MSM Chapter 1200 3/1/21
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms and Clinical Significance of Pharmacokinetic-Based Drug-Drug Interactions With
DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Title Mechanisms and Clinical Significance of Pharmacokinetic-based Drug-drug Interactions with Drugs Approved by the U.S. Food and Drug Administration in 2017 Jingjing Yu, Ichiko D. Petrie, René H. Levy, and Isabelle Ragueneau-Majlessi Department of Pharmaceutics, School of Pharmacy, University of Washington, Seattle, WA, USA (J.Y., I.P., R.H.L. I.R-M.) Downloaded from dmd.aspetjournals.org at ASPET Journals on October 3, 2021 1 DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Running Title Page a) Running title: A review of clinical DDIs in 2017 NDAs b) Corresponding author: Jingjing Yu, Drug Interaction Database (DIDB) Program, Department of Pharmaceutics, School of Pharmacy, University of Washington, Box 357610, Seattle, WA 98195, Phone: 206.221.2856, Fax: 206.543.3204, E-mail: [email protected] c) Number of text pages: 18 Number of tables: 2 Downloaded from Number of figures: 2 Number of references: 38 Number of words in the Abstract: 242 dmd.aspetjournals.org Number of words in the Introduction: 227 Number of words in the Discussion: 619 d) Abbreviations: at ASPET Journals on October 3, 2021 AUC, area under the time-plasma concentration curve; BCRP, breast cancer resistance protein; Cmax, maximum plasma -

LGM-Pharma-Regulatory-1527671011
Pipeline Products List Specialty Portfolio Updated Q2 2018 Updated Q2 2018 See below list of newly approved API’s, samples are readily available for your R&D requirements: Inhalation Ophthalmic Transdermal Sublingual Abaloparatide Defibrotide Sodium Liraglutide Rituximab Abciximab Deforolimus Lixisenatide Rivastigmine Aclidinium Bromide Azelastine HCl Agomelatine Alprazolam Abemaciclib Delafloxacin Lumacaftor Rivastigmine Hydrogen Tartrate Beclomethasone Dipropionate Azithromycin Amlodipine Aripiprazole Acalabrutinib Denosumab Matuzumab Rizatriptan Benzoate Budesonide Besifloxacin HCl Apomorphine Eletriptan HBr Aclidinium Bromide Desmopressin Acetate Meloxicam Rocuronium Bromide Adalimumab Difluprednate Memantine Hydrochloride Rolapitant Flunisolide Bimatoprost Clonidine Epinephrine Aflibercept Dinoprost Tromethamine Micafungin Romidepsin Fluticasone Furoate Brimonidine Tartrate Dextromethorphan Ergotamine Tartrate Agomelatine Dolasetron Mesylate Mitomycin C Romosozumab Fluticasone Propionate Bromfenac Sodium Diclofenac Levocetrizine DiHCl Albiglutide Donepezil Hydrochloride Mometasone Furoate Rotigotine Formoterol Fumarate Cyclosporine Donepezil Meclizine Alectinib Dorzolamide Hydrochloride Montelukast Sodium Rucaparib Iloprost Dexamethasone Valerate Estradiol Melatonin Alemtuzumab Doxercalciferol Moxifloxacin Hydrochloride Sacubitril Alirocumab Doxorubicin Hydrochloride Mycophenolate Mofetil Salmeterol Xinafoate Indacaterol Maleate Difluprednate Fingolimod Meloxicam Amphotericin B Dulaglutide Naldemedine Secukinumab Levalbuterol Dorzolamide -

Specialty Drug List 10-22-12 Final
Iowa Medicaid Specialty Drug List Effective 10/22/2012 “Specialty” drugs include biological drugs, blood-derived products, complex molecules, and select oral, injectable, and infused medications identified by the Department and reimbursed at AWP-17% plus the dispensing fee. Specialty pricing will be applied to both the brand and generic drug products. NOTE: See the PDL at www.iowamedicaidpdl.com for specific PA criteria for the following drugs. BRAND NAME GENERIC NAME AGENTS FOR GAUCHER DISEASE ELELYSO taliglucerase alfa VPRIV velaglucerase alfa ALS RILUTEK riluzole ALCOHOL DEPENDENCE VIVITROL naltrexone AMINOGLYCOSIDES TOBI tobramycin ANTI-ASTHMATICS ALPHA PROTEINASE INHIBITORS ARALAST proteinase inhibitor ARALAST NP proteinase inhibitor PROLASTIN, C proteinase inhibitor ZEMAIRA alpha-1 proteinase inhibitor ANTIASTHMATIC - BETA - ADRENERGICS BRETHINE INJECTION turbutaline sulfate ANTIASTHMATIC - HYDRO-LYTIC ENZYMES KALYDECO ivacaftor ANTIBIOTICS - MISC. CAYSTON aztreonam lysine for inhal soln ANTI-CATAPLECTIC AGENTS XYREM sodium oxybate oral solution ANTICOAGULANTS ARIXTRA fondaparinux sodium FRAGMIN dalteparin sodium INNOHEP tinzaparin sodium LOVENOX enoxaparin sodium ANTICONVULSANTS SABRIL vigabatrin ANTIDOTES FERRIPROX deferiprone ANTIDOTES - CHELATING AGENTS CHEMET succimer EXJADE deferasirox tab for oral susp Page 1 of 10 ANTIEMETIC - TETRAHYDROCANNABINOL (THC) DERIVATIVES MARINOL dronabinol ANTIFUNGALS - ASSORTED AMBISOME amphotericin B Liposome IV for suspension ANCOBON flucytosine CANCIDAS caspofungin acetate for IV solution -

2 Total Pharmaceutical Sales
OECD Health Statistics 2021 Definitions, Sources and Methods Total pharmaceutical sales Total sales of pharmaceutical products on the domestic market, in total and by selected Anatomical Therapeutic Chemical (ATC) classification groups, based on retail prices (which means the final price paid by the customer). The ATC codes below are based on the 2021 version of the ATC Index. All alterations implemented from January 2021 are available on the WHO Collaborating Centre for Drug Statistics Methodology website at http://www.whocc.no/atc/lists_of_new_atc_ddds_and_altera/alterations_in_atc_ddd/. Note: There are at least three possible sources of under-reporting of drug sales in different countries: 1) sales data may only cover those drugs that are reimbursed by public insurance schemes; 2) they may be based on ex-factory or wholesale prices rather than retail prices; and 3) sales data may exclude drug consumption in hospitals. Data for the following countries under-estimate pharmaceutical sales reported in this section because of one of these limitations: Australia, Austria, France, Germany, Greece, Japan, Luxembourg, the Netherlands, the Slovak Republic (before 2016) and Spain. (For further information, see the country-specific information below). Please also note that depending on the allocation of pharmaceutical products with more than one use, differences in reporting of specific drugs may occur across countries, thereby affecting the relative size of specific ATC groups. Data should reflect total sales for each drug category, based on -

Expression of Recombinant Human Androgen Receptor and Its Use for Screening Methods
Institut für Physiologie FML Weihenstephan Technische Universität München Expression of recombinant human androgen receptor and its use for screening methods Ellinor Rose Sigrid Bauer Vollständiger Abdruck der von der Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt der Technischen Universität München zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigten Dissertation. Vorsitzender: Univ.-Prof. Dr. B. Hock Prüfer der Dissertation: Univ.-Prof. Dr. H. H. D. Meyer Univ.-Prof. Dr. H. Sauerwein (Rheinische Friedrich-Wilhelms-Universität Bonn) Die Dissertation wurde am 31.10.2002 bei der Technischen Universität München eingereicht und durch die Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt am 03.12.2002 angenommen. Introduction Content 1. INTRODUCTION ..................................................................................................................................... 5 1.1. ENDOCRINE DISRUPTERS 5 1.2. ANDROGENS AND ANTIANDROGENS 7 1.2.1. DEFINITIONS 7 1.2.2. MODE OF ACTION 8 1.3. STRUCTURES OF ENDOCRINE DISRUPTERS 10 1.4. STRATEGIES FOR MONITORING ANDROGEN ACTIVE SUBSTANCES 13 1.4.1. IN VIVO METHODS 13 1.4.2. IN VITRO METHODS 15 1.5. OBJEKTIVE OF THE STUDIES 18 2. MATERIALS AND METHODS ................................................................................................................. 19 2.1. PREPARATION OF RECEPTORS 19 2.2. ASSAY SYSTEMS 19 2.2.1. IN SOLUTION AR ASSAY 19 2.2.2. IMMUNO-IMMOBILISED RECEPTOR ASSAY (IRA) 20 2.2.3. PR AND SHBG ASSAYS 21 2.2.4. DATA EVALUATION 21 2.3. ANALYTES 22 3. RESULTS AND DISCUSSION ................................................................................................................. 23 3.1. DEVELOPMENT OF NEW ASSAY SYSTEMS 23 3.1.1. BAR ASSAY 23 3.1.2. CLONING OF THE HUMAN AR AND PRODUCTION OF FUNCTIONAL PROTEIN 24 3.1.3. DEVELOPMENT OF A SCREENING ASSAY ON MICROTITRE PLATES (IRA) 25 3.2. -

Inbrija, INN-Levodopa
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Inbrija 33 mg inhalation powder, hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each hard capsule contains 42 mg levodopa. Each delivered dose contains 33 mg levodopa. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Inhalation powder, hard capsule. White opaque capsules containing white powder, with “A42” printed in black on the cap of the capsule and two black bands printed on the body of the capsule. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Inbrija is indicated for the intermittent treatment of episodic motor fluctuations (OFF episodes) in adult patients with Parkinson’s disease (PD) treated with a levodopa/dopa-decarboxylase inhibitor. 4.2 Posology and method of administration Posology Patients should be on a stable levodopa/dopa-decarboxylase inhibitor (e.g. carbidopa or benserazide) regimen before starting Inbrija. Patients selected for treatment with Inbrija should be able to recognize the onset of their 'OFF' symptoms and be capable of preparing the inhaler or else have a responsible care giver able to prepare the inhaler for them when required. Inbrija should be inhaled when symptoms, motor or non-motor, of an OFF period start to return. The recommended dose of Inbrija is 2 hard capsules up to 5 times per day each delivering 33 mg levodopa. The maximum daily dose of Inbrija should not exceed 10 capsules (330 mg). It is not recommended to take more than 2 capsules per OFF period. Exceeding the recommended dose may lead to increased levodopa associated adverse reactions. -

207145Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 207145Orig1s000 OTHER REVIEW(S) CSS Consult: NDA 207,145 Safinamide M E M O R A N D U M Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research * Date: March 8, 2017 To: Billy Dunn, M.D., Director Division of Neurology Products Through: Martin Rusinowitz, M.D., Medical Officer Silvia Calderon, Ph.D., Pharmacologist Controlled Substance Staff From: Alicja Lerner, M.D., Ph.D., Medical Officer Controlled Substance Staff Subject: Erratum-CSS Review of NDA 207,145 dated December 29, 2016 (Author: Lerner, Alicja) AMENDMENT This memorandum corrects an error and changes the title of Table 4, page 14, in the previously submitted CSS review dated Dec 29, 2016. In our prior review, we erroneously listed the subject population reporting the tabulated adverse events as comprising only healthy volunteers (HV). However, as indicated in the revised Table Title, the data derived from Phase 2 and Phase 3 controlled trials. This erratum does not change the conclusions or recommendations in the previous CSS review. Table 4 should read: Table 4. Summary of Selected Abuse Potential Adverse Events from all Completed Safinamide Phase 2 and Phase 3 Controlled Trials for PD – All Pooled Studies (based on the table 11, page 27, 8 factor-analysis). 1 of 2 Reference ID: 4066812 CSS Consult: NDA 207,145 Safinamide Body System Or Organ Class All Safinamide Placebo pool pool N=919 N=1516 (n, %) (n, %) Patients with at least one abuse potential event 230 (15.2) -
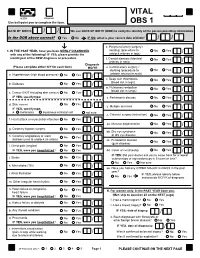
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd. -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -

Specialty Drug Benefit Document
Louisiana Healthcare Connections Specialty Drug Benefit ouisiana Healthcare Connections provides coverage of a number of specialty drugs. All specialty drugs, such as biopharmaceuticals and injectables, require a prior authorization (PA) to be approved for L payment by Louisiana Healthcare Connections. PA requirements are programmed specific to the drug. Since the list of specialty drugs changes over time due to new drug arrivals and other market conditions, it is important to contact Provider Services at 1-866-595-8133 or check the Louisiana Healthcare Connections website at www.LouisianaHealthConnect.com for updates to this benefit. Requests for specialty drugs can be submitted to Louisiana Healthcare Connections by filling out the Medication Prior Authorization Form that is available on the Louisiana Healthcare Connections website at www.LouisianaHealthConnect.com and faxing the request as instructed on the form. Louisiana Healthcare Connections members can receive the specialty drugs they require at any outpatient pharmacy enrolled in our pharmacy network that can supply specialty drugs. Providers that wish to have drugs distributed by a SPECIALTY PHARMACY should FAX the request to 1-866-399-0929 for review. If a provider wishes to dispense a specialty drug from OFFICE STOCK, the provider should FAX the request to Louisiana Healthcare Connections at 1-877-401-8172 for review. BRAND NAME INGREDIENTS SPECIAL INSTRUCTIONS ACTEMRA TOCILIZUMAB ACTHAR HP CORTICOTROPIN ACTIMMUNE INTERFERON GAMMA-1B ADAGEN PEGADEMASE BOVINE Limited Distribution -

Highlights of Prescribing Information
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gastrointestinal Perforation: Increased risk in patients with certain GI These highlights do not include all the information needed to use disorders; Signs and symptoms may be masked (5.4) ® EMFLAZA safely and effectively. See full prescribing information for • Behavioral and Mood Disturbances: May include euphoria, insomnia, EMFLAZA. mood swings, personality changes, severe depression, and psychosis (5.5) • Effects on Bones: Monitor for decreases in bone mineral density with EMFLAZA® (deflazacort) tablets, for oral use EMFLAZA® (deflazacort) oral suspension chronic use of EMFLAZA (5.6) Initial U.S. Approval: 2017 • Ophthalmic Effects: May include cataracts, infections, and glaucoma; Monitor intraocular pressure if EMFLAZA is continued for more than 6 ---------------------------INDICATIONS AND USAGE--------------------------- weeks (5.7) EMFLAZA is a corticosteroid indicated for the treatment of Duchenne muscular dystrophy (DMD) in patients 2 years of age and older (1) • Vaccination: Do not administer live or live attenuated vaccines to patients receiving immunosuppressive doses of corticosteroids. Administer live- ----------------------DOSAGE AND ADMINISTRATION---------------------- attenuated or live vaccines at least 4 to 6 weeks prior to starting • The recommended once-daily dosage is approximately 0.9 mg/kg/day EMFLAZA (5.8) administered orally (2.2) • Serious Skin Rashes: Discontinue at the first sign of rash, unless the rash is • Discontinue gradually when administered for more than a few -

Comparative Effects of Anti-Inflammatory Corticosteroids in Human Bone-Derived Osteoblast-Like Cells
Copyright ©ERS Journals Ltd 1998 Eur Respir J 1998; 12: 1327–1333 European Respiratory Journal DOI: 10.1183/09031936.98.12061327 ISSN 0903 - 1936 Printed in UK - all rights reserved Comparative effects of anti-inflammatory corticosteroids in human bone-derived osteoblast-like cells H. Namkung-Matthäi*, J.P. Seale**, K. Brown***, R.S. Mason* aa Comparative effects of anti-inflammatory corticosteroids in human bone-derived osteo- Depts of *Physiology and Institute for blast- like cells. H. Namkung-Matthäi, J.P. Seale, K. Brown, R.S. Mason. ©ERS Journals Ltd Biomedical Research, **Pharmacology and 1998. ***Pharmacy, University of Sydney, Aus- ABSTRACT: While effects of inhaled corticosteroids on serum markers of bone tralia. metabolism in normal and asthmatic subjects have been reported, there are little data Correspondence: R.S. Mason on the direct effects of these corticosteroids on end-organs such as bone. The results Dept of Physiology and Institute for Bio- presented here compare the effects of budesonide and its epimers (22S- and 22R- medical Research budesonide), fluticasone and dexamethasone on growth and differentiation of cul- University of Sydney tured human bone cells. NSW 2006 Osteoblast-like cells were cultured from human foetal bone chips grown to conflu- Australia ence and used at first subculture. Fax: 61 293512058 At concentrations of 10-11–10-7 M each corticosteroid (CS) caused a dose-dependent Keywords: Alkaline phosphatase decrease in [3H]thymidine incorporation into deoxyribonucleic acid (DNA), median bioactivity effective concentration (EC50): fluticasone (0.06 nM) >22R (0.26 nM) >22S (0.4 nM) bone-derived cells >budesonide (0.47 nM) >dexamethasone (1.5 nM).