Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Does the Antidepressant-Like Effect of Mirtazapine and Venlafaxine Differ Between Male and Female Rats?
ORIGINAL ARTICLE Volume 43, Issue 1, January-February 2020 doi: 10.17711/SM.0185-3325.2020.002 Does the antidepressant-like effect of mirtazapine and venlafaxine differ between male and female rats? Adriana Álvarez Silva,1 Alonso Fernández-Guasti1 1 Departamento de Farmacobiología, ABSTRACT Centro de Investigación y de Estu- dios Avanzados del Instituto Politécni- Depression is a global health problem with nearly 350 million people affected, mainly women. co Nacional, Ciudad de México, Introduction. México. However, nowadays a rising amount of men are being diagnosed. This makes necessary the screening of new treatment options that are effective in women as well as in men. Objective. To analyze if the administration of Correspondence: mirtazapine and venlafaxine to male and female rats shows a sex-related antidepressant-like effect, and the Alonso Fernández-Guasti Laboratorio de Farmacología possible associated neurochemical mechanisms. Method. Mirtazapine (40 mg/kg) or venlafaxine (60 mg/kg) Conductual, Centro de Investigación were administered subchronically to young adult male and female (ovariectomized and steroid-primed) rats, y de Estudios Avanzados del Instituto and their antidepressant-like effects were evaluated using the forced swim test (FST). The active behaviors, Politécnico Nacional. swimming and climbing, were also analyzed. a) mirtazapine and venlafaxine reduced immobility Calzada de los Tenorios 235, Results. Col Granjas Coapa, in the FST in males and females; b) both antidepressants increased climbing and swimming in male rats; Alcaldía Tlalpan, c) in female rats, mirtazapine and venlafaxine only increased swimming. Discussion and conclusion. In 14330, Ciudad de México, México. males, the effects of mirtazapine and venlafaxine seem to be produced by the activation of the serotonergic Phone: +52 (55) 5483 - 2848 and noradrenergic systems. -

Dopamine Reuptake Transporter (DAT) “Inverse Agonism” E Anovel 66 2 67 3 Hypothesis to Explain the Enigmatic Pharmacology of Cocaine 68 4 * 69 5 Q5 David J
NP5526_proof ■ 24 June 2014 ■ 1/22 Neuropharmacology xxx (2014) 1e22 55 Contents lists available at ScienceDirect 56 57 Neuropharmacology 58 59 60 journal homepage: www.elsevier.com/locate/neuropharm 61 62 63 64 65 1 Dopamine reuptake transporter (DAT) “inverse agonism” e Anovel 66 2 67 3 hypothesis to explain the enigmatic pharmacology of cocaine 68 4 * 69 5 Q5 David J. Heal , Jane Gosden, Sharon L. Smith 70 6 71 RenaSci Limited, BioCity, Pennyfoot Street, Nottingham NG1 1GF, UK 7 72 8 73 9 article info abstract 74 10 75 11 76 Article history: The long held view is cocaine's pharmacological effects are mediated by monoamine reuptake inhibition. 12 Available online xxx However, drugs with rapid brain penetration like sibutramine, bupropion, mazindol and tesofensine, 77 13 which are equal to or more potent than cocaine as dopamine reuptake inhibitors, produce no discernable 78 14 Keywords: subjective effects such as drug “highs” or euphoria in drug-experienced human volunteers. Moreover 79 15 Cocaine they are dysphoric and aversive when given at high doses. In vivo experiments in animals demonstrate 80 16 Dopamine reuptake inhibitor that cocaine's monoaminergic pharmacology is profoundly different from that of other prescribed 81 Dopamine releasing agent 17 monoamine reuptake inhibitors, with the exception of methylphenidate. These findings led us to 82 Dopamine transporter fi 18 Inverse agonist conclude that the highly unusual, stimulant pro le of cocaine and related compounds, eg methylphe- 83 19 DAT inverse agonist nidate, is not mediated by monoamine reuptake inhibition alone. 84 We describe the experimental findings which suggest cocaine serves as a negative allosteric 20 Novel mechanism 85 21 modulator to alter the function of the dopamine reuptake transporter (DAT) and reverse its direction of fi 86 22 transport. -
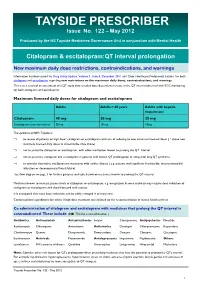
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Compositions and Methods for Selective Delivery of Oligonucleotide Molecules to Specific Neuron Types
(19) TZZ ¥Z_T (11) EP 2 380 595 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 26.10.2011 Bulletin 2011/43 A61K 47/48 (2006.01) C12N 15/11 (2006.01) A61P 25/00 (2006.01) A61K 49/00 (2006.01) (2006.01) (21) Application number: 10382087.4 A61K 51/00 (22) Date of filing: 19.04.2010 (84) Designated Contracting States: • Alvarado Urbina, Gabriel AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Nepean Ontario K2G 4Z1 (CA) HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL • Bortolozzi Biassoni, Analia Alejandra PT RO SE SI SK SM TR E-08036, Barcelona (ES) Designated Extension States: • Artigas Perez, Francesc AL BA ME RS E-08036, Barcelona (ES) • Vila Bover, Miquel (71) Applicant: Nlife Therapeutics S.L. 15006 La Coruna (ES) E-08035, Barcelona (ES) (72) Inventors: (74) Representative: ABG Patentes, S.L. • Montefeltro, Andrés Pablo Avenida de Burgos 16D E-08014, Barcelon (ES) Edificio Euromor 28036 Madrid (ES) (54) Compositions and methods for selective delivery of oligonucleotide molecules to specific neuron types (57) The invention provides a conjugate comprising nucleuc acid toi cell of interests and thus, for the treat- (i) a nucleic acid which is complementary to a target nu- ment of diseases which require a down-regulation of the cleic acid sequence and which expression prevents or protein encoded by the target nucleic acid as well as for reduces expression of the target nucleic acid and (ii) a the delivery of contrast agents to the cells for diagnostic selectivity agent which is capable of binding with high purposes. -
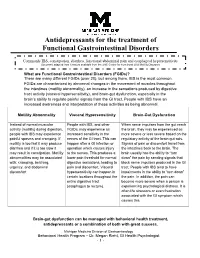
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

(12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed Et Al
US0078.93053B2 (12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed et al. (45) Date of Patent: Feb. 22, 2011 (54) TREATING PSYCHOLOGICAL CONDITIONS WO WO 2006/127418 11, 2006 USING MUSCARINIC RECEPTORM ANTAGONSTS (75) Inventors: Brian Seed, Boston, MA (US); Jordan OTHER PUBLICATIONS Mechanic, Sunnyvale, CA (US) Chau et al. (Nucleus accumbens muscarinic receptors in the control of behavioral depression : Antidepressant-like effects of local M1 (73) Assignee: Theracos, Inc., Sunnyvale, CA (US) antagonist in the porSolt Swim test Neuroscience vol. 104, No. 3, pp. 791-798, 2001).* (*) Notice: Subject to any disclaimer, the term of this Lind et al. (Muscarinic acetylcholine receptor antagonists inhibit patent is extended or adjusted under 35 chick Scleral chondrocytes Investigative Ophthalmology & Visual U.S.C. 154(b) by 726 days. Science, vol.39, 2217-2231.* Chau D., et al., “Nucleus Accumbens Muscarinic Receptors in the (21) Appl. No.: 11/763,145 Control of Behavioral Depression: Antidepressant-like Effects of Local M1 Antagonists in the Porsolt Swin Test.” Neuroscience, vol. (22) Filed: Jun. 14, 2007 104, No. 3, Jun. 14, 2001, pp. 791-798. Bechtel, W.D., et al., “Biochemical pharmacology of pirenzepine. (65) Prior Publication Data Similarities with tricyclic antidepressants in antimuscarinic effects only.” Arzneimittelforschung, vol. 36(5), pp. 793-796 (May 1986). US 2007/O293480 A1 Dec. 20, 2007 Chau, D.T. et al., “Nucleus accumbens muscarinic receptors in the control of behavioral depression: antidepressant-like effects of local Related U.S. Application Data Mantagonist in the Porsolt Swim test.” Neuroscience, vol. 104(3), (60) Provisional application No. -

Mechanism of Action of Antidepressants and Mood Stabilizers
79 MECHANISM OF ACTION OF ANTIDEPRESSANTS AND MOOD STABILIZERS ROBERT H. LENOX ALAN FRAZER Bipolar disorder (BPD), the province of mood stabilizers, the more recent understanding that antidepressants share has long been considered a recurrent disorder. For more this property in UPD have focused research on long-term than 50 years, lithium, the prototypal mood stabilizer, has events, such as alterations in gene expression and neuroplas- been known to be effective not only in acute mania but ticity, that may play a significant role in stabilizing the clini- also in the prophylaxis of recurrent episodes of mania and cal course of an illness. In our view, behavioral improvement depression. By contrast, the preponderance of past research and stabilization stem from the acute pharmacologic effects in depression has focused on the major depressive episode of antidepressants and mood stabilizers; thus, both the acute and its acute treatment. It is only relatively recently that and longer-term pharmacologic effects of both classes of investigators have begun to address the recurrent nature of drugs are emphasized in this chapter. unipolar disorder (UPD) and the prophylactic use of long- term antidepressant treatment. Thus, it is timely that we address in a single chapter the most promising research rele- vant to the pharmacodynamics of both mood stabilizers and MOOD STABILIZERS antidepressants. As we have outlined in Fig. 79.1, it is possible to charac- The term mood stabilizer within the clinical setting is com- terize both the course and treatment of bipolar and unipolar monly used to refer to a class of drugs that treat BPD. -

Problems of Drug Dependence 1982 Proceedings of the 44Th Annual Scientific Meeting The
National Institute Drug Abuse MONOGRAPH SERIES Problems of Drug Dependence 1982 Proceedings of the 44th Annual Scientific Meeting The Committee on Problems of Drug Dependence, Inc. U. S. DEPARTMENT OF HEALTH AND HUMAN SERVICE • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration Problems of Drug Dependence, 1982 Proceedings of the 44th Annual Scientific Meeting, The Committee on Problems of Drug Dependence, Inc. Editor, Louis S. Harris, Ph.D. NIDA Research Monograph 43 April 1983 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse Office of Science 5600 Fishers Lane Rockville, Maryland 20657 NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art confer- ences, integrative research reviews and significant original research. Its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisory Board Avram Goldstein, M.D. Addiction Research Foundation Palo Alto, California Jerome Jaffe, M.D. University of Connecticut School of Medicine Farmington, Connecticut Reese T. Jones, M.D. Langley Porter Neuropsychiatric Institute University of California San Francisco, California Jack Mendelson, M.D. Alcohol and Drug Abuse Research Center Harvard Medical School McLean Hospital Belmont, Massachusetts Helen Nowlis, Ph.D. Rochester, New York Lee Robins, Ph.D. Washington University School of Medicine St. Louis, Missouri NIDA Research Monograph Series William Pollin, M.D. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -
Expansion of a Cheminformatic Database of Spectral Data for Forensic Chemists and Toxicologists
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Expansion of a Cheminformatic Database of Spectral Data for Forensic Chemists and Toxicologists Author(s): Peter Stout, Katherine Moore, Megan Grabenauer, Jeri Ropero-Miller Document No.: 241444 Date Received: March 2013 Award Number: 2010-DN-BX-K177 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this Federally- funded grant report available electronically. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. Award Number: 2010-DN-BX-K177 July 16, 2012 Expansion of a Cheminformatic Database of Spectral Data for Forensic Chemists and Toxicologists Final Report Authors: Peter Stout Katherine Moore Megan Grabenauer Jeri Ropero-Miller This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. Expansion of a Cheminformatic Database of Spectral Data for Forensic Chemists and Toxicologists Table of Contents Abstract ........................................................................................................................................... 1 Executive Summary ....................................................................................................................... -

Director's Report 2/01
Director's Report 2/01 Director's Report to the National Advisory Council on Drug Abuse February, 2001 Index Research Findings Basic Research Behavioral Research Treatment Research and Development Research on AIDS and Other Medical Consequences of Drug Abuse Epidemiology, Etiology and Prevention Research Services Research Intramural Research Program Activities Extramural Policy and Review Activities Congressional Affairs International Activities Meetings and Conferences Media and Education Activities Planned Meetings Publications Staff Highlights Grantee Honors [Office of Director] [First Report Section] Archive Home | Accessibility | Privacy | FOIA (NIH) | Current NIDA Home Page The National Institute on Drug Abuse (NIDA) is part of the National Institutes of Health (NIH) , a component of the U.S. Department of Health and Human Services. Questions? _ See our Contact Information. https://archives.drugabuse.gov/DirReports/DirRep201/DirectorRepIndex.html[11/17/16, 9:48:57 PM] Director's Report 2/01 - Basic Research Director's Report to the National Advisory Council on Drug Abuse February, 2001 Research Findings Basic Research Role for GDNF in Biochemical and Behavioral Adaptations to Drugs of Abuse Drs. David Russell and Eric Nestler and their research team at the Yale University examined a role for Glial-Derived Neurotrophic Factor (GDNF) in adaptations to drugs of abuse. Infusion of GDNF into the ventral tegmental area (VTA), a dopaminergic brain region important for addiction, blocks certain biochemical adaptations to chronic cocaine or morphine as well as the rewarding effects of cocaine. Conversely, responses to cocaine are enhanced in rats by intra-VTA infusion of an anti-GDNF antibody and in mice heterozygous for a null mutation in the GDNF gene.