Schizophrenia Care Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HALDOL Brand of Haloperidol Injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia
HALDOL® brand of haloperidol injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol is the first of the butyrophenone series of major antipsychotics. The chemical designation is 4-[4-(p-chlorophenyl)-4-hydroxypiperidino] 4’-fluorobutyrophenone and it has the following structural formula: HALDOL (haloperidol) is available as a sterile parenteral form for intramuscular injection. The injection provides 5 mg haloperidol (as the lactate) and lactic acid for pH adjustment between 3.0 – 3.6. -

Pindolol of the Activation of Postsynaptic 5-HT1A Receptors
Potentiation by (-)Pindolol of the Activation of Postsynaptic 5-HT1A Receptors Induced by Venlafaxine Jean-Claude Béïque, Ph.D., Pierre Blier, M.D., Ph.D., Claude de Montigny, M.D., Ph.D., and Guy Debonnel, M.D. The increase of extracellular 5-HT in brain terminal regions antagonist WAY 100635 (100 g/kg, i.v.). A short-term produced by the acute administration of 5-HT reuptake treatment with VLX (20 mg/kg/day ϫ 2 days) resulted in a inhibitors (SSRI’s) is hampered by the activation of ca. 90% suppression of the firing activity of 5-HT neurons somatodendritic 5-HT1A autoreceptors in the raphe nuclei. in the dorsal raphe nucleus. This was prevented by the The present in vivo electrophysiological studies were coadministration of (-)pindolol (15 mg/kg/day ϫ 2 days). undertaken, in the rat, to assess the effects of the Taken together, these results indicate that (-)pindolol coadministration of venlafaxine, a dual 5-HT/NE reuptake potentiated the activation of postsynaptic 5-HT1A receptors inhibitor, and (-)pindolol on pre- and postsynaptic 5-HT1A resulting from 5-HT reuptake inhibition probably by receptor function. The acute administration of venlafaxine blocking the somatodendritic 5-HT1A autoreceptor, but not and of the SSRI paroxetine (5 mg/kg, i.v.) induced a its postsynaptic congener. These results support and extend suppression of the firing activity of dorsal hippocampus CA3 previous findings providing a biological substratum for the pyramidal neurons. This effect of venlafaxine was markedly efficacy of pindolol as an accelerating strategy in major potentiated by a pretreatment with (-)pindolol (15 mg/kg, depression. -

Australian Product Information Parlodel® (Bromocriptine Mesilate)
AUSTRALIAN PRODUCT INFORMATION PARLODEL® (BROMOCRIPTINE MESILATE) TABLET AND HARD CAPSULE 1 NAME OF THE MEDICINE Bromocriptine mesilate 2 QUALITATIVE AND QUANTITATIVE COMPOSITION • Parlodel tablets and capsules contain bromocriptine mesilate • Oral tablets: ➢ 2.5 mg bromocriptine (present as 2.9 mg mesilate). • Oral capsules: ➢ 10 mg bromocriptine (present as 11.5 mg mesilate). ➢ 5 mg bromocriptine (present at 5.735 mg mesilate). • List of excipients with known effect: lactose and sugars. • For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Oral tablets: • White, coded XC with breakline on one side, SANDOZ on the other side. Oral capsules: • 5 mg: opaque white and opaque blue, marked PS • 10 mg: opaque white 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS • Prevention of onset of lactation in the puerperium for clearly defined medical reasons. Therapy should be continued for 14 days to prevent rebound lactation. Parlodel should not be used to suppress established lactation. • Treatment of hyperprolactinaemia where surgery and/or radiotherapy are not indicated or have already been used with incomplete resolution. Precautions should be taken to ensure that the hyperprolactinaemia is not due to severe primary hypothyroidism. Where the cause of hyperprolactinaemia is a prolactin-secreting microadenoma or macroadenoma, Parlodel is indicated for conservative treatment; prior to surgery in order to reduce tumour size and to facilitate removal; after surgery if prolactin level is still elevated. • Adjunctive therapy in the management of acromegaly when: (1) The patient refuses surgery and/or radiotherapy (2) Surgery and/or radiotherapy has been unsuccessful or full effects are not expected for some months (3) A manifestation of the acromegaly needs to be brought under control pending surgery and/or radiotherapy. -

Anaesthesia and Past Use Of
177 Correspondence were using LSD. It is more popular than other commonly Anaesthesia and past use of used hallucinogens whose quoted incidence of clients are: LSD ketamine 0.1% (super-K/vitamin K.I), psilocybin and psilocin 0.6% (the active alkaloids in the Mexican "magic To the Editor: mushroom"), and 3,4 methylenedioxymethamphetamine We report the case of a 43-yr-old lady who was admitted ~MDMA" 1% (ecstasy). The effects of the concurrent to the Day Surgery Unit for release of her carpal tunnel ingestion of LSD on anaesthesia are well described. 2-4 retinaculum. During the preoperative visit, she reported The long-term effects of the past use of LSD are largely no intercurrent illnesses, drug therapy or allergies. She unknown. We wonder if the hallucinations experienced did say, however, that she was frightened of general anaes- by our patient during anaesthesia were due to her LSD thesia, since she had experienced terrifying dreams during intake many years before. We would be interested to surgery under general anaesthesia on three occasions dur- know if others have had experience anaesthetising patients ing the previous ten years. On further questioning, she who are past users of phencyclidine-derived drugs. admitted that she had used lysergic acid diethylamide (LSD) during the late 1960's, the last occasion being 1968 Geoffrey N. Morris MRCGPFRCA when she had experienced characterstic hallucinations. Patrick T. Magee MSe FRCA She had not experienced hallucinations in the ensuing Anaesthetic Department years, except on the surgical occasions mentioned. Royal United Hospital One of the three previous operations had been per- Combe Park formed at our hospital and the anaesthetic record was Bath BA1 3NG checked. -

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -

AMANTADIP\Dle: on Nemolebtic-II[WDUCED CATALEPSY UV the RAT
J. Fac. Plmnz. Istanbul lstanbul Ecz. Fak. Mec. 29, 1 (1993) 29, 1 (1993) THE EFFECT OF CYPROHEPT~~AWEb AMANTADIP\dlE: ON NEmOLEBTIC-II[WDUCED CATALEPSY UV THE RAT SUMMARY Catalepsy is not a unitary phenomenon. With respect to biochemical mechanisms and neurotransmitter sytems, the origin of this behavioural response varies according to different substances which cause catalepsy. For example, the catdeptogenic effect of ne- uroleptics has been related to the blockage of striatal doparnine receptors. Neurophysio- logical and biochemical data have shown that a mechanism caused by gama-aminobuty- ric acid and serotonin have been effective in the proper functioning of the dopaminergic nigrosbriatal tract. We have studied the effects of cyproheptadine, a serotonin antagonist, and of amantadin which is used in the treatment of Parkinson syndrome on the catalepsy indu- ced by trifluoperazine, a phenothiazin compound, and pimozid, a drug used as a neuro- leptic. It was observed that when rats were pretreated with cyproheptadine as well as amantadiie, the catalepsy induced by the above neuroleptic drugs was attenuated. The results of our study show that substances which have an effect on the seroto- nergic and dopaminergic systems also play a role on cases of catalepsy induced by the neuroleptic drugs mentioned above. (*) Faculty of Pharmacy, Depament of Pharmacology, University of Istanbul, 31152, Istanbul, Turkey Katalepsi bir tek nedene bagh OWortaya qllian bit durum degildir. Biyokimya- sal ve norotransmitter sistemler agsmdan bu davran~glnsebebi, katalepsi olughYan qe- gitli maddeler iqin fad&&. Omegin noroleptiklerin kataleptojenik etkisi striatal dopa- min reseptorlerinin blokaj~nabajjlanmqtx. Niirofizyolojik ve biyokimyasal veriler do- pamine jik nigro-striatal sistemin duzenli $&$masmda gma-aminobutirik asid ve sero- tonin'e bagh olan bir mekanizmmn etkili oldugunu gostermigtir. -

Papers and Originals
BRITISH MEDICAL JOURNAL 19 FEBRUARY 1972 463 PAPERS AND ORIGINALS Drug Interaction: Inhibitory Effect of Neuroleptics on Metabolism of Tricyclic Antidepressants in Man LARS F. GRAM, KERSTIN FREDRICSON OVERO British Medical Journal, 1972, 1, 463-465 excretion (Anders, 1971). There are relatively few reports on interaction concerning neuroleptics or tricyclic antidepressants. Summary Chlorpromazine has both stimulatory and inhibitory effects on the metabolism of hexobarbitone in Total urinary excretion of radioactivity after oral or experimental animals of a test of (Riimke and Bout, 1960-1). Furthermore, chlorpromazine intravenous administration dose '4C-imi- accelerates the metabolism pramine was measured in were tested ofmeprobamate (Kato and Vassanelli, eight patients. They 1962). Tricyclic antidepressants have been shown to inhibit the before, during, and after treatment with neuroleptics. metabolism Excretion diminished while the were of tremorine and oxotremorine in rats in vitro and patients being in vivo (Hammer and Sjoqvist, 1967). It has also been found treated with perphenazine, haloperidol, or chlorproma- that zine, not treatment. desipramine hydrochloride inhibits the metabolism of though during flupenthixol amphetamine in isolated, perfused rat liver (Dingell and Bass, Total urinary excretion of radioactivity and plasma 1969). Pretreatment levels of metabolites and were measured with phenobarbitone decreased steady-state unchanged drug plasma levels of desipramine and nortriptyline in man (Sjoqvist in five patients after a test dose of 14C-nortriptyline. Each et was before and al. 1968). These findings were later confirmed in a twin study patient tested again during perphenazine (Alexanderson et al., 1969). Forrest et treatment. In all patients perphenazine treatment caused: al. (1970) found increased (1) decrease of total urinary excretion, (2) decreased urinary excretion of chlorpromazine metabolites when patients plasma level of metabolites, and (3) increased plasma were given additional treatment with phenobarbitone. -

Delusional Parasitosis Mimicking Cutaneous Infestation in Elderly Patients
LESSONS FROM PRACTICE LESSONS FROM PRACTICE Delusional parasitosis mimicking cutaneous infestation in elderly patients Clinical records Patient 1 Patient 3 An 88-year-old man gave a 12-month history of seeing insects attacking An 81-year-old woman was referred with a persistent belief that his legs and crawling along the floor of his house. He described these she had scabies and lice infestation of her eyes, nose, arms and insects as 4 cm long, black and white bugs with beaks, which pecked anus. This resulted in her persistently washing her clothes and at hisThe legs, Medical causing Journal wounds. of He Australia often felt ISSN:a sharp 0025-729X stinging sensation 18 herself and reporting the retirement village where she lived to the heraldingAugust their 2003 presence. 179 4 209-210 He also had burning pain in both legs below Health Department. She had received anti-scabies treatment the knees. He had had his house fumigated twice in the previous year empirically. ©The Medical Journal of Australia 2003 www.mja.com.au andLessons put various from chemicals practice across his doorways and bed to ward off the She had a long history of severe depression after the death of her bugs. He described no other hallucinations or delusions. husband, for which she took doxepin. She had paranoid ideation He was not using any regular medications and had never been a about her neighbours and saw things crawling down the walls, consumer of alcohol. He lived alone and managed all activities of and had moved residences several times to avoid these problems. -
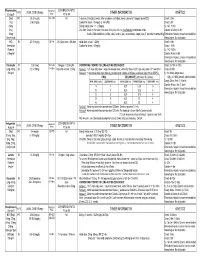
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Does Curcumin Or Pindolol Potentiate Fluoxetine's Antidepressant Effect
Research Paper Does Curcumin or Pindolol Potentiate Fluoxetine’s Antidepressant Effect by a Pharmacokinetic or Pharmacodynamic Interaction? H. A. S. MURAD*, M. I. SULIAMAN1, H. ABDALLAH2 AND MAY ABDULSATTAR1 Department of Pharmacology, Faculty of Medicine, Rabigh, King Abdulaziz University (KAU), Jeddah-21589, Saudi Arabia (SA) and Faculty of Medicine, Ain Shams University, Cairo-11541, Egypt. 1Department of Pharmacology, Faculty of Medicine, KAU, Jeddah-21589, SA. 2Department of Natural Products, Faculty of Pharmacy, KAU, Jeddah-21589, SA and Department of Pharmacognosy, Faculty of Pharmacy, Cairo University, Cairo-11541, Egypt Murad, et al.: Potentiation of Fluoxetine by Curcumin This study was designed to study potentiation of fluoxetine’s antidepressant effect by curcumin or pindolol. Twenty eight groups of mice (n=8) were used in three sets of experiments. In the first set, 9 groups were subjected to the forced swimming test after being treated intraperitoneally with three vehicles, fluoxetine (5 and 20 mg/kg), curcumin (20 mg/kg), pindolol (32 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg). One hour after the test, serum and brain fluoxetine and norfluoxetine levels were measured in mice receiving fluoxetine (5 and 20 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg). In the second set, the test was done after pretreatment with p-chlorophenylalanine. In the third set, the locomotor activity was measured. The immobility duration was significantly decreased in fluoxetine (20 mg/kg), curcumin (20 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg) groups. These decreases were reversed with p-chlorophenylalanine. -
Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

Opipramol and Trifluoperazine in the Treatment of Anxiety and Tension
A COMPARATIVE STUDY OF TWO ANTIHISTAMINES 395 In table VI are given the results of a question directed at discovering how effective the preferred treatment was compared to any other antihistamine used. Fifteen patients only were able to give this information but the results are interesting. Discussion TABLE VI The design of this study was very simple as COMPARISON WITH PREVIOUSLY USED ANTIHISTAMINE such studies must be if they are to be completed under the conditions of a busy general practice. In a condition such as hay fever where anti- Worse As good Better Total histamines are known to be etfective and where fairly rapid symptomatic relief is needed by the 2 4 9 15* patient, we did not feel justified in including a placebo. The results of the study seem fairly *In the majority of patients the previously used clear-cut that if patients are offered the choice antihistamine was the chemically related chlor- of a plain form of this antihistamine or a long- pheniramine maleate B.P. acting form more will choose the latter. Ofthose that do so, however, only about a third find a single tablet at night completely effective, the remainder have to take one further tablet during the day. Both forms of antihistamine are effective and where a retrospective comparison can be made this effectiveness is considered greater or equal to that of previously administered anti-histamines. Summary A simple comparative study under general-practice conditions of two formulations of pheniramine is described. Sixty-one per cent of patients preferred the long-acting form of this antihistamine.