209241Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Journal of Pharmaceutical Research Mathur Et Al
World Journal of Pharmaceutical Research Mathur et al . World Journal of Pharmaceutical SJIF ResearchImpact Factor 8.074 Volume 7, Issue 16, 111-124. Review Article ISSN 2277– 7105 ADRS DUE TO ANTIPSYCHOTIC DRUGS: A REVIEW Prashant Mathur*1 and Waseem Yahya2 1,2Department of Pharmacy Practice Shri Guru Ram Rai Institute of Technology and Science, Patel Nagar (248001), Dehradun, Uttarakhand. INTRODUCTION Article Received on 28 June 2018, WHO defines an ADR as ―any response to a drug which is noxious and Revised on 18 July 2018, unintended, and which occurs at doses normally used in man for Accepted on 08 August 2018, DOI: 10.20959/wjpr201816-12706 prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function‖.[1] The antipsychotic drugs are chemically *Corresponding Author diverse but have the common property of alleviating the symptoms of [2] Prashant Mathur organic as well as functional psychosis. Antipsychotics are among Department of Pharmacy the most effective drugs used in psychiatry in the maintenance therapy Practice Shri Guru Ram Rai of schizophrenia, mania, or in acute psychotic reactions.[3] These drugs Institute of Technology and are also capable of causing a wide range of potential adverse drug Science, Patel Nagar (248001), Dehradun, reactions that can lead to non-compliance that can impair quality of Uttarakhand. life, may cause stigma and physical morbidity which may lead to discontinuation of medication and in extreme cases may be fatal.[4] Antipsychotic drugs have a high therapeutic -

2D6 Substrates 2D6 Inhibitors 2D6 Inducers
Physician Guidelines: Drugs Metabolized by Cytochrome P450’s 1 2D6 Substrates Acetaminophen Captopril Dextroamphetamine Fluphenazine Methoxyphenamine Paroxetine Tacrine Ajmaline Carteolol Dextromethorphan Fluvoxamine Metoclopramide Perhexiline Tamoxifen Alprenolol Carvedilol Diazinon Galantamine Metoprolol Perphenazine Tamsulosin Amiflamine Cevimeline Dihydrocodeine Guanoxan Mexiletine Phenacetin Thioridazine Amitriptyline Chloropromazine Diltiazem Haloperidol Mianserin Phenformin Timolol Amphetamine Chlorpheniramine Diprafenone Hydrocodone Minaprine Procainamide Tolterodine Amprenavir Chlorpyrifos Dolasetron Ibogaine Mirtazapine Promethazine Tradodone Aprindine Cinnarizine Donepezil Iloperidone Nefazodone Propafenone Tramadol Aripiprazole Citalopram Doxepin Imipramine Nifedipine Propranolol Trimipramine Atomoxetine Clomipramine Encainide Indoramin Nisoldipine Quanoxan Tropisetron Benztropine Clozapine Ethylmorphine Lidocaine Norcodeine Quetiapine Venlafaxine Bisoprolol Codeine Ezlopitant Loratidine Nortriptyline Ranitidine Verapamil Brofaramine Debrisoquine Flecainide Maprotline olanzapine Remoxipride Zotepine Bufuralol Delavirdine Flunarizine Mequitazine Ondansetron Risperidone Zuclopenthixol Bunitrolol Desipramine Fluoxetine Methadone Oxycodone Sertraline Butylamphetamine Dexfenfluramine Fluperlapine Methamphetamine Parathion Sparteine 2D6 Inhibitors Ajmaline Chlorpromazine Diphenhydramine Indinavir Mibefradil Pimozide Terfenadine Amiodarone Cimetidine Doxorubicin Lasoprazole Moclobemide Quinidine Thioridazine Amitriptyline Cisapride -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -
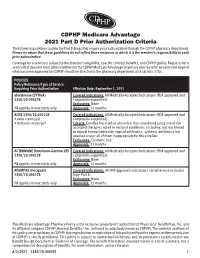
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -

Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone -

(Xenazine); Deutetrabenazine (Austedo); Valbenazine
tetrabenazine (Xenazine ®); deutetrabenazine (Austedo ™); valbenazine (Ingrezza ™) EOCCO POLICY Po licy Type: PA/SP Pharmacy Coverage Policy: EOCCO157 Description Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) are reversible vesicular monoamine transporter 2 (VMAT2) inhibitors that act by regulating monoamine uptake from the cytoplasm to the synaptic vesicle. Its mechanism of action in Tardive dyskinesia or chorea-reduction is unknown . Length of Authorization Initial (Tardive dyskinesia): Three months Initial (Chorea associated with Huntington’s disease): 12 months Renewal: 12 months Quantity limits Product Name Dosage Form Indication Quantity Limit 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with tetrabenazine (Xenazine) Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 12.5 mg Chorea associated with 60 tablets/30 days 25 mg Huntington’s disease Chorea associated with generic tetrabenazine Huntington’s disease, 25 mg genotyped extensive 120 tablets/30 days and intermediate metabolizers 6 mg Tardive dyskinesia in adults; Chorea 30 tablets/30 days deutetrabenazine (Austedo) 9 mg associated with 12 mg Huntington’s disease 120 tablets/30 days 40 mg 30 capsules/30 days; valbenazine (Ingrezza) Tardive Dyskinesia 80 mg 4-week Initiation Pack Initial Evaluation I. Tetrabenazine (Xenazine), deutetrabenazine (Austedo) and valbenazine (Ingrezza) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Medication is prescribed by, or in consultation with, a neurologist or psychiatrist; AND C. Medication will not be used in combination with another VMAT2 inhibitor [e.g. tetrabenazine (Xenazine), deutetrabenazine (Austedo) valbenazine (Ingrezza)], monoamine oxidase inhibitor (MAOI) [e.g. -

Mechanisms of Action of Antipsychotic Drugs Of
302 Current Neuropharmacology, 2009, 7, 302-314 Mechanisms of Action of Antipsychotic Drugs of Different Classes, Refractoriness to Therapeutic Effects of Classical Neuroleptics, and Individual Variation in Sensitivity to their Actions: PART I R. Miller* Otago Centre for Theoretical Studies in Psychiatry and Neuroscience (OCTSPAN), Department of Anatomy and Struc- tural Biology, School of Medical Sciences, University of Otago, P.O.Box 913, Dunedin, New Zealand Abstract: Many issues remain unresolved about antipsychotic drugs. Their therapeutic potency scales with affinity for dopamine D2 receptors, but there are indications that they act indirectly, with dopamine D1 receptors (and others) as pos- sible ultimate targets. Classical neuroleptic drugs disinhibit striatal cholinergic interneurones and increase acetyl choline release. Their effects may then depend on stimulation of muscarinic receptors on principle striatal neurones (M4 recep- tors, with reduction of cAMP formation, for therapeutic effects; M1 receptors for motor side effects). Many psychotic pa- tients do not benefit from neuroleptic drugs, or develop resistance to them during prolonged treatment, but respond well to clozapine. For patients who do respond, there is a wide (>ten-fold) range in optimal doses. Refractoriness or low sensitiv- ity to antipsychotic effects (and other pathologies) could then arise from low density of cholinergic interneurones. Clozap- ine probably owes its special actions to direct stimulation of M4 receptors, a mechanism available when indirect action is lost. Key Words: Antipsychotic drugs, neuroleptic drugs, cholinergic interneurones, D1 receptors, D2 receptors, muscarinic M1 receptors, muscarinic M4 receptors, neuroleptic threshold, atypical antipsychotic agents. 1. INTRODUCTION these drugs. Guidelines for dosage, and dose equivalences between different drugs have been based on group averages The first antipsychotic drug - chlorpromazine - was dis- derived from dose-finding trials. -

Journal of Pharmaceutical and Pharmacological Sciences Jaithliya T
Journal of Pharmaceutical and Pharmacological Sciences Jaithliya T. J Pharma Pharma Sci 02: JPPS 122. Case Report DOI:10.29011/2574-7711.100022 Ashwagandha-The Nature’s Gift to Mankind Tanvay Jaithliya* Department of Pharmacy, Mewar University, Gangrar (Chittorgarh), India *Corresponding author: Jaithliya T, Department of Pharmacy, Mewar University, Gangrar (Chittorgarh) India. Tel: +91 01471291148; E-mail: [email protected] Citation: Jaithliya T (2017) Ashwagandha-The Nature’s Gift to Mankind. J Pharma Pharma Sci 02: 122. DOI: 10.29011/2574-7711.100022 Received Date: 15 March, 2017; Accepted Date: 10 April, 2017; Published Date: 17 April, 2017 Withania somnifera commonly known as Ashwagandha, In- Sindh, Gujarat and Rajasthan. It is also found in Nepal, China and dian Ginseng, poison gooseberry or winter cherry is a plant in the Yemen. solanaceae family or night shade family. It is used as one of the most powerful herbs in Ayurvedic healing, has been used since ancient times for a wide variety of conditions, and is most well- known for its restorative benefits. Traditionally, it is believed that a person who consumes this herbal medicine will gain horse like strength and vitality. Pathology Ashwagandha is prone to several pests and diseases. Leaf spot disease caused by alternariaalternata Is the most prevalent disease, which is most severe in the plains of Punjab, Haryana, Jammu and Kashmir and Himachal Pradesh? Bio deterioration of its pharmaceutically active components during leaf spot disease Description has been reported. This species is short, tender perennial shrub growing 14-30 Culinary Use inches tall. Leaves are dull green, elliptic, usually up to 10-12 cm long. -

170 Limited Use of Anticholinergic Drugs For
170 Penning-van Beest F1, Sukel M1, Reilly K2, Kopp Z2, Erkens J1, Herings R1 1. PHARMO Institute, 2. Pfizer Inc LIMITED USE OF ANTICHOLINERGIC DRUGS FOR OVERACTIVE BLADDER: A PHARMO STUDY Hypothesis / aims of study The aim of the study was to determine the prevalence of use of anticholinergic drugs for overactive bladder (OAB) in men and women in the Netherlands in the period 1998-2003. Study design, materials and methods Data were obtained from the PHARMO Record Linkage System, which includes patient centric data of drug-dispensing records and hospital records of more than one million patients in the Netherlands. Currently four anticholinergic drugs are available on the Dutch market for the treatment of OAB: tolterodine immediate release (IR), since 1998, tolterodine extended release (ER), since 2001, oxybutynin, since 1986, and flavoxate, since 1979. All patients who were ever prescribed these OAB drugs in the period January 1998 until December 2003 were included in the study cohort. The prevalence of use of tolterodine ER, tolterodine IR, oxybutynin and flavoxate was determined per calendar year, stratified by gender, by counting the number of patients having a dispensing with a duration of use including a single fixed day a year. Results The number of OAB drug users included in the study cohort increased from about 3,800 in 1998 to 5,000 in 2003. About 60% of the OAB drug users in the study cohort were women and about 42% of the OAB drug users were 70 years or older. The use of OAB drugs increased from 100 users per 100,000 men in 1998 to 140 users per 100,000 men in 2003 (table).