Serotonin 2A Activation and a Novel Therapeutic Drug
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Atypical Antipsychotics TCO 02.2018
Therapeutic Class Overview Atypical Antipsychotics INTRODUCTION • Antipsychotic medications have been used for over 50 years to treat schizophrenia and a variety of other psychiatric disorders (Miyamato et al 2005). • Antipsychotic medications generally exert their effect in part by blocking dopamine (D)-2 receptors (Jibson et al 2017). • Antipsychotics are divided into 2 distinct classes based on their affinity for D2 and other neuroreceptors: typical antipsychotics, also called first-generation antipsychotics (FGAs), and atypical antipsychotics, also called second- generation antipsychotics (SGAs) (Miyamato et al 2005). • Atypical antipsychotics do not have a uniform pharmacology or mechanism of action; these differences likely account for the different safety and tolerability profiles of these agents (Clinical Pharmacology 2020, Jibson et al 2017). The atypical antipsychotics differ from the early antipsychotics in that they have affinity for the serotonin 5-HT2 receptor in addition to D2. Clozapine is an antagonist at all dopamine receptors (D1-5), with lower affinity for D1 and D2 receptors and high affinity for D4 receptors. Aripiprazole and brexpiprazole act as partial agonists at the D2 receptor, functioning as an ○ agonist when synaptic dopamine levels are low and as an antagonist when they are high. Cariprazine is a partial agonist at D2 and D3. Pimavanserin does not have dopamine blocking activity and is primarily an inverse agonist at 5-HT2A receptors. The remaining atypical antipsychotics share the similarity of D2 and 5-HT2A -

Reviews Insights Into Pathophysiology from Medication-Induced Tremor
Freely available online Reviews Insights into Pathophysiology from Medication-induced Tremor 1* 1 1 1 John C. Morgan , Julie A. Kurek , Jennie L. Davis & Kapil D. Sethi 1 Movement Disorders Program Parkinson’s Foundation Center of Excellence, Department of Neurology, Medical College of Georgia, Augusta, GA, USA Abstract Background: Medication-induced tremor (MIT) is common in clinical practice and there are many medications/drugs that can cause or exacerbate tremors. MIT typically occurs by enhancement of physiological tremor (EPT), but not all drugs cause tremor in this way. In this manuscript, we review how some common examples of MIT have informed us about the pathophysiology of tremor. Methods: We performed a PubMed literature search for published articles dealing with MIT and attempted to identify articles that especially dealt with the medication’s mechanism of inducing tremor. Results: There is a paucity of literature that deals with the mechanisms of MIT, with most manuscripts only describing the frequency and clinical settings where MIT is observed. That being said, MIT emanates from multiple mechanisms depending on the drug and it often takes an individualized approach to manage MIT in a given patient. Discussion: MIT has provided some insight into the mechanisms of tremors we see in clinical practice. The exact mechanism of MIT is unknown for most medications that cause tremor, but it is assumed that in most cases physiological tremor is influenced by these medications. Some medications (epinephrine) that cause EPT likely lead to tremor by peripheral mechanisms in the muscle (b-adrenergic agonists), but others may influence the central component (amitriptyline). -

Low Continuation of Antipsychotic Therapy in Parkinson Disease – Intolerance, Ineffectiveness, Or Inertia? Thanh Phuong Pham Nguyen1,2,3,4*, Danielle S
Pham Nguyen et al. BMC Neurology (2021) 21:240 https://doi.org/10.1186/s12883-021-02265-x RESEARCH Open Access Low continuation of antipsychotic therapy in Parkinson disease – intolerance, ineffectiveness, or inertia? Thanh Phuong Pham Nguyen1,2,3,4*, Danielle S. Abraham1,2,3,4, Dylan Thibault1,2, Daniel Weintraub1,5 and Allison W. Willis1,2,3,4,6 Abstract Background: Antipsychotics are used in Parkinson disease (PD) to treat psychosis, mood, and behavioral disturbances. Commonly used antipsychotics differ substantially in their potential to worsen motor symptoms through dopaminergic receptor blockade. Recent real-world data on the use and continuation of antipsychotic therapy in PD are lacking. The objectives of this study are to (1) examine the continuation of overall and initial antipsychotic therapy in individuals with PD and (2) determine whether continuation varies by drug dopamine receptor blocking activity. Methods: We conducted a retrospective cohort study using U.S. commercially insured individuals in Optum 2001– 2019. Adults aged 40 years or older with PD initiating antipsychotic therapy, with continuous insurance coverage for at least 6 months following drug initiation, were included. Exposure to pimavanserin, quetiapine, clozapine, aripiprazole, risperidone, or olanzapine was identified based on pharmacy claims. Six-month continuation of overall and initial antipsychotic therapy was estimated by time to complete discontinuation or switching to a different antipsychotic. Cox proportional hazards models evaluated factors associated with discontinuation. Results: Overall, 38.6% of 3566 PD patients in our sample discontinued antipsychotic therapy after the first prescription, 61.4% continued with overall treatment within 6 months of initiation. Clozapine use was too rare to include in statistical analyses. -
Pimavanserin: a Potentially Safer Alternative to Clozapine for Refractory Hallucinations and Delusions
From the Editor Pimavanserin: A potentially safer alternative to clozapine for refractory hallucinations and delusions Up to 30% of patients with schizo- established a nonprofit foundation Henry A. Nasrallah, MD we called CURESZ (Comprehensive Editor-in-Chief phrenia do not respond to dopamine antagonists, which include all first- and Understanding via Research and Education in Schizophrenia), and assem- second-generation antipsychotics. bled a panel of 80 clozapine experts They are labeled as “treatment-resis- across the country to provide access to tant” if they have a partial response, clozapine for the hundreds of thousands Our clinical team or “treatment-refractory” if their hal- of individuals with refractory psychosis who never received a trial of clozapine made a serendipitous lucinations and/or delusions do not from their psychiatrists or psychiatric discovery about the improve at all despite multiple trials nurse practitioners. (Visit CURESZ.org efficacy of pimavanserin of antipsychotics. for details.) Bethany was very lucky to respond in patients with That’s why clozapine is considered and recover completely, because only schizophrenia who a “lifesaver” for such patients, a last- 40% of patients with refractory psycho- failed to respond to resort medication that unshackles sis respond to clozapine. She does not patients with refractory psychotic mind having her blood drawn every clozapine therapy symptoms from the tyranny of audi- week to measure her white blood cell tory and/or visual hallucinations and count for early detection of potentially the reality distortion of fixed false fatal agranulocytosis. Many refrac- beliefs such as paranoid delusions. tory, often homeless patients with Many long-suffering patients with chronic schizophrenia refuse to have refractory psychosis recover and return weekly phlebotomy and therefore are to their baseline, thanks to clozapine. -

Antipsychotics
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Pharmacy Policy Antipsychotics Policy Number: 9.503 Version Number: 2.1 Version Effective Date: 9/1/2021 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth - MCO MassHealth - ACO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options __________________________________ Note: Disclaimer and audit information is located at the end of this document. Prior Authorization Policy Products Affected: aripiprazole ODT Latuda (lurasidone) aripiprazole Sol Nuplazid (pimavanserin) asenapine maleate Rexulti (brexpiprazole) clozapine ODT Vraylar (cariprazine) risperidone ODT Versacloz (clozapine) Fanapt (iloperidone) Secuado (asenapine) Paliperidone The Plan may authorize coverage of the above products for members meeting the following criteria: Covered All FDA approved indications not otherwise excluded Use All indications supported by established clinical literature for the medical condition and age + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. Antipsychotics 1 of 6 Exclusion None Criteria Required Medical Information clozapine ODT, risperidone ODT, aripiprazole ODT, aripiprazole sol, Versacloz 1. A diagnosis of bipolar disorder, schizophrenia, or other psychotic disorder; OR 2. A diagnosis of major depression requiring adjunct therapy ( aripiprazole ODT, aripiprazole sol only); AND 3. Clinical swallowing difficulties (including unwillingness to swallow tablets) Fanapt, palipedione (oral), Latuda, Vraylar 1. A diagnosis of bipolar disorder, schizophrenia, or other psychotic disorder; AND 2. An inadequate response, intolerance or contraindication to a trial of two covered atypical antipsychotics (See Appendix A) Nuplazid 1. -

122 Use of Pimavanserin in Patients with Parkinson's Disease Psychosis
ABSTRACTS 77 than 10,000 downloads (2) a score of 3.5 or higher on the receptor (5-HT2A) inverse agonist/antagonist, is newly Mobile Apps Rating System (MARS) and (3) acquisition FDA-approved for the treatment of hallucinations and cost less than $1. Consumer reviews were scanned. A delusions associated with PDP. total of 7 apps were culled from an expanding universe of thousands. This included top-rated apps in each of three METHODS: In Study 020, a 6-week FDA registration study, symptom domains: depression, anxiety and cognitive 199 patients with baseline Mini-Mental State Examina- ≥ disorders. Ranked in order of MARS rating the leading tion (MMSE) score 21, moderate-severe psychosis, and depression apps were “Depression CBT Self-Help Guide” on stable PD meds, were randomized to PIM (34 mg/day) and “eCBT Mood”. The most popular anxiety apps were or placebo (PBO) for 6 weeks. This subgroup analysis “Stop Panic & Anxiety” and “Headspace”. The top apps evaluates efficacy and safety between two groups: those ≥ < for cognitive enhancement training were “Brain HQ” and with MMSE total score 21 but 25 (cognitively “Fit Brains Focus”. In addition, the suicide prevention impaired; equivalent to Montreal Cognitive Assessment ≥ app “My3” was included because of its life saving [MoCA] score 15-19) and those with score 25 (cogni- potential. Consumers have rated the reviewed apps tively normal; equivalent to MoCA score 20-30). Safety favorably. Conclusion: Smartphone apps are achieving assessments were performed on the full safety dataset wide acceptance in self-management of common psy- (i.e., three 6-week placebo-controlled studies) including = = chiatric disorders. -

Pimavanserin (NUPLAZID)
Pimavanserin (NUPLAZID) Criteria for Use December 2016; revised May 2018, August 2019 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The following recommendations are based on medical evidence, clinician input, and expert opinion. The content of the document is dynamic and will be revised as new information becomes available. The purpose of this document is to assist practitioners in clinical decision-making, to standardize and improve the quality of patient care, and to promote cost-effective drug prescribing. THE CLINICIAN SHOULD UTILIZE THIS GUIDANCE AND INTERPRET IT IN THE CLINICAL CONTEXT OF THE INDIVIDUAL PATIENT. INDIVIDUAL CASES THAT ARE EXCEPTIONS TO THE EXCLUSION AND INCLUSION CRITERIA SHOULD BE ADJUDICATED AT THE LOCAL FACILITY ACCORDING TO THE POLICY AND PROCEDURES OF ITS P&T COMMITTEE AND PHARMACY SERVICES. The Product Information should be consulted for detailed prescribing information. See the VA National PBM-MAP-VPE Monograph on this drug at www.pbm.va.gov or http://vaww.pbm.va.gov for further information. Exclusion Criteria If the answer to ANY item below is met, then the patient should NOT receive pimavanserin. The patient has a diagnosis of dementia-related psychosis due to Alzheimer’s disease, Lewy Body Dementia or other dementia not secondary to Parkinson disease. The patient has known QTc prolongation, history of cardiac arrhythmias, as well as other circumstances that may increase the risk of the occurrence of torsade de pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia, or the presence of congenital prolongation of the QT interval, or is taking other medications known to prolong the QT interval. -
BLACK-BOX WARNINGS: How They Can Improve Your Clinical Practice a Better Understanding of These Warnings Leads to Safer, More Effective Prescribing
BLACK-BOX WARNINGS: How they can improve your clinical practice A better understanding of these warnings leads to safer, more effective prescribing Matthew A. Schreiber, MD, PhD ecently, the FDA issued “black-box” warnings, its most promi- Staff Psychiatrist 1 Puget Sound VA Health Care System nent drug safety statements, for esketamine, which is indicated Seattle, Washington for treatment-resistant depression, and the Z-drugs, which are Assistant Professor R 2 indicated for insomnia (Table 1, page 20). A black-box warning also Department of Psychiatry and Behavioral Sciences University of Washington School of Medicine comes with brexanolone, which was recently approved for postpar- Seattle, Washington tum depression.3 While these newly issued warnings serve as a timely Michelle Wiese, MD, MPH reminder of the importance of black-box warnings, older black-box PGY-3 Psychiatry Resident warnings also cover large areas of psychiatric prescribing, including all University of Washington School of Medicine Seattle, Washington medications indicated for treating psychosis or schizophrenia (increased mortality in patients with dementia), and all psychotropic medications Disclosures The authors report no financial relationships with any with a depression indication (suicidality in younger people). company whose products are mentioned in this article, or with In this article, we help busy prescribers navigate the landscape manufacturers of competing products. The views expressed are of black-box warnings by providing a concise review of how to use those of the authors and do not reflect the official policy of the Department of Veterans Affairs or the US Government. them in clinical practice, and where to find information to keep up-to-date. -

Louisiana Fee-For-Service Medicaid Antipsychotics
Louisiana Fee-for-Service Medicaid Antipsychotics The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request: Authorization for non-preferred agents for recipients 6 years of age and older; AND Authorization for all preferred and non-preferred agents for recipients younger than 6 years of age; AND Authorization to exceed maximum daily dose/quantity limit for all ages. See full prescribing information for individual agents for details on the information below: *These agents have Black Box Warnings †These agents are subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations ‡ For long-acting injectable agents, it is required that the previous 60-day period of pharmacy claims show one of the following: Established tolerance to the oral formulation (as evidenced by a paid pharmacy claim for the oral formulation); OR Established therapy with the requested injectable agent (as evidenced by a paid pharmacy claim for the requested injectable agent) NOTE: Diagnosis code requirements apply to both preferred and non-preferred agents (see Table 1). Maximum daily dose edits (see Table 2), quantity limits (see Table 3), and other requirements at Point-of-Sale for select agents in this category may apply to both preferred and non-preferred agents. For additional information, see http://www.lamedicaid.com/provweb1/Pharmacy/pharmacyindex.htm. Oral Antipsychotics – Generic Name (Brand Example) * Amitriptyline/Perphenazine * Aripiprazole ODT; Oral Solution (Abilify®); Tablet (Abilify®) -

Medications to Be Avoided Or Used with Caution in Parkinson's Disease
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease This medication list is not intended to be complete and additional brand names may be found for each medication. Every patient is different and you may need to take one of these medications despite caution against it. Please discuss your particular situation with your physician and do not stop any medication that you are currently taking without first seeking advice from your physician. Most medications should be tapered off and not stopped suddenly. Although you may not be taking these medications at home, one of these medications may be introduced while hospitalized. If a hospitalization is planned, please have your neurologist contact your treating physician in the hospital to advise which medications should be avoided. Medications to be avoided or used with caution in combination with Selegiline HCL (Eldepryl®, Deprenyl®, Zelapar®), Rasagiline (Azilect®) and Safinamide (Xadago®) Medication Type Medication Name Brand Name Narcotics/Analgesics Meperidine Demerol® Tramadol Ultram® Methadone Dolophine® Propoxyphene Darvon® Antidepressants St. John’s Wort Several Brands Muscle Relaxants Cyclobenzaprine Flexeril® Cough Suppressants Dextromethorphan Robitussin® products, other brands — found as an ingredient in various cough and cold medications Decongestants/Stimulants Pseudoephedrine Sudafed® products, other Phenylephrine brands — found as an ingredient Ephedrine in various cold and allergy medications Other medications Linezolid (antibiotic) Zyvox® that inhibit Monoamine oxidase Phenelzine Nardil® Tranylcypromine Parnate® Isocarboxazid Marplan® Note: Additional medications are cautioned against in people taking Monoamine oxidase inhibitors (MAOI), including other opioids (beyond what is mentioned in the chart above), most classes of antidepressants and other stimulants (beyond what is mentioned in the chart above). -

Medications for Behavioral Changes in LBD
Caregiver Link: 800.539.9767 BEHAVIORAL CHANGES IN LEWY BODY DEMENTIA Care Brief #6 – Medications for Behavioral Changes in LBD People living with Lewy body dementia (LBD) may exhibit one or more of the following behavioral changes: psychosis (hallucinations; illusions; delusions, including paranoia, misidentification, Capgras syndrome, and reduplicative paramnesia; disinhibition; wandering; catastrophic reactions; and verbal and physical agitation) and mood or affective changes (depression, apathy, anxiety). (See Care Briefs #1 -2 for definitions, descriptions, examples, and causes.) Treatments should be tailored to each person’s unique needs. Non-medication treatments should be the first line of treatment (See Care Briefs #3-5). A physician with experience managing LBD-related behavioral changes may add drug treatment if needed. This Care Brief summarizes things to know about LBD treatments, in general; when to consider medication to treat behavioral and mood changes; medications that may reduce behavioral and mood changes; and medications that should be avoided or used with caution. Things to know about LBD treatments, in general - Before considering what medications might help manage behavioral and mood symptoms, care partners should know the following: • There are currently no medications that slow or stop the progression of LBD. However, there are drugs that may help with symptoms, including behavior and mood changes. • No medications are approved by the U.S. Food and Drug Administration (FDA) to treat any symptom of dementia with Lewy bodies (DLB); only one, rivastigmine/Exelon, is approved to treat cognition in Parkinson’s disease dementia (PDD). However, FDA-approved medications for other disorders such as Alzheimer’s disease and Parkinson’s disease are sometimes prescribed “off-label” in LBD. -
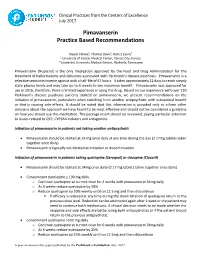
Pimavanserin Practice Based Recommendations
Clinical Practices from the Centers of Excellence July 2017 Pimavanserin Practice Based Recommendations Rajesh Pahwa1, Thomas Davis2, Kelly E Lyons1 1 University of Kansas Medical Center, Kansas City, Kansas 2 Vanderbilt University Medical Center, Nashville, Tennessee Pimavanserin (Nuplazid) is the only medication approved by the Food and Drug Administration for the treatment of hallucinations and delusions associated with Parkinson’s disease psychosis. Pimavanserin is a selective serotonin inverse agonist with a half-life of 57 hours. It takes approximately 12 days to reach steady state plasma levels and may take up to 6 weeks to see maximum benefit. Pimavanserin was approved for use in 2016, therefore, there is limited experience in using the drug. Based on our experience with over 130 Parkinson’s disease psychosis patients started on pimavanserin, we present recommendations on the initiation of pimavanserin, particularly when switching from another antipsychotic with suboptimal benefit or that is causing side effects. It should be noted that this information is provided only to inform other clinicians about the approach we have found to be most effective and should not be considered a guideline on how you should use this medication. The package insert should be reviewed, paying particular attention to issues related to QTC, CYP3A4 inducers and antagonists. Initiation of pimavanserin in patients not taking another antipsychotic • Pimavanserin should be started at 34 mg once daily at any time during the day (2 17mg tablets taken together