Valbenazine for Tardive Dyskinesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
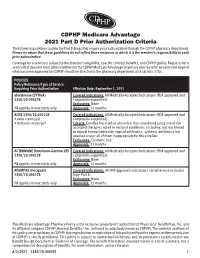
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

New Zealand Data Sheet 1
New Zealand Data Sheet 1. PRODUCT NAME Motetis 25 mg tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each Motetis 25 mg tablets contains 25 mg of tetrabenazine. Excipient(s) with known effect Contains lactose monohydrate. For the full list of excipients, see Section 6.1. 3. PHARMACEUTICAL FORM Yellow, round, flat tablet with a score line on one side. The tablet can be divided into equal halves. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Movement disorders associated with organic central nervous system conditions, such as Huntington's chorea, hemiballismus and senile chorea. Tetrabenazine is also indicated for the treatment of moderate to severe tardive dyskinesia, which is disabling and/or socially embarrassing. The condition should be persistent despite withdrawal of antipsychotic therapy, or in cases where withdrawal of antipsychotic medication is not a realistic option; also, where the condition persists despite reduction in dosage of antipsychotic medication or switching to atypical antipsychotic medication. 4.2. Dose and method of administration Dose Proper dosing of tetrabenazine involves careful titration of therapy to determine an individualised dose for each patient. When first prescribed, tetrabenazine therapy should be titrated slowly over several weeks to allow the identification of a dose for chronic use that reduces chorea and is well tolerated. Movement disorders Dosage and administration are variable and only a guide is given. An initial starting dose of 25 mg three times a day is recommended. This can be increased by 25 mg a day every three (3) or four (4) days until 200 mg per day is being given or the limit of tolerance, as dictated by unwanted effects, is reached, whichever is the lower dose. -

209241Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209241Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 209241 PDUFA Goal Date April 11, 2017 OSE RCM # 2016-2014 Reviewer Name(s) Mona Patel, Pharm.D. Team Leader Leah Hart, Pharm.D. Deputy Division Director Jamie Wilkins Parker, Pharm.D. Review Completion Date March 22, 2017 Subject Evaluation of Need for a REMS Established Name Valbenazine Trade Name Ingrezza Name of Applicant Neurocrine Biosciences, Inc. Therapeutic Class Vesicular Monoamine Transporter 2 (VMAT 2) Formulation(s) capsule Dosing Regimen 80 mg once daily 1 Reference ID: 4072847 Table of Contents EXECUTIVE SUMMARY............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background.........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Tetrabenazine: the First Approved Drug for the Treatment of Chorea in US Patients with Huntington Disease
Neuropsychiatric Disease and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW 7HWUDEHQD]LQHWKHÀUVWDSSURYHGGUXJ for the treatment of chorea in US patients with Huntington disease Samuel Frank Abstract: Huntington disease (HD) is a dominantly inherited progressive neurological disease Boston University School of Medicine, characterized by chorea, an involuntary brief movement that tends to flow between body regions. Boston, Massachusetts, USA HD is typically diagnosed based on clinical findings in the setting of a family history and may be confirmed with genetic testing. Predictive testing is available to those at risk, but only experienced clinicians should perform the counseling and testing. Multiple areas of the brain degenerate mainly involving the neurotransmitters dopamine, glutamate, and G-aminobutyric acid. Although pharmacotherapies theoretically target these neurotransmitters, few well-conducted trials for symptomatic or neuroprotective interventions yielded positive results. Tetrabenazine (TBZ) is a dopamine-depleting agent that may be one of the more effective agents for reducing chorea, although it has a risk of potentially serious adverse effects. Some newer antipsychotic agents, such as olanzapine and aripiprazole, may have adequate efficacy with a more favorable adverse-effect profile than older antipsychotic agents for treating chorea and psychosis. This review will address the epidemiology and diagnosis of HD as background for understanding potential pharmacological treatment options. Because TBZ is the only US Food and Drug Administration-approved medication in the United States for HD, the focus of this review will be on its pharmacology, efficacy, safety, and practical uses. There are no current treatments to change the course of HD, but education and symptomatic therapies can be effective tools for clinicians to use with patients and families affected by HD. -

Clinical Study Protocol with Amendment 3 an Open-Label
Clinical Study Protocol with Amendment 3 An Open-Label, Long Term Safety Study of SD-809 ER in Subjects with Chorea Associated with Huntington Disease Study SD-809-C-16 NCT01897896 Protocol with Amendment 3 Approval Date: 2 March 2015 &21),'(17,$/ 7KHIROORZLQJFRQWDLQVFRQILGHQWLDOSURSULHWDU\LQIRUPDWLRQZKLFKLVWKHSURSHUW\RI $XVSH[3KDUPDFHXWLFDOV,QF 35272&2/180%(56'& $123(1/$%(//21*7(506$)(7<678'<2)6'(5,1 68%-(&76:,7+&+25($$662&,$7(':,7+ +817,1*721',6($6( $OWHUQDWLYHVIRU5HGXFLQJ&KRUHDLQ+XQWLQJWRQ'LVHDVH $5&+' 0DUFK $PHQGPHQW 'HYHORSPHQW3KDVH Auspex Pharmaceuticals, Inc. Protocol SD-809-C-16 Huntington Study Group ARC-HD STUDY CONTACTS SPONSOR: Auspex Pharmaceuticals, Inc. 3333 N. Torrey Pines Court, Suite 400 La Jolla, CA 92037 USA Principal Investigator Co-Principal Investigator CLINICAL MONITOR Amendment 3 CONFIDENTIAL 2 Auspex Pharmaceuticals, Inc. Protocol SD-809-C-16 Huntington Study Group ARC-HD PROTOCOL SYNOPSIS PROTOCOL SD-809-C-16 TITLE An Open-Label, Long Term Safety Study of SD-809 ER in Subjects With Chorea Associated With Huntington Disease Running Title Alternatives for Reducing Chorea in HD (ARC-HD) PHASE 3 (Safety) INDICATION Treatment of chorea associated with Huntington disease NO. SITES Approximately 40 OBJECTIVES 1) Evaluate the safety and tolerability of titration and maintenance therapy with SD-809 ER 2) Evaluate the safety and tolerability of switching subjects from tetrabenazine to SD-809 ER 3) Evaluate the pharmacokinetics of tetrabenazine, SD-809 and their respective α- and β-HTBZ metabolites in subjects switching from tetrabenazine to SD-809 ER STUDY Approximately 116 male and female adult subjects with manifest Huntington disease POPULATION (HD) who are receiving approved doses of tetrabenazine for treatment of chorea (approx. -

Amnurite® Tablets
Amnurite® Tablets Each Tablet Contains Amitriptyline – 10 / 25 mg Mecobalamin – 1500 mcg SR PHARMACEUTICAL INFORMATION – AMITRIPTYLINE Generic name: Amitriptyline Chemical name: 3-(10,11-dihydro-5H-dibenzo[a,d]cycloheptene-5-ylidene)-N,N-dimethyl propan - 1 - amine Molecular mass: 277.403 g/mol Structural formula: Empirical formula – C20 H23 N Storage and Stability: Store at room temperature (15°to 30°C) MECOBALAMIN Generic name: Methylcobalamin Molecular mass: 1344.40 g/mol Structural formula: Empirical formula – C63H91CoN13O14P PHARMACOKINETIC PROPERTIES – Amitriptyline Amitriptyline is well absorbed from the gastrointestinal tract with peak plasma concentrations occurring between 2 and 12 hours after administration. Bioavailability of the drug is between 30 and 60% due to extensive first pass metabolism of the drug in the liver. Amitriptyline is demethylated in the liver to its primary active metabolite, nortriptyline. Amitriptyline is over 90% protein bound. Its elimination half-life varies from 10 to 50 hours, with an average of 15 hours. Within 24 hours, approximately 25 to 50% of a dose of amitriptyline is excreted in the urine as inactive metabolites; small amounts are excreted in the bile. Routine serum drug concentration monitoring is not warranted but may be useful to assess compliance or suspected toxicity. Recommended therapeutic trough levels, i.e., the sum of both amitriptyline and its metabolite nortriptyline, vary widely and range from 250 to 900 nmol/L (60 to 250 ng/mL). Ideally, the trough level should be taken 12 hours following administration of the last dose. TCAs are thought to work by inhibiting reuptake of norepinephrine and serotonin in the CNS, which potentiates the neurotransmitters. -

Central Nervous System (CNS) Agents
Clinical Policy: Central Nervous System (CNS) Agents: Movement Disorders Reference Number: OH.PHAR.PPA.96 Effective Date: 01.01.2021 Last Review Date: 11.20 Line of Business: Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. MOVEMENT DISORDERS CLINICAL PA REQUIRED “PREFERRED” PA REQUIRED “NON-PREFERRED” AUSTEDO ® (deutetrabenazine)† INGREZZA® (valbenazine) TETRABENAZINE (generic of Xenazine®) † Quantity limit of 4 tablets per day Description Deutetrabenazine (Austedo®), tetrabenazine (Xenazine®) and valbenazine (Ingrezza®) are vesicular monoamine transporter 2 (VMAT2) inhibitors. FDA Approved Indication(s) Austedo is indicated for the treatment of: • Chorea associated with Huntington’s disease • Tardive dyskinesia (TD) in adults Ingrezza is indicated for the treatment of adults with tardive dyskinesia. Xenazine is indicated for the treatment of chorea associated with Huntington’s disease. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Austedo, Xenazine or Ingrezza are medically necessary when the following criteria are met: I. Initial Approval Criteria A. Chorea Associated with Huntington Disease (must meet all): Page 1 of 7 CLINICAL POLICY Central Nervous System (CNS) Agents: Movement Disorders 1. Diagnosis of chorea associated with Huntington disease; 2. Requested medication is either Austedo or Xenazine; 3. Member must meet labeled age requirements for requested medication; 4. If requested medication is Austedo member has had a trial and failure of tetrabenazine at maximally tolerated doses up to 100 mg per day, unless contraindicated or clinically significant adverse effects are experienced; 5. -

Medications to Be Avoided Or Used with Caution in Parkinson's Disease
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease This medication list is not intended to be complete and additional brand names may be found for each medication. Every patient is different and you may need to take one of these medications despite caution against it. Please discuss your particular situation with your physician and do not stop any medication that you are currently taking without first seeking advice from your physician. Most medications should be tapered off and not stopped suddenly. Although you may not be taking these medications at home, one of these medications may be introduced while hospitalized. If a hospitalization is planned, please have your neurologist contact your treating physician in the hospital to advise which medications should be avoided. Medications to be avoided or used with caution in combination with Selegiline HCL (Eldepryl®, Deprenyl®, Zelapar®), Rasagiline (Azilect®) and Safinamide (Xadago®) Medication Type Medication Name Brand Name Narcotics/Analgesics Meperidine Demerol® Tramadol Ultram® Methadone Dolophine® Propoxyphene Darvon® Antidepressants St. John’s Wort Several Brands Muscle Relaxants Cyclobenzaprine Flexeril® Cough Suppressants Dextromethorphan Robitussin® products, other brands — found as an ingredient in various cough and cold medications Decongestants/Stimulants Pseudoephedrine Sudafed® products, other Phenylephrine brands — found as an ingredient Ephedrine in various cold and allergy medications Other medications Linezolid (antibiotic) Zyvox® that inhibit Monoamine oxidase Phenelzine Nardil® Tranylcypromine Parnate® Isocarboxazid Marplan® Note: Additional medications are cautioned against in people taking Monoamine oxidase inhibitors (MAOI), including other opioids (beyond what is mentioned in the chart above), most classes of antidepressants and other stimulants (beyond what is mentioned in the chart above). -

Xenazine (Tetrabenazine) Policy Number: C3894A
Prior Authorization Criteria Xenazine (tetrabenazine) Policy Number: C3894A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 02/2019 02/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL J8499 MCP MCP-075 PRODUCTS AFFECTED: Oral (tablets) DRUG CLASS: Central Monoamine-Depleting Agent; Vesicular Monoamine Transporter 2 (VMAT2) Inhibitor ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Specialty Pharmacy AVAILABLE DOSAGE FORMS: Tablets: 12.5 mg, 25 mg FDA-APPROVED USES: Chorea associated with Huntington’s disease COMPENDIAL APPROVED OFF-LABELED USES: Tardive dyskinesia in adults, Tourette's syndrome (TS or Gilles de la Tourette's syndrome) COVERAGE CRITERIA: INITIAL AUTHORIZATION DIAGNOSIS: Chorea associated with Huntington’s Disease; Tardive Dyskinesia; Tourette's syndrome REQUIRED MEDICAL INFORMATION: A. CHOREA ASSOCIATED WITH HUNTINGTON’S DISEASE: 1. Diagnosis of Huntington’s disease with chorea symptoms confirmed by documentation of: (a) Huntington Disease Mutation Analysis: indicating an expanded CAG repeat (≥ 36) in the huntington gene (HTT) (also known as HD gene), OR (b)A positive family history of HD, with autosomal dominant inheritance pattern AND 2. Documented trial of at least one alternative treatment (typical neuroleptics, atypical antipsychotics, atypical antipsychotics, benzodiazepines, or amantadine) AND 3. STABLE psychiatric status: Member does not have risk for suicidal or violent behavior and does not have untreated or inadequately treated depression AND 4. If member has a history of depression and/or suicidal ideation: An evaluation by a neurologist or behavioral health provider prior to starting therapy is required AND member is counseled on receiving treatment and follow-up assessment for psychiatric condition from the Prescriber (neurologist) or behavioral health provider while on therapy. -

Drug Interactions Mechanisms and Clinical Relevance Jonathan E
Drug Interactions Mechanisms and Clinical Relevance Jonathan E. Alpert, MD, PhD Dorothy and Marty Silverman Department Chair Department of Psychiatry and Behavioral Sciences Professor of Psychiatry, Neuroscience, and Pediatrics Montefiore Medical Center Albert Einstein College of Medicine Psychopharmacology 2020 www.mghcme.org Disclosures Speaker’s honoraria: American Society of Clinical Psychopharmacology, American Psychiatric Association, Eli Lilly & Co., LIJ/Zucker-Hillside, Nevada Psychiatric Association, New York University, North Shore Medical Center, Organon Inc., Psicofarma, Primedia, Reed Medical Education, University of Louisville, Xian-Janssen Royalties: Belvoir Publishing, Marcel Dekker, Institut la Conference Hippocrate Consultant fees: Consulting Medical Associates, Luye Pharmaceuticals, PamLab LLC, Pharmavite Research support: Abbott Labs, Alkermes, Aspect Medical Systems, Astra- Zeneca, Axsome Therapeutics, Bristol-Myers Squibb, Cephalon, Eli Lilly & Co., Forest Pharmaceuticals, GlaxoSmithKline, J&J Pharmaceuticals, Lichtwer Pharma, Lorex Pharmaceuticals, NARSAD, NIH, Novartis, Organon, Otsuka, PamLab LLC, PCORI, Pharmavite, Roche Laboratories, Solvay Pharma, Sanofi/Synthelabo, Wyeth-Ayerst Laboratories www.mghcme.org Drug Interactions • Ubiquitous polypharmacy • Treatment of psychiatric conditions among medically ill • Use of dietary health supplements/OTCs • Focus on preventable drug errors • Advances in pharmacokinetics and pharmacodynamics and in bioinformatics • Application of bioinformatics to large populations •