View Board (#17–0011)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
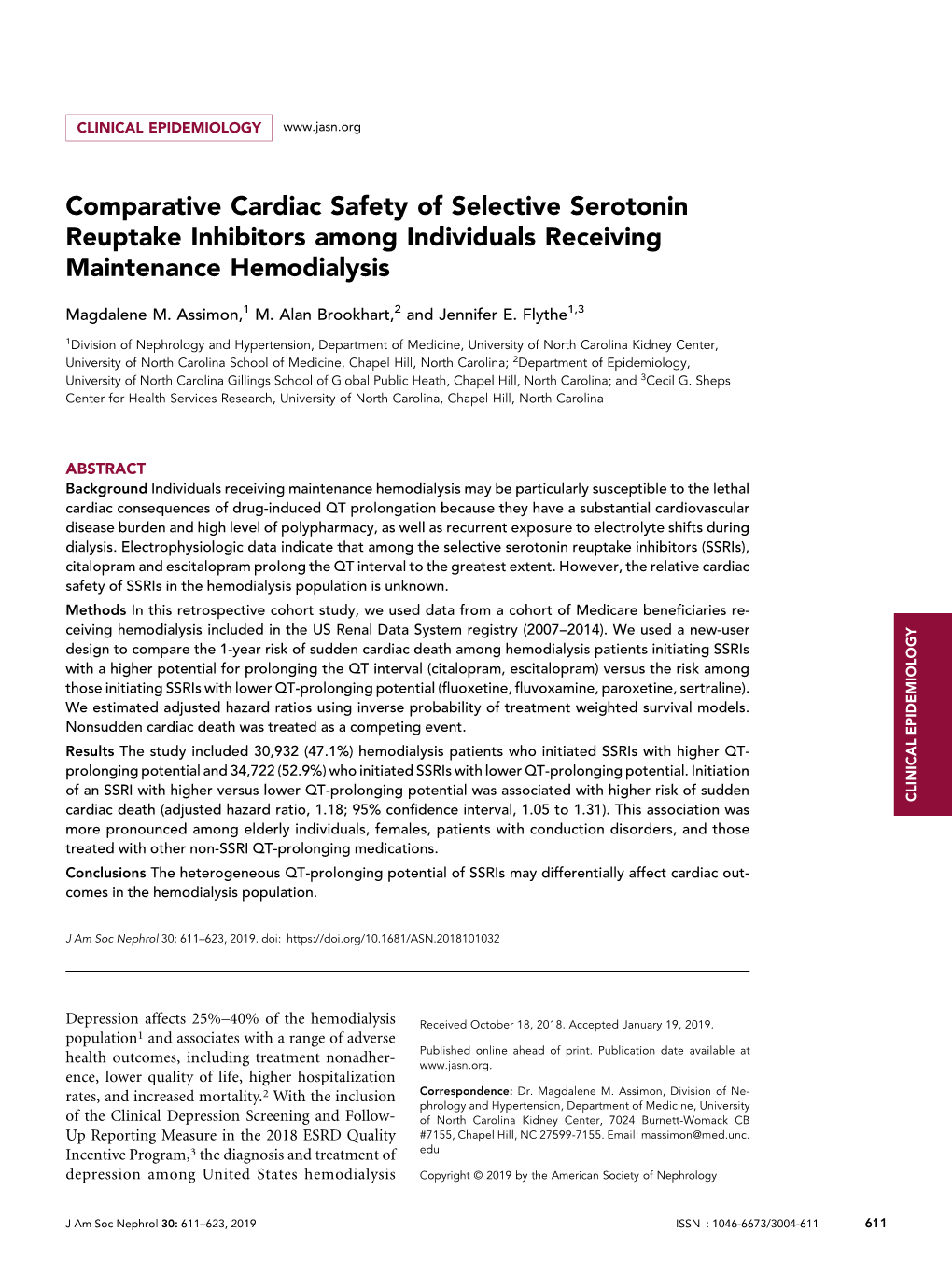
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2012 Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors Marisa Rosenberg Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2715 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. ANTINOCICEPTIVE EFFECTS OF MONOAMINE REUPTAKE INHIBITORS IN ASSAYS OF PAIN-STIMULATED AND PAIN-DEPRESSED BEHAVIOR A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Marisa B. Rosenberg Bachelor of Science, Temple University, 2008 Advisor: Sidney Stevens Negus, Ph.D. Professor, Department of Pharmacology/Toxicology Virginia Commonwealth University Richmond, VA May, 2012 Acknowledgement First and foremost, I’d like to thank my advisor Dr. Steven Negus, whose unwavering support, guidance and patience throughout my graduate career has helped me become the scientist I am today. His dedication to education, learning and the scientific process has instilled in me a quest for knowledge that I will continue to pursue in life. His thoroughness, attention to detail and understanding of pharmacology has been exemplary to a young person like me just starting out in the field of science. I’d also like to thank all of my committee members (Drs. -
Multi-Residue Automated Turbulent Flow Online LC-MS/MS Method for the Determination of Antibiotics in Milk
Multi-residue Automated Turbulent Flow 63551 Method: Online LC-MS/MS Method for the Determination of Antibiotics in Milk Katerina Bousova, Klaus Mittendorf, Thermo Fisher Scientific Food Safety Response Center, Dreieich, Germany Key Words Transcend TLX, TSQ Quantum Access MAX, Antibiotics, Food Safety, Milk, TurboFlow Technology 1. Schematic of Method Sample Shaking 1. Weigh 500 mg of shaken milk into 2 mL centrifuge tube Sample 500 mg + IS 2. Add 450 µL acetonitrile and 50 µL working IS solution 3. Vortex sample for 5 minutes Extraction 4. Centrifuge sample with 12,000 rpm for 5 minutes For fast screening of antibiotics, microbiological or bioassay techniques are widely used. These techniques 5. Filter sample through 0.45 µm nylon microfilter are not able to distinguish between the different types of antibiotics and provide only a semi-quantitative result Centrifugation and Filtration for the total amount of drug residues. The big drawback is the incidence of false-negative or false-positive results 6. Inject into TLX-LC-MS/MS because of low sensitivity and specificity. However, these screening assays are still very popular and widely used Turbulent Flow LC-MS/MS because of their cost-effectiveness and speed of analysis. For quantitative analysis it is necessary to use instrumental techniques such as LC-MS/MS. This 2. Introduction technique can also be used for screening, and provides Antibiotics are a group of chemicals that are widely used much higher sensitivity and greater specificity. The in animal husbandry primarily for protection of animals use of LC-MS/MS for screening was described in a from disease but also as growth promoters. -

Dexmedetomidine)
Frequently asked questions regarding alpha-2 agonist DEXDOMITOR® (dexmedetomidine) Q: How should I monitor a patient that has received DEXDOMITOR for sedation or as a premedication? A: The monitoring of vital signs is critical for any patient under sedation or anesthesia. It is important to monitor heart rate, blood pressure, palpable pulse quality, and respiratory rate and volume. Because a2 agonists cause peripheral vasoconstriction, the use of pulse oximetry may not adequately reflect the true status of the patient. Q: What can I expect to see in a patient under DEXDOMITOR sedation? A: The patient may have pale pink or grayish mucous membranes because of peripheral vasoconstriction. The sedation induced by DEXDOMITOR causes a decrease in respiratory rate and a lower body temperature. Q: What is considered a low heart rate? A: Because of the wide range of dog sizes and corresponding heart rates, normal heart rates should be based on the dog’s body size. A reduction in heart rate following a2 agonist sedation should be expected. Patient status should be evaluated by the simultaneous measurement of many parameters, including pulse quality, respiratory rate and quality, blood pressure, and heart rate. Q: What is the effect on the respiratory rate? A: DEXDOMITOR does not have a direct effect on respiration. Although the respiratory rate may decrease as a result of sedation, ventilatory volume generally increases, and overall ventilation (gas exchange) remains stable. Q: I am concerned about hypothermia. A: Hypothermia can occur in a patient following administration of any anesthetic or sedative drug. It is important that body temperature be maintained in all patients undergoing anesthesia or sedation, including those that receive an a2 agonist. -

Serotonin 2A Activation and a Novel Therapeutic Drug
Psychopharmacology (2018) 235:3083–3091 https://doi.org/10.1007/s00213-018-5042-1 THEORETICAL AND METHODOLOGICAL PERSPECTIVE The neuropharmacology of sleep paralysis hallucinations: serotonin 2A activation and a novel therapeutic drug Baland Jalal1 Received: 23 April 2018 /Accepted: 17 September 2018 /Published online: 5 October 2018 # The Author(s) 2018 Abstract Sleep paralysis is a state of involuntary immobility occurring at sleep onset or offset, often accompanied by uncanny Bghost-like^ hallucinations and extreme fear reactions. I provide here a neuropharmacological account for these hallucinatory experiences by evoking the role of the serotonin 2A receptor (5-HT2AR). Research has shown that 5-HT2AR activation can induce visual hallucinations, Bmystical^ subjective states, and out-of-body experiences (OBEs), and modulate fear circuits. Hallucinatory experiences triggered by serotonin—serotonergic (Bpseudo^) hallucinations, induced by hallucinogenic drugs—tend to be Bdream-like^ with the experiencer having insight (Bmeta-awareness^) that he is hallucinating, unlike dopaminergic (Bpsychotic^ and Blife-like^) hallucinations where such insight is lost. Indeed, hallucinatory experiences during sleep paralysis have the classic features of serotonergic hallucinations, and are strikingly similar to perceptual and subjective states induced by hallucinogenic drugs (e.g., lysergic acid diethylamide [LSD] and psilocybin), i.e., they entail visual hallucinations, mystical experiences, OBEs, and extreme fear reactions. I propose a possible mechanism whereby serotonin could be functionally implicated in generating sleep paralysis hallucinations and fear reactions through 5-HT2AR activity. Moreover, I speculate on the role of 5-HT2C receptors vis-à-vis anxiety and panic during sleep paralysis, and the orbitofrontal cortex—rich with 5-HT2A receptors—in influencing visual pathways during sleep paralysis, and, in effect, hallucinations. -

Meta-Analysis of the Dose-Response Relationship of SSRI in Obsessive
Molecular Psychiatry (2010) 15, 850–855 & 2010 Macmillan Publishers Limited All rights reserved 1359-4184/10 www.nature.com/mp ORIGINAL ARTICLE Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder MH Bloch1, J McGuire1, A Landeros-Weisenberger1, JF Leckman1 and C Pittenger2 1Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA and 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA We sought to determine differences in efficacy and tolerability between different doses of selective serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder (OCD) using meta-analysis. We identified 9 studies involving 2268 subjects that were randomized, double-blind placebo-controlled clinical trials that compared multiple, fixed- doses of selective serotonin reuptake inhibitors (SSRIs) to each other and to placebo in the treatment of adults with OCD. Change in Y-BOCS score, proportion of treatment responders, and dropouts (all-cause and due to side-effects) were determined for each included study. Weighted mean difference was used to examine mean change in Y-BOCS score. Pooled absolute risk difference was used to examine dichotomous outcomes. Meta-analysis was performed using a fixed effects model in RevMan 4.2.8. We found that compared with either low or medium doses, higher doses of SSRIs were associated with improved treatment efficacy, using either Y-BOCS score or proportion of treatment responders as an outcome. Dose of SSRIs was not associated with the number of all-cause dropouts. Higher doses of SSRIs were associated with significantly higher proportion of dropouts due to side-effects. -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -

Atypical Antipsychotics TCO 02.2018
Therapeutic Class Overview Atypical Antipsychotics INTRODUCTION • Antipsychotic medications have been used for over 50 years to treat schizophrenia and a variety of other psychiatric disorders (Miyamato et al 2005). • Antipsychotic medications generally exert their effect in part by blocking dopamine (D)-2 receptors (Jibson et al 2017). • Antipsychotics are divided into 2 distinct classes based on their affinity for D2 and other neuroreceptors: typical antipsychotics, also called first-generation antipsychotics (FGAs), and atypical antipsychotics, also called second- generation antipsychotics (SGAs) (Miyamato et al 2005). • Atypical antipsychotics do not have a uniform pharmacology or mechanism of action; these differences likely account for the different safety and tolerability profiles of these agents (Clinical Pharmacology 2020, Jibson et al 2017). The atypical antipsychotics differ from the early antipsychotics in that they have affinity for the serotonin 5-HT2 receptor in addition to D2. Clozapine is an antagonist at all dopamine receptors (D1-5), with lower affinity for D1 and D2 receptors and high affinity for D4 receptors. Aripiprazole and brexpiprazole act as partial agonists at the D2 receptor, functioning as an ○ agonist when synaptic dopamine levels are low and as an antagonist when they are high. Cariprazine is a partial agonist at D2 and D3. Pimavanserin does not have dopamine blocking activity and is primarily an inverse agonist at 5-HT2A receptors. The remaining atypical antipsychotics share the similarity of D2 and 5-HT2A -

M2021: Pharmacogenetic Testing
Pharmacogenetic Testing Policy Number: AHS – M2021 – Pharmacogenetic Prior Policy Name and Number, as applicable: Testing • M2021 – Cytochrome P450 Initial Presentation Date: 06/16/2021 Revision Date: N/A I. Policy Description Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome (CYP) P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. CYP P450 are essential to produce many biochemical building blocks, such as cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in CYP P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased levels of toxic substances in the body. Approximately 58 CYP genes are in humans (Bains, 2013; Tantisira & Weiss, 2019). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. Azathioprine and mercaptopurine are used for treatment of nonmalignant immunologic disorders; mercaptopurine is used for treatment of lymphoid malignancies; and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011). Dihydropyrimidine dehydrogenase (DPD), encoded by the gene DPYD, is a rate-limiting enzyme responsible for fluoropyrimidine catabolism. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors, such as colorectal, breast, and aerodigestive tract tumors (Amstutz et al., 2018). A variety of cell surface proteins, such as antigen-presenting molecules and other proteins, are encoded by the human leukocyte antigen genes (HLAs). -
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
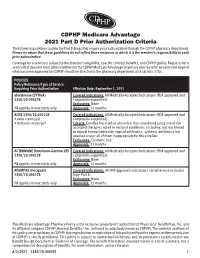
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -
TAYSIDE PRESCRIBER Issue No
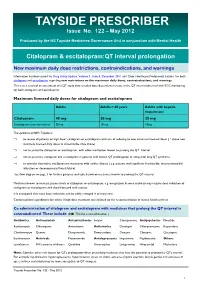
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Deutetrabenazine
PATIENT & CAREGIVER EDUCATION Deutetrabenazine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Austedo Warning This drug may raise the chance of depression and suicidal thoughts or actions in people with Huntington’s disease. If you have ever had depression or suicidal thoughts or actions, talk with your doctor. This drug may not be right for you. People who take this drug must be watched closely. Call your doctor right away if you have signs like depression, nervousness, restlessness, grouchiness, panic attacks, or any other changes in feelings, mood, or behavior. Call your doctor right away if you have any thoughts or actions of suicide. What is this drug used for? It is used to treat disabling involuntary movements in Huntington’s chorea. It is used to treat tardive dyskinesia. What do I need to tell my doctor BEFORE I take this drug? If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have or have ever had depression or thoughts of suicide. Deutetrabenazine 1/6 If you have liver disease. If you have ever had a long QT on ECG or other heartbeat that is not normal. If you have taken certain drugs for depression or Parkinson’s disease in the last 14 days. This includes isocarboxazid, phenelzine, tranylcypromine, selegiline, or rasagiline.