Antidepressants for Functional Gastrointestinal Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2012 Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors Marisa Rosenberg Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2715 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. ANTINOCICEPTIVE EFFECTS OF MONOAMINE REUPTAKE INHIBITORS IN ASSAYS OF PAIN-STIMULATED AND PAIN-DEPRESSED BEHAVIOR A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Marisa B. Rosenberg Bachelor of Science, Temple University, 2008 Advisor: Sidney Stevens Negus, Ph.D. Professor, Department of Pharmacology/Toxicology Virginia Commonwealth University Richmond, VA May, 2012 Acknowledgement First and foremost, I’d like to thank my advisor Dr. Steven Negus, whose unwavering support, guidance and patience throughout my graduate career has helped me become the scientist I am today. His dedication to education, learning and the scientific process has instilled in me a quest for knowledge that I will continue to pursue in life. His thoroughness, attention to detail and understanding of pharmacology has been exemplary to a young person like me just starting out in the field of science. I’d also like to thank all of my committee members (Drs. -

FDA Warns About an Increased Risk of Serious Pancreatitis with Irritable Bowel Drug Viberzi (Eluxadoline) in Patients Without a Gallbladder
FDA warns about an increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder Safety Announcement [03-15-2017] The U.S. Food and Drug Administration (FDA) is warning that Viberzi (eluxadoline), a medicine used to treat irritable bowel syndrome with diarrhea (IBS-D), should not be used in patients who do not have a gallbladder. An FDA review found these patients have an increased risk of developing serious pancreatitis that could result in hospitalization or death. Pancreatitis may be caused by spasm of a certain digestive system muscle in the small intestine. As a result, we are working with the Viberzi manufacturer, Allergan, to address these safety concerns. Patients should talk to your health care professional about how to control your symptoms of irritable bowel syndrome with diarrhea (IBS-D), particularly if you do not have a gallbladder. The gallbladder is an organ that stores bile, one of the body’s digestive juices that helps in the digestion of fat. Stop taking Viberzi right away and get emergency medical care if you develop new or worsening stomach-area or abdomen pain, or pain in the upper right side of your stomach-area or abdomen that may move to your back or shoulder. This pain may occur with nausea and vomiting. These may be symptoms of pancreatitis, an inflammation of the pancreas, an organ important in digestion; or spasm of the sphincter of Oddi, a muscular valve in the small intestine that controls the flow of digestive juices to the gut. Health care professionals should not prescribe Viberzi in patients who do not have a gallbladder and should consider alternative treatment options in these patients. -

Therapeutic Class Overview Irritable Bowel Syndrome Agents
Therapeutic Class Overview Irritable Bowel Syndrome Agents Therapeutic Class Overview/Summary: This review will focus on agents used for the treatment of Irritable Bowel Syndrome (IBS).1-5 IBS is a gastrointestinal syndrome characterized primarily by non-specific chronic abdominal pain, usually described as a cramp-like sensation, and abnormal bowel habits, either constipation or diarrhea, in which there is no organic cause. Other common gastrointestinal symptoms may include gastroesophageal reflux, dysphagia, early satiety, intermittent dyspepsia and nausea. Patients may also experience a wide range of non-gastrointestinal symptoms. Some notable examples include sexual dysfunction, dysmenorrhea, dyspareunia, increased urinary frequency/urgency and fibromyalgia-like symptoms.6 IBS is defined by one of four subtypes. IBS with constipation (IBS-C) is the presence of hard or lumpy stools with ≥25% of bowel movements and loose or watery stools with <25% of bowel movements. When IBS is associated with diarrhea (IBS-D) loose or watery stools are present with ≥25% of bowel movements and hard or lumpy stools are present with <25% of bowel movements. Mixed IBS (IBS-M) is defined as the presence of hard or lumpy stools with ≥25% and loose or water stools with ≥25% of bowel movements. Final subtype, or unsubtyped, is all other cases of IBS that do not fall into the other classes. Pharmacological therapy for IBS depends on subtype.7 While several over-the-counter or off-label prescription agents are used for the treatment of IBS, there are currently only two agents approved by the Food and Drug Administration (FDA) for the treatment of IBS-C and three agents approved by the FDA for IBS-D. -
Prophylactic Antiemetic Therapy with Ondansetron, Granisetron and Metoclopramide in Patients Undergoing Laparoscopic Cholecystectomy Under GA
JK SCIENCE ORIGINAL ARTICLE Prophylactic Antiemetic Therapy with Ondansetron, Granisetron and Metoclopramide in Patients Undergoing Laparoscopic Cholecystectomy Under GA Vishal Gupta, Renu Wakhloo, Anjali Mehta, Satya Dev Gupta Abstract The aim of the present study was to compare the antiemetic effect of intravenous Granisetron, Ondansetron & Metoclopramide in a randomized blinded study for prophylaxis of post operative nausea and vomiting (PONV) in patients undergoing laparoscopic cholecystectomy under general anaesthesia. 60 patients (ASA I & II) undergoing laparoscopic cholecystectomy under general anaesthesia were randomly allocated into three equal groups (n=20). Emetic episodes in first 24 hours were recorded and compared in different study groups. Results were analyzed. Minimal emetic episodes were observed in early post-operative period (1-12hrs) in patients who had received intravenous granisetron in comparison to ondansetron and metoclopramide. However, after 12 hours emesis free periods were statistically insignificant between group A and B while patients in group C had no antiemetic effect. Keywords Post Operative Nausea and Vomiting (PONV), Granisetron, Ondensetron, Metoclopramide Introduction The most common and distressing symptoms, which vascular anastomoses and increased intracranial follow anaesthesia and surgery, are pain and emesis. The pressure(4). The anaesthetic consequences are aspiration syndrome of nausea, retching and vomiting is known as pneumonitis and discomfort in recovery. For institutions 'sickness' and each part of it can be distinguished as a there is increased financial burden because of increased separate entity (1). PONV (post operative nausea and nursing care, delayed discharge from Phase I and II vomiting) has been characterized as big 'little problem(2) recovery units and unexpected admissions. Hence, and has been a common complication for both in patients prophylactic antiemetic therapy is needed for all these and out patients undergoing virtually all types of surgical patients. -
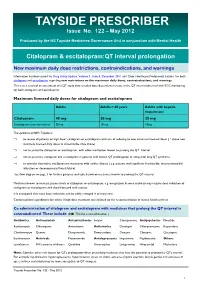
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Irritable Bowel Syndrome-Diarrhea
Clinical Pharmacy Program Guidelines for Irritable Bowel Syndrome-Diarrhea Program Prior Authorization Medication Lotronex (alosetron), Viberzi (eluxadoline) Markets in Scope Arizona, California, Colorado, Hawaii, Maryland, Nevada, New Jersey, New York, New York EPP, Pennsylvania- CHIP, Rhode Island, South Carolina Issue Date 3/2013 Pharmacy and 3/2021 Therapeutics Approval Date Effective Date 6/2021 1. Background: Lotronex (alosetron) is indicated only for use in women with severe diarrhea- predominant irritable bowel syndrome (IBS) who have: chronic IBS, had anatomical or biochemical abnormalities of the gastrointestinal tract excluded, and not responded adequately to conventional therapy. Viberzi (eluxadoline) is a mu-opioid receptor agonist, indicated for the treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults. 2. Coverage Criteria: A. Lotronex 1. Initial Authorization a. Lotronex will be approved based on all of the following criteria: (1) Diagnosis of severe diarrhea-predominant irritable bowel syndrome (IBS) -AND- (2) Symptoms for at least 6 months -AND- (3) Patient was female at birth -AND- Confidential and Proprietary, © 2021 UnitedHealthcare Services Inc. 1 (4) Age greater than or equal to 18 years -AND- (5) History of failure, contraindication, or intolerance to a tricyclic antidepressant (e.g. amitriptyline) Authorization will be issued for 12 months. 2. Reauthorization a. Lotronex will be approved based on the following criterion: (1) Documentation of positive clinical response to Lotronex therapy Authorization will be issued for 12 months. B. Viberzi 1. Initial Authorization a. Viberzi will be approved based on all of the following criteria: (1) Diagnosis of irritable bowel syndrome with diarrhea (IBS-D) -AND- (2) History of failure, contraindication, or intolerance to a tricyclic antidepressant (e.g. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -

Efficacy of Eluxadoline in Irritable Bowel Syndrome with Diarrhea
This is a repository copy of Efficacy of Eluxadoline in Irritable Bowel Syndrome With Diarrhea. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/156693/ Version: Accepted Version Article: Black, CJ, Houghton, LA and Ford, AC orcid.org/0000-0001-6371-4359 (2020) Efficacy of Eluxadoline in Irritable Bowel Syndrome With Diarrhea. American Journal of Gastroenterology, 115 (3). pp. 483-484. ISSN 0002-9270 10.14309/ajg.0000000000000518 © The American College of Gastroenterology 2020. All Rights Reserved. This is an author produced version of correspondence published in The American Journal of Gastroenterology. Uploaded in accordance with the publisher's self-archiving policy. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Black et al Page 1 of 11 TITLE PAGE Title: Relative Efficacy of Eluxadoline in Irritable Bowel Syndrome. Authors: Christopher J. Black1, 2, Lesley A. Houghton, 2, Alexander C. Ford1, 2. 1Leeds Gastroenterology Institute, St. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Acute Inhibitory Effects of Antidepressants on Lacrimal Gland Secretion in the Anesthetized Rat
Physiology and Pharmacology Acute Inhibitory Effects of Antidepressants on Lacrimal Gland Secretion in the Anesthetized Rat Martin Dankis, Ozgu Aydogdu, Gunnar Tobin, and Michael Winder Department of Pharmacology, Institute of Neuroscience and Physiology, the Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden Correspondence: Michael Winder, PURPOSE. Patients that medicate with antidepressants commonly report dryness of eyes. Department of Pharmacology, The cause is often attributed to the anticholinergic properties of the drugs. However, regu- Institute of Neuroscience and lation of tear production includes a substantial reflex-evoked component and is regulated Physiology, the Sahlgrenska via distinct centers in the brain. Further, the anticholinergic component varies greatly Academy, University of Gothenburg, among antidepressants with different mechanisms of action. In the current study it was Medicinaregatan 13 413 90, Gothenburg, Sweden; wondered if acute administration of antidepressants can disturb production of tears by [email protected]. affecting the afferent and/or central pathway. Received: November 9, 2020 METHODS. Tear production was examined in vivo in anesthetized rats in the presence Accepted: May 10, 2021 or absence of the tricyclic antidepressant (TCA) clomipramine or the selective sero- Published: June 7, 2021 tonin reuptake inhibitor (SSRI) escitalopram. The reflex-evoked production of tears was Citation: Dankis M, Aydogdu O, measured by challenging the surface of the eye with menthol (0.1 mM) and choliner- Tobin G, Winder M. Acute inhibitory gic regulation was examined by intravenous injection with the nonselective muscarinic effects of antidepressants on agonist methacholine (1–5 μg/kg). lacrimal gland secretion in the RESULTS. Acute administration of clomipramine significantly attenuated both reflex- anesthetized rat. -

Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee
Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee Summary of Safety Alert (December 2011) – http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769 Citalopram and escitalopram are associated with dose-dependent QT interval prolongation and should not be used in those with: congenital long QT syndrome; known pre-existing QT interval prolongation; or in combination with other medicines that prolong the QT interval. ECG measurements should be considered for patients with cardiac disease, and electrolyte disturbances should be corrected before starting treatment. For citalopram, new restrictions on the maximum daily doses now apply: 40 mg for adults; 20 mg for patients older than 65 years; and 20 mg for those with hepatic impairment. For escitalopram, the maximum daily dose for patients older than 65 years is now reduced to 10 mg/day; other doses remain unchanged. Recommended actions for prescribers If dose is above maximum recommended dose or patient is taking other medications likely to prolong QTc: Need for more than 1. Discuss with service user/patient. citalopram 40mg daily 2. Consider continued need for citalopram and/or alternative therapies (adults), 20mg daily (elderly and reduced hepatic function) e.g. for OCD, PTSD Adult citalopram Elderly (or other risk factors) Taking ANY other medicines Elderly and escitalopram dose above citalopram dose above likely to cause QTc dose above 10mg daily: prolongation 40mg daily: 20mg daily: Consider risk/benefit with service user. Switch if 1-Consider switching relevant possible medication to alternative with no Monitor If under 18 refer to CAMHS effect on QTc prolongation or Reduce dose stepwise to 40mg citalopram daily for adults (unlicensed use).