Antipsychotics Therapeutic Class Review (TCR)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HALDOL Brand of Haloperidol Injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia
HALDOL® brand of haloperidol injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol is the first of the butyrophenone series of major antipsychotics. The chemical designation is 4-[4-(p-chlorophenyl)-4-hydroxypiperidino] 4’-fluorobutyrophenone and it has the following structural formula: HALDOL (haloperidol) is available as a sterile parenteral form for intramuscular injection. The injection provides 5 mg haloperidol (as the lactate) and lactic acid for pH adjustment between 3.0 – 3.6. -

Original Research Published, Reproduced, Transmitted, Modified, Posted, Sold, Licensed, Or Used for Commercial Purposes
This work may not be copied, distributed, displayed, Original Research published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the Efficacy and Effectiveness of Depot publisher’s Terms & Conditions. Versus Oral Antipsychotics in Schizophrenia: Synthesizing Results Across Different Research Designs Noam Y. Kirson, PhD; Peter J. Weiden, MD; Sander Yermakov, MS; Wayne Huang, MPP; Thomas Samuelson, BA; Steve J. Offord, PhD; Paul E. Greenberg, MS, MA; and Bruce J. O. Wong, MD ABSTRACT he cornerstone of long-term maintenance therapy Objective: Nonadherence is a major challenge in schizophrenia Tof schizophrenia patients is relapse prevention. treatment. While long-acting (depot) antipsychotic medications are Relapse prevention is necessary—albeit not sufficient— often recommended to address adherence problems, evidence on for eventual successful rehabilitation.1 In practice, the the comparative effectiveness of depot versus oral antipsychotics is effectiveness of maintenance antipsychotic treatment is inconsistent. We hypothesize that this inconsistency could be due to often undermined by poor adherence to therapy. Not systematic differences in study design. This review evaluates the effect only is nonadherence the single greatest modifiable of study design on the comparative effectiveness of antipsychotic risk factor for relapse,2,3 it is also often undetected, formulations. The optimal use of different antipsychotic formulations resulting in lost opportunities to employ psychosocial in a general clinical setting depends on better understanding of the underlying reasons for differences in effectiveness across research interventions for adherence, as well as uncertainty as designs. to the relative contribution of lack of efficacy versus Data Sources: A PubMed literature review targeted English-language adherence problems to poor outcomes. -
When Clozapine Is Not Tolerated Mitchell J
University of North Dakota UND Scholarly Commons Nursing Capstones Department of Nursing 10-28-2018 When Clozapine is Not Tolerated Mitchell J. Relf Follow this and additional works at: https://commons.und.edu/nurs-capstones Recommended Citation Relf, Mitchell J., "When Clozapine is Not Tolerated" (2018). Nursing Capstones. 268. https://commons.und.edu/nurs-capstones/268 This Independent Study is brought to you for free and open access by the Department of Nursing at UND Scholarly Commons. It has been accepted for inclusion in Nursing Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. Running head: WHEN CLOZAPINE IS NOT TOLERATED 1 WHEN CLOZAPINE IS NOT TOLERATED by Mitchell J. Relf Masters of Science in Nursing, University of North Dakota, 2018 An Independent Study Submitted to the Graduate Faculty of the University of North Dakota in partial fulfillment of the requirements for the degree of Master of Science Grand Forks, North Dakota December 2018 WHEN CLOZAPINE IS NOT TOLERATED 2 PERMISSION Title When Clozapine is Not Tolerated Department Nursing Degree Master of Science In presenting this independent study in partial fulfillment of the requirements for a graduate degree from the University of North Dakota, I agree that the College of Nursing and Professional Disciplines of this University shall make it freely available for inspection. I further agree that permission for extensive copying or electronic access for scholarly purposes may be granted by the professor who supervised my independent study work or, in her absence, by the chairperson of the department or the dean of the School of Graduate Studies. -

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -

HIGHLIGHTS of PRESCRIBING INFORMATION These Highlights Do
HIGHLIGHTS OF PRESCRIBING INFORMATION • Metabolic Changes: Atypical antipsychotic drugs have been associated with These highlights do not include all the information needed to use metabolic changes that may increase cardiovascular/cerebrovascular risk. CLOZARIL safely and effectively. See full prescribing information for These metabolic changes include: CLOZARIL. o Hyperglycemia and Diabetes Mellitus: Monitor for symptoms of CLOZARIL® (clozapine) tablets, for oral use hyperglycemia including polydipsia, polyuria, polyphagia, and Initial U.S. Approval: 1989 weakness. Monitor glucose regularly in patients with diabetes or at risk for diabetes. (5.9) WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC o Dyslipidemia: Undesirable alterations in lipids have occurred in HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; patients treated with atypical antipsychotics. (5.9) MYOCARDITIS AND CARDIOMYOPATHY; INCREASED o Weight Gain: Significant weight gain has occurred. Monitor weight MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA- gain. (5.9) RELATED PSYCHOSIS • Neuroleptic Malignant Syndrome (NMS): Immediately discontinue and See full prescribing information for complete boxed warning. monitor closely. Assess for co-morbid conditions. (5.10) • Fever: Evaluate for infection and for neutropenia, NMS. (5.11) • Pulmonary Embolism (PE): Consider PE if respiratory distress, chest pain, • Severe Neutropenia: CLOZARIL can cause severe neutropenia, which or deep-vein thrombosis occur. (5.12) can lead to serious and fatal infections. Patients initiating and • Anticholinergic Toxicity: Use cautiously in presence of specific conditions continuing treatment with CLOZARIL must have a baseline blood (e.g., narrow angle glaucoma, use of anticholinergic drugs). (5.13) absolute neutrophil count (ANC) measured before treatment initiation • Interference with Cognitive and Motor Performance: Advise caution when and regular ANC monitoring during treatment (2.1, 5.1). -

ADHD Parents Medication Guide Revised July 2013
ADHD Parents Medication Guide Revised July 2013 Attention-Deficit/Hyperactivity Disorder Prepared by: American Academy of Child & Adolescent Psychiatry and American Psychiatric Association Supported by the Elaine Schlosser Lewis Fund Physician: ___________________________________________________ Address: ___________________________________________________ ___________________________________________________ ___________________________________________________ Phone: ___________________________________________________ Email: ___________________________________________________ ADHD Parents Medication Guide – July 2013 2 Introduction Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by difficulty paying attention, excessive activity, and impulsivity (acting before you think). ADHD is usually identified when children are in grade school but can be diagnosed at any time from preschool to adulthood. Recent studies indicate that almost 10 percent of children between the ages of 4 to 17 are reported by their parents as being diagnosed with ADHD. So in a classroom of 30 children, two to three children may have ADHD.1,2,3,4,5 Short attention spans and high levels of activity are a normal part of childhood. For children with ADHD, these behaviors are excessive, inappropriate for their age, and interfere with daily functioning at home, school, and with peers. Some children with ADHD only have problems with attention; other children only have issues with hyperactivity and impulsivity; most children with ADHD have problems with all three. As they grow into adolescence and young adulthood, children with ADHD may become less hyperactive yet continue to have significant problems with distraction, disorganization, and poor impulse control. ADHD can interfere with a child’s ability to perform in school, do homework, follow rules, and develop and maintain peer relationships. When children become adolescents, ADHD can increase their risk of dropping out of school or having disciplinary problems. -
Reveiw Week 3 Final with Questions
REVIEW 3 SOMATIZATION AND RELATED DISORDERS SOMATIZATION AND RELATED DISORDERS SOMATIZATION ▸ Psychological problems or concerns that are converted into and communicated as physical distress ▸ Anxiety is either Conscious or Unconscious ▸ Physical Illness is Real SOMATIZATION AND RELATED DISORDERS - SSD SOMATIC SYMPTOM DISORDER A. One or more somatic symptoms that are distressing or result in significant disruption of daily life B. Excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns as manifested by at least one of the following 1. Disproportionate and persistent thoughts about the seriousness or one’s symptoms 2. Persistently high level of anxiety about health or symptoms 3. Excessive time and energy devoted to these symptoms or health concerns C. Although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent (typically more than 6 months) SOMATIZATION AND RELATED DISORDERS - SSD TREATMENT ▸ Regular office visits with the same physician ▸ Psychotherapy ▸ Validate the patient’s feelings/experience of symptoms SOMATIZATION AND RELATED DISORDERS - ILLNESS ANXIETY DISORDER ILLNESS ANXIETY DISORDER A. Formerly hypochondriasis B. Preoccupation with having or acquiring a serious illness C. Somatic symptoms are not present or, if present, are only mild in intensity. If another medical condition is present or there is a high risk for developing a medical condition (strong FH), the preoccupation is clearly excessive or disproportionate D. There is a high level of anxiety about health, and the individual is easily alarmed about personal health status (preoccupation with idea one is sick) E. The individual performs excessive health-related behaviors (checking body) or exhibits maladaptive avoidance (avoids doctors) F. -

Lurasidone (Latuda) Reference Number: CP.PMN.50 Effective Date: 09.01.15 Last Review Date: 02.21 Line of Business: Commercial, HIM, Medicaid Revision Log
Clinical Policy: Lurasidone (Latuda) Reference Number: CP.PMN.50 Effective Date: 09.01.15 Last Review Date: 02.21 Line of Business: Commercial, HIM, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Lurasidone (Latuda®) is an atypical antipsychotic. FDA Approved Indication(s) Latuda is indicated for the treatment of: • Schizophrenia in adults and adolescents (13 to 17 years) • Depressive episode associated with bipolar I disorder (bipolar depression) in adults and pediatric patients (10 to 17 years) as monotherapy • Depressive episode associated with bipolar I disorder (bipolar depression) in adults as adjunctive therapy with lithium or valproate Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Latuda is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Bipolar Disorder (must meet all): 1. Diagnosis of bipolar disorder; 2. Age ≥ 10 years; 3. Failure of two preferred atypical antipsychotics (e.g., aripiprazole, ziprasidone, quetiapine, risperidone, or olanzapine) at up to maximally indicated doses, each used for ≥ 4 weeks, unless all are contraindicated or clinically significant adverse effects are experienced; 4. Dose does not exceed 120 mg per day for adults and 80 mg per day for pediatric patients. Approval duration: Medicaid/HIM – 12 months Commercial – Length of Benefit B. Schizophrenia (must meet all): 1. Diagnosis of schizophrenia; 2. Age ≥ 13 years; 3. Failure of two preferred atypical antipsychotics (e.g., aripiprazole, ziprasidone, quetiapine, risperidone, or olanzapine) at up to maximally indicated doses, each used Page 1 of 6 CLINICAL POLICY Lurasidone for ≥ 4 weeks, unless all are contraindicated or clinically significant adverse effects are experienced; 4. -
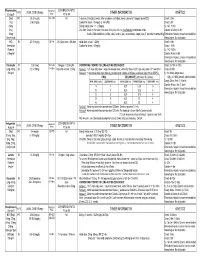
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Adverse Reactions to Hallucinogenic Drugs. 1Rnstttutton National Test
DOCUMENT RESUME ED 034 696 SE 007 743 AUTROP Meyer, Roger E. , Fd. TITLE Adverse Reactions to Hallucinogenic Drugs. 1rNSTTTUTTON National Test. of Mental Health (DHEW), Bethesda, Md. PUB DATP Sep 67 NOTE 118p.; Conference held at the National Institute of Mental Health, Chevy Chase, Maryland, September 29, 1967 AVATLABLE FROM Superintendent of Documents, Government Printing Office, Washington, D. C. 20402 ($1.25). FDPS PRICE FDPS Price MFc0.50 HC Not Available from EDRS. DESCPTPTOPS Conference Reports, *Drug Abuse, Health Education, *Lysergic Acid Diethylamide, *Medical Research, *Mental Health IDENTIFIEPS Hallucinogenic Drugs ABSTPACT This reports a conference of psychologists, psychiatrists, geneticists and others concerned with the biological and psychological effects of lysergic acid diethylamide and other hallucinogenic drugs. Clinical data are presented on adverse drug reactions. The difficulty of determining the causes of adverse reactions is discussed, as are different methods of therapy. Data are also presented on the psychological and physiolcgical effects of L.S.D. given as a treatment under controlled medical conditions. Possible genetic effects of L.S.D. and other drugs are discussed on the basis of data from laboratory animals and humans. Also discussed are needs for futher research. The necessity to aviod scare techniques in disseminating information about drugs is emphasized. An aprentlix includes seven background papers reprinted from professional journals, and a bibliography of current articles on the possible genetic effects of drugs. (EB) National Clearinghouse for Mental Health Information VA-w. Alb alb !bAm I.S. MOMS Of NAM MON tMAN IONE Of NMI 105 NUNN NU IN WINES UAWAS RCM NIN 01 NUN N ONMININI 01011110 0. -
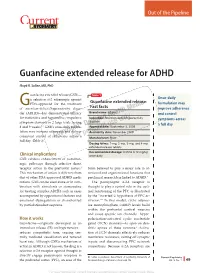
Guanfacine Extended Release for ADHD
Out of the Pipeline p Guanfacine extended release for ADHD Floyd R. Sallee, MD, PhD uanfacine extended release (GXR)— Table 1 α Once-daily a selective -2 adrenergic agonist Guanfacine extended release: GFDA-approved for the treatment formulation may of attention-defi cit/hyperactivity disor- Fast facts improve adherence der (ADHD)—has demonstrated effi cacy Brand name: Intuniv and control for inattentive and hyperactive/impulsive Indication: Attention-defi cit/hyperactivity symptoms across disorder symptom domains in 2 large trials lasting® Dowden Health Media a full day 8 and 9 weeks.1,2 GXR’s once-daily formu- Approval date: September 3, 2009 lation may increase adherence and deliver Availability date: November 2009 consistent control of symptomsCopyright across a For personalManufacturer: use Shire only full day (Table 1). Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets Recommended dosage: 0.05 to 0.12 mg/kg Clinical implications once daily GXR exhibits enhancement of noradren- ergic pathways through selective direct receptor action in the prefrontal cortex.3 brain believed to play a major role in at- This mechanism of action is different from tentional and organizational functions that that of other FDA-approved ADHD medi- preclinical research has linked to ADHD.3 cations. GXR can be used alone or in com- The postsynaptic α-2A receptor is bination with stimulants or atomoxetine thought to play a central role in the opti- for treating complex ADHD, such as cases mal functioning of the PFC as illustrated accompanied by oppositional features and by the “inverted U hypothesis of PFC ac- emotional dysregulation or characterized tivation.”4 In this model, cyclic adenos- by partial stimulant response.