurology Products Through: Martin Rusinowitz, M.D., Medical Officer Silvia Calderon, Ph.D., Pharmacologist Controlled Substance Staff From: Alicja Lerner, M.D., Ph.D., Medical Officer Controlled Substance Staff Subject: Erratum-CSS Review of NDA 207,145 dated December 29, 2016 (Author: Lerner, Alicja) AMENDMENT This memorandum corrects an error and changes the title of Table 4, page 14, in the previously submitted CSS review dated Dec 29, 2016. In our prior review, we erroneously listed the subject population reporting the tabulated adverse events as comprising only healthy volunteers (HV). However, as indicated in the revised Table Title, the data derived from Phase 2 and Phase 3 controlled trials. This erratum does not change the conclusions or recommendations in the previous CSS review. Table 4 should read: Table 4. Summary of Selected Abuse Potential Adverse Events from all Completed Safinamide Phase 2 and Phase 3 Controlled Trials for PD – All Pooled Studies (based on the table 11, page 27, 8 factor-analysis). 1 of 2 Reference ID: 4066812 CSS Consult: NDA 207,145 Safinamide Body System Or Organ Class All Safinamide Placebo pool pool N=919 N=1516 (n, %) (n, %) Patients with at least one abuse potential event 230 (15.2) -
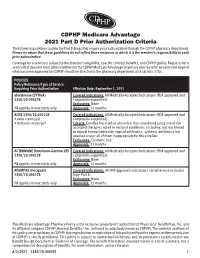
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

Inflammatory Conditions – Kevzara™ (Sarilumab for Subcutaneous Injection)
Cigna National Formulary Coverage Policy Prior Authorization Inflammatory Conditions – Kevzara® (sarilumab for subcutaneous injection) Table of Contents Product Identifier(s) National Formulary Medical Necessity ................ 1 59231 Conditions Not Covered....................................... 2 Background .......................................................... 2 References .......................................................... 3 Revision History ................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -

New Biologics in Psoriasis: an Update on IL-23 and IL-17 Inhibitors
New Biologics in Psoriasis: An Update on IL-23 and IL-17 Inhibitors Joanna Dong, BA; Gary Goldenberg, MD PRACTICE POINTS • The newest biologics for treatment of moderate to severe plaque psoriasis are IL-23 and IL-17 inhibitors with unprecedented efficacy of complete skin clearance compared to older biologics. • Risankizumab, guselkumab, and tildrakizumab are new IL-23 inhibitors currently in phase 3 trials with promising early efficacy and safety results. • Ixekizumab, which recently was approved, and brodalumab, which is pending US Food and Drug Administration review, are new IL-17 inhibitors that achieved total skin clearance in more than one-quarter of phase 3 participants after 12 weeks of treatment. copy not As immune-related pathways involved in the he role of current biologic therapies in pso- pathogenesis of psoriasis are elucidated, new riasis predicates on the pathogenic role of biologic treatments targeting these steps of the Tupregulated, immune-related mechanisms psoriatic immune cascade are developed. In Dothis that result in the activation of myeloid dendritic article, we review the literature on IL-23 and IL-17 cells, which release IL-17, IL-23, and other cytokines inhibitors in the pipeline for use in moderate to to activate T cells, including helper T cell TH17. severe psoriasis. Numerous pipeline biologic Along with other immune cells, TH17 produces therapies, including risankizumab, guselkumab, IL-17. This proinflammatory cascade results in kera- tildrakizumab, ixekizumab, and brodalumab, are tinocyte proliferation, angiogenesis, and migration being investigated in phase 2 and 3 studies to of immune cells toward psoriatic lesions.1 Thus, the establish the efficacy and safety of these new newest classes of biologics target IL-12, IL-23, and agents. -

Emerging Therapies in Psoriasis: a Systematic Review
CLINICAL REVIEW Emerging Therapies In Psoriasis: A Systematic Review Erica B. Lee, BS; Mina Amin, BS; Tina Bhutani, MD; Jashin J. Wu, MD soriasis is a chronic, autoimmune-mediated disease PRACTICE POINTS estimated to affect 2.8% of the US population.1 The pathogenesis of psoriasis is thought to involve a • Tumor necrosis factor α, I L-23, and IL-17A are key P targets for psoriasis therapy based on an under- complex process triggered by a combination of genetic standing of the key role that these cytokines play and environmental factors that induce tumor necrosis in the pathophysiology of disease. factor (TNF) α secretion by keratinocytes, which in turn • The biologic agents secukinumab and ixekizumab activates dendritic cells. Activated dendritic cells produce 2,3 are approved for use in the management of pso- IL-23, leading to helper T cell (TH17) differentiation. riasis. Other biologics—brodalumab, bimekizumab, TH17 cells secrete IL-17A, which has been shown to pro- guselkumab, tildrakizumab, risankizumab, and cer- mote psoriatic skincopy changes.4 Therefore, TNF-α, IL-23, tolizumab pegol—have been (and some continue to and IL-17A have been recognized as key targets for pso- be) the focus of phase 2 and phase 3 clinical trials. riasis therapy. • Findings of several of those trials support the idea that The newest biologic agents targeting IL-17– therapies targeting IL-23, specifically its p19 subunit, mediated pathways include ixekizumab, brodalumab, but that spare IL-12 are effective against psoriasis. andnot bimekizumab. Secukinumab, the first US Food and • Longer-term studies are needed to determine whether Drug Administration (FDA)–approved IL-17 inhibitor, the agents reviewed here, including those approved for has been available since 2015 and therefore is not clinical use, are suitable for prolonged administration. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

(12) Patent Application Publication (10) Pub. No.: US 2017/0172932 A1 Peyman (43) Pub
US 20170172932A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2017/0172932 A1 Peyman (43) Pub. Date: Jun. 22, 2017 (54) EARLY CANCER DETECTION AND A 6LX 39/395 (2006.01) ENHANCED IMMUNOTHERAPY A61R 4I/00 (2006.01) (52) U.S. Cl. (71) Applicant: Gholam A. Peyman, Sun City, AZ CPC .......... A61K 9/50 (2013.01); A61K 39/39558 (US) (2013.01); A61K 4I/0052 (2013.01); A61 K 48/00 (2013.01); A61K 35/17 (2013.01); A61 K (72) Inventor: sham A. Peyman, Sun City, AZ 35/15 (2013.01); A61K 2035/124 (2013.01) (21) Appl. No.: 15/143,981 (57) ABSTRACT (22) Filed: May 2, 2016 A method of therapy for a tumor or other pathology by administering a combination of thermotherapy and immu Related U.S. Application Data notherapy optionally combined with gene delivery. The combination therapy beneficially treats the tumor and pre (63) Continuation-in-part of application No. 14/976,321, vents tumor recurrence, either locally or at a different site, by filed on Dec. 21, 2015. boosting the patient’s immune response both at the time or original therapy and/or for later therapy. With respect to Publication Classification gene delivery, the inventive method may be used in cancer (51) Int. Cl. therapy, but is not limited to such use; it will be appreciated A 6LX 9/50 (2006.01) that the inventive method may be used for gene delivery in A6 IK 35/5 (2006.01) general. The controlled and precise application of thermal A6 IK 4.8/00 (2006.01) energy enhances gene transfer to any cell, whether the cell A 6LX 35/7 (2006.01) is a neoplastic cell, a pre-neoplastic cell, or a normal cell.