CASE REPORT Osteopathic Manipulative Treatment to Resolve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Occipitomastoid Suture As a Novel Landmark to Identify The
The Occipitomastoid Suture as a Novel Landmark to Identify the Occipital Groove and Proximal Segment of the Occipital Artery Halima Tabani MD; Sirin Gandhi MD; Roberto Rodriguez Rubio MD; Michael T. Lawton MD; Arnau Benet M.D. University of California, San Francisco Introduction Results Conclusions The occipital artery (OA) is commonly used as a In 71.5% of the specimens the OA ran in a groove, The OMS is a key landmark for localizing the donor for posterior circulation bypass procedures. while it carved an impression in the rest of the proximal OA. The OMS can be followed inferiorly Localization of OA during harvesting is important to cases (28.5%). In none of the specimens the OA prevent inadvertent damage to the donor. The was found to run in a bony canal. In 68.6% of the from the asterion to the OA groove, thereby proximal portion of the OA is found in the occipital cases, the OMS was found to be medial to the OA localizing the proximal OA. Inadvertent damage to groove. The occipitomastoid suture (OMS) is located groove or impression while in 31.4%, it ran the proximal OA may be avoided by identifying the between the occipital bone and the mastoid portion centrally through the OA groove or impression OMS and dissecting medial to it, since in majority of the temporal bone. This study aimed to assess (Figure 1). The OMS was never found lateral to the of cases, the proximal OA will be located lateral to the relationship between the OMS and the occipital OA it groove, in order to facilitate localization of the proximal portion of OA while harvesting it for bypass Learning Objectives 1.To understand the relationship between the Figure 1 occipital groove and the occiptomastoid suture 2.To understand the potential use of occipitomastoid suture as a landmark to identify the proximal Methods segment of OA in the occipital groove Thirty-five dry skulls were assessed bilaterally (n=70) to study the bony landmarks that can be used to identify and locate the proximal segment of OA. -

Chapter 22 TEMPORAL BONE FRACTURES
Temporal Bone Fractures Chapter 22 TEMPORAL BONE FRACTURES † CARLOS R. ESQUIVEL, MD,* AND NICHOLAS J. SCALZITTI, MD INTRODUCTION INITIAL EVALUATION FRACTURE CLASSIFICATION RADIOGRAPHIC EVALUATION MANAGEMENT OF INJURIES Facial Nerve Injury Hearing Loss Cerebrospinal Fluid Leak and Use of Antibiotic Therapy SPECIAL CONSIDERATIONS FOR WARTIME INJURIES Acute Management CASE PRESENTATIONS Case Study 22-1 Case Study 22-2 *Lieutenant Colonel (Retired), Medical Corps, US Air Force; Clinical Director, Department of Defense, Hearing Center of Excellence, Wilford Hall Ambulatory Surgical Center, 59th Medical Wing, Lackland Air Force Base, Texas 78236 †Captain, Medical Corps, US Air Force; Resident Otolaryngologist, San Antonio Military Medical Center, 3551 Roger Brooke Drive, Joint Base San Antonio, Fort Sam Houston, Texas 78234 267 Otolaryngology/Head and Neck Combat Casualty Care INTRODUCTION The conflicts in Iraq and Afghanistan have resulted age to the deeper structures of the middle and inner in large numbers of head and neck injuries to NATO ear, as well as the brain. Special arrangement of the (North Atlantic Treaty Organization) and Afghan ser- outer and middle ear is essential for efficient capture vice members. Improvised explosive devices, mortars, and transduction of sound energy to the inner ear in and suicide bombs are the weapons of choice during order for hearing to take place. This efficiency relies this conflict. The resultant injuries are high-velocity on a functional anatomical relationship of a taut tym- projectile injuries. Relatively little is known about the panic membrane connected to a mobile, intact ossicular precise incidence and prevalence of isolated closed chain. Traumatic forces that disrupt this relationship temporal bone fractures in theater. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO Abstract This paper will explore how bony and soft tissue dysfunctions, at various Motor codes (head region) locations, can affect The Spinal Accessory Nerve (CN XI). The resultant possible neuromusculoskeletal abnor- Posterior limb of internal capsule malities will be discussed, including specific descriptions of the dysfunctions, along with various types of osteopathic DBOUSSFigon In pyramids manipulative medicine (OMM) as Nucleus amblguus treatment measures. IX Lateral X corticospinal tract The Spinal Root of CN XI is derived XI Jugular from motor cells in the lateral ventral foramen Accessory nucleus columns of the gray matter of the first five or six segments of the spinal cord (1-Page 944). They are approximately in line with nucleus ambiguus. These Flgure XI-I Branchtal Motot Component of Accessory Nerve (Elevated Brain Sterol cells are called the spinal nuclei of the accessory nerve (2-Page 105). Laterally, the motor roots exit the spinal cord about midway between the dorsal and ventral roots. Each inferior root joins with the one above until a trunk is formed that extends superiorly and laterally through the foramen magnum posterior to the Jugular lor•men vertebral artery, bilaterally (XI in Figure Accessory (spinal XI-1). The Cranial Root of CN XI consists nucleus CI-CS of a few axons whose cell bodies reside in the caudal part of nucleus ambiguus Sternomesiod (cull (3-Page 144). These join to form the Lent or scapulae cranial accessory trunk which enters the Trap-axles jugular foramen with the spinal trunk. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1
Open Access Review Article DOI: 10.7759/cureus.8697 The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1 Bruno Bordoni 1 1. Physical Medicine and Rehabilitation, Foundation Don Carlo Gnocchi, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract In osteopathic manual medicine (OMM), there are several approaches for patient assessment and treatment. One of these is the five diaphragm model (tentorium cerebelli, tongue, thoracic outlet, diaphragm, and pelvic floor), whose foundations are part of another historical model: respiratory-circulatory. The myofascial continuity, anterior and posterior, supports the notion the human body cannot be divided into segments but is a continuum of matter, fluids, and emotions. In this first part, the neurological relationships of the tentorium cerebelli and the lingual muscle complex will be highlighted, underlining the complex interactions and anastomoses, through the most current scientific data and an accurate review of the topic. In the second part, I will describe the neurological relationships of the thoracic outlet, the respiratory diaphragm and the pelvic floor, with clinical reflections. In literature, to my knowledge, it is the first time that the different neurological relationships of these anatomical segments have been discussed, highlighting the constant neurological continuity of the five diaphragms. Categories: Medical Education, Anatomy, Osteopathic Medicine Keywords: diaphragm, osteopathic, fascia, myofascial, fascintegrity, -

PRACTICAL Practical
PRACTICAL Practical 140 Practical PRACTICAL Contents Craniometry Maximum Cranial Length Maximum Cranial Breadth Maximum Bizygomatic Breadth Greatest Occipital Breadth Upper Facial Height Nasal Breadth Nasal Index Cranial Index Osteometry Measurements of long bones: lengths, minimum/least circumference and calibre index. Learning Objectives After reading this practical manual you will be able to: define craniometry and osteometery; know various craniometric and osteometric landmarks and measurements; get an idea of various tools and techniques used by Anthropologists for measurement of human cranium and long bones; and calculate various craniometric and osteometric indices. CRANIOMETRY Skull is the upper most part of our skeleton consisting of head and face. The lower part of the facial skeleton is constituted by a single loose bone, the mandible. The skeleton of a skull without mandible is called a cranium. The brain box, i.e. the neurocranium, is also designated as calvarium; and the top most part of the skull i.e. the skull cap is designated as Calotte. Fig. 1: Skull and its different parts (a) Skull; (b) Cranium; (c) Calotte Source: Mukherjee et al., 2009 141 Practical For the purpose of morphological study a human cranium is observed from five different positions or normas viz., norma verticalis,norma frontalis, norma lateralis, norma occipitalis and norma basalis. Such studies of the normas help understand the shape of a cranium from particular views. Secondly, such study helps to observe relative contribution of different cranial bones in structuring a particular aspect. Thirdly, different surface characters of a particular aspect of the cranium can be studied. Finally, studies of the normas are essential, rather indispensable, in comparative craniology with apes’ crania and also in comprehending evolutionary changes in cranium. -
Axial Skeleton 214 7.7 Development of the Axial Skeleton 214
SKELETAL SYSTEM OUTLINE 7.1 Skull 175 7.1a Views of the Skull and Landmark Features 176 7.1b Sutures 183 7.1c Bones of the Cranium 185 7 7.1d Bones of the Face 194 7.1e Nasal Complex 198 7.1f Paranasal Sinuses 199 7.1g Orbital Complex 200 Axial 7.1h Bones Associated with the Skull 201 7.2 Sex Differences in the Skull 201 7.3 Aging of the Skull 201 Skeleton 7.4 Vertebral Column 204 7.4a Divisions of the Vertebral Column 204 7.4b Spinal Curvatures 205 7.4c Vertebral Anatomy 206 7.5 Thoracic Cage 212 7.5a Sternum 213 7.5b Ribs 213 7.6 Aging of the Axial Skeleton 214 7.7 Development of the Axial Skeleton 214 MODULE 5: SKELETAL SYSTEM mck78097_ch07_173-219.indd 173 2/14/11 4:58 PM 174 Chapter Seven Axial Skeleton he bones of the skeleton form an internal framework to support The skeletal system is divided into two parts: the axial skele- T soft tissues, protect vital organs, bear the body’s weight, and ton and the appendicular skeleton. The axial skeleton is composed help us move. Without a bony skeleton, we would collapse into a of the bones along the central axis of the body, which we com- formless mass. Typically, there are 206 bones in an adult skeleton, monly divide into three regions—the skull, the vertebral column, although this number varies in some individuals. A larger number of and the thoracic cage (figure 7.1). The appendicular skeleton bones appear to be present at birth, but the total number decreases consists of the bones of the appendages (upper and lower limbs), with growth and maturity as some separate bones fuse. -

TO ELABORATE CONCEPT of SEVANI with the HELP of MODERN ANATOMY Dr
Review Article International Ayurvedic Medical Journal ISSN:2320 5091 TO ELABORATE CONCEPT OF SEVANI WITH THE HELP OF MODERN ANATOMY Dr. Budruk Pramod Appasaheb M.D. Sharir Rachna, L.L.B.(spl), Principal- Hon.Shri. Annasaheb Dange Ayurved Medical College, Ashta. Tal- Walwa, Dist- Sangli, Maharashtra, India ABSTRACT Ayurveda gives new Idea about human being in case of Anatomy, Physiology & other subjects also. Ayurvedokth Rachana Sharir describes about various terminology. In fifth chapter of Sharirsthan Susrut described various parts of the body. Not only various parts of the body, but also number of these parts or organs, is nicely given in this Sharir sankhya vyakarana sharir Ad- hayaya. Anaga, Pratnyaga, Twacha, Kala, Sira, Snayu, Dhamani are described with its numbers & distribution of them. Sivani is the one of structure present in the body. There is Sapta-Sevani present in the body. Structure of Sevani & also importance of it is given by Ayurveda. Though Sevani is mentioned in one sloka, but it has very much important.Its importance is given by comparative study with modern Science. Division of the skull is done by these sevani, as given in modern science. Sevani word gives two references. First is a sapt Shivayna available for the sevani & second in case of sandhi sharir. There is confusion regarding various terms as sevani or simant. With the help of this article I am trying to clarify these concepts with the help of mod- ern science. Keywords: Sevani, Septasevani, Sivani, Tunnasevani,Sutures INTRODUCTION We know that structural & functional science, these structures we can easily corre- unit of the body is cell. -

A Study on the Development of Cranial Traction Therapy Program for Facial Non-Symmertric Correction -Utilize Delphi Technique
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 27 October 2020 doi:10.20944/preprints202010.0537.v1 Article A Study on the Development of Cranial Traction therapy Program for Facial Non-symmertric Correction -Utilize Delphi technique Sung-Yeon Park 1, Hea-Ju Hwang2* Kyu-Nam Park3* 1,2 Graduate School of Medicine, CHA University, Seongnam-si, Gyeonggi-do 13503, Korea 3 Graduate School of Public Health Industry, CHA University, Seongnam-si, Gyeonggi-do 13503, Korea * Correspondence: [email protected] (H.-J.H.); [email protected] (K.-N.P.) Abstract: The purpose of this study is to develop a cranial traction therapy program to help correct facial asymmetry of the hard tissues through the means of the treatment of soft tissues—a non-surgical therapeutic method for the correcting of facial asymmetry. We have formed a group of experts who have agreed to the study. In the primary survey, open questions were used. In the second survey, the results of the first survey were summarized and the degree of agreement was presented to the questions in each category. In the third survey, we conducted a statistical analysis of the degree of agreement on each item of question. All surveys also performed email. The distribution was calculated using the SPSS (ver.23.0) program, and the mean difference between the result and X² was calculated. The significance level was set to p<.05. Most of the questions attained a certain level of consensus by the experts (average of 4.0 or higher), it can be said that most are important and suitable questions. -
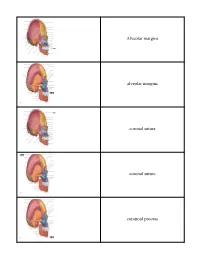
Crista Galli (Part of Cribriform Plate of Ethmoid Bone)
Alveolar margins alveolar margins coronal suture coronal suture coronoid process crista galli (part of cribriform plate of ethmoid bone) ethmoid bone ethmoid bone ethmoid bone external acoustic meatus external occipital crest external occipital protuberance external occipital protuberance frontal bone frontal bone frontal bone frontal sinus frontal squama of frontal bone frontonasal suture glabella incisive fossa inferior nasal concha inferior nuchal line inferior orbital fissure infraorbital foramen internal acoustic meatus lacrimal bone lacrimal bone lacrimal fossa lambdoid suture lambdoid suture lambdoid suture mandible mandible mandible mandibular angle mandibular condyle mandibular foramen mandibular notch mandibular ramus mastoid process of the temporal bone mastoid process of the temporal bone maxilla maxilla maxilla mental foramen mental foramen middle nasal concha of ethmoid bone nasal bone nasal bone nasal bone nasal bone occipital bone occipital bone occipital bone occipitomastoid suture occipitomastoid suture occipitomastoid suture occipital condyle optic canal optic canal palatine bone palatine process of maxilla parietal bone parietal bone parietal bone parietal bone perpendicular plate of ethmoid bone pterygoid process of sphenoid bone sagittal suture sella turcica of sphenoid bone Sphenoid bone (greater wing) spehnoid bone (greater wing) sphenoid bone (greater wing) sphenoid bone (greater wing) sphenoid sinus sphenoid sinus squamous suture squamous suture styloid process of temporal bone superior nuchal line superior orbital fissure supraorbital foramen (notch) supraorbital margin sutural bone temporal bone temporal bone temporal bone vomer bone vomer bone zygomatic bone zygomatic bone. -
Neural Manipulation 1 Preparation 1
Neural Manipulation 1 Preparation 1. Review this video 2. Read: Trauma: An Osteopathic Approach 3. Review these slides Important terms and structures important to study prior to NM1 attendance. Relationship of Spinal Nerves to Dura Brachial Plexus ~ Lumbar Plexus ~ Sacral Plexus Layers of the intracranial membrane system Cranial Suture Anatomy – coronal, sagittal, lamdoid Craniospinal Juncture Anatomy Pelvic Ligaments – sacrotuberous, sacrospinous Tentorium Cerebelli – anatomy of intracranial attachments Brachial Plexus Femoral Nerve Sciatic Nerve NM1 Preparation Quiz Answers at the end 1. The coronal suture is between what 2 bones? 2. The occipito-mastoid suture/jugular foramen is between what 2 bones? 3. The falx cerebri is mostly under what suture? 4. The attachments of the tentorium cerebelli are: a. frontal bone, petrouss part of temporal bone, occiput b. occiput, parietal, temporal, bones, anterior and posterior clinoid processes of sphenoid bone c. occiput, parietal and temporal bones, maxilla Neural Manipulation Neural Manipulation (NM) is a gentle hands-on therapy which helps to free up the nerves and the connective tissue around the nerves (dura mater), the bones around the brain (cranium) so that the nervous system functions better. (Barral & Croibier 2007) “Neural” refers to the nervous system of the body, which includes the brain, spinal cord, nerves of upper and lower extremities, trunk and head. Cranial Anatomy Frontal bone Coronal suture Parietal bones Sagittal suture Sutures The sutures provide for growth and elasticity of the newborn skull. The begin to close after 3-4 months, however the anterior fontanelle will not close until 20 months (average). They can be difficult to palpate after 6 months.