Chapter 22 TEMPORAL BONE FRACTURES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Occipitomastoid Suture As a Novel Landmark to Identify The
The Occipitomastoid Suture as a Novel Landmark to Identify the Occipital Groove and Proximal Segment of the Occipital Artery Halima Tabani MD; Sirin Gandhi MD; Roberto Rodriguez Rubio MD; Michael T. Lawton MD; Arnau Benet M.D. University of California, San Francisco Introduction Results Conclusions The occipital artery (OA) is commonly used as a In 71.5% of the specimens the OA ran in a groove, The OMS is a key landmark for localizing the donor for posterior circulation bypass procedures. while it carved an impression in the rest of the proximal OA. The OMS can be followed inferiorly Localization of OA during harvesting is important to cases (28.5%). In none of the specimens the OA prevent inadvertent damage to the donor. The was found to run in a bony canal. In 68.6% of the from the asterion to the OA groove, thereby proximal portion of the OA is found in the occipital cases, the OMS was found to be medial to the OA localizing the proximal OA. Inadvertent damage to groove. The occipitomastoid suture (OMS) is located groove or impression while in 31.4%, it ran the proximal OA may be avoided by identifying the between the occipital bone and the mastoid portion centrally through the OA groove or impression OMS and dissecting medial to it, since in majority of the temporal bone. This study aimed to assess (Figure 1). The OMS was never found lateral to the of cases, the proximal OA will be located lateral to the relationship between the OMS and the occipital OA it groove, in order to facilitate localization of the proximal portion of OA while harvesting it for bypass Learning Objectives 1.To understand the relationship between the Figure 1 occipital groove and the occiptomastoid suture 2.To understand the potential use of occipitomastoid suture as a landmark to identify the proximal Methods segment of OA in the occipital groove Thirty-five dry skulls were assessed bilaterally (n=70) to study the bony landmarks that can be used to identify and locate the proximal segment of OA. -

Facial Nerve Electrodiagnostics for Patients with Facial Palsy: a Clinical Practice Guideline
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Helsingin yliopiston digitaalinen arkisto European Archives of Oto-Rhino-Laryngology (2020) 277:1855–1874 https://doi.org/10.1007/s00405-020-05949-1 REVIEW ARTICLE Facial nerve electrodiagnostics for patients with facial palsy: a clinical practice guideline Orlando Guntinas‑Lichius1,2,3 · Gerd Fabian Volk1,2 · Kerry D. Olsen4 · Antti A. Mäkitie5 · Carl E. Silver6 · Mark E. Zafereo7 · Alessandra Rinaldo8 · Gregory W. Randolph9 · Ricard Simo10 · Ashok R. Shaha11 · Vincent Vander Poorten3,12 · Alfo Ferlito13 Received: 14 March 2020 / Accepted: 27 March 2020 / Published online: 8 April 2020 © The Author(s) 2020 Abstract Purpose Facial nerve electrodiagnostics is a well-established and important tool for decision making in patients with facial nerve diseases. Nevertheless, many otorhinolaryngologist—head and neck surgeons do not routinely use facial nerve electro- diagnostics. This may be due to a current lack of agreement on methodology, interpretation, validity, and clinical application. Electrophysiological analyses of the facial nerve and the mimic muscles can assist in diagnosis, assess the lesion severity, and aid in decision making. With acute facial palsy, it is a valuable tool for predicting recovery. Methods This paper presents a guideline prepared by members of the International Head and Neck Scientifc Group and of the Multidisciplinary Salivary Gland Society for use in cases of peripheral facial nerve disorders based on a systematic literature search. Results Required equipment, practical implementation, and interpretation of the results of facial nerve electrodiagnostics are presented. Conclusion The aim of this guideline is to inform all involved parties (i.e. -

Cleidocranial Dysplasia- a Case Report
Case Report Cleidocranial Dysplasia- A Case Report Akhilanand Chaurasia Department of Oral Medicine & Radiology, Faculty of Dental Sciences, King George Medical University, Lucknow E-mail: [email protected] ABSTRACT Cleidocranial dysplasia is a rare congenital disease. It is characterized by autosomal dominant inheritance pattern which is caused due to mutations in the Cbfa1 gene (Runx2) located on chromosome 6p21. It primarily affects bones which are formedby intra-membranous ossification and have equal sex distribution. It is also known as Marie and Sainton disease, Mutational dysostosis and cleidocranialdysostosis. The skeletal deformities of cleidocranial dysplasia are characterized by partial or complete absence of clavicles, late closure of the fontanels, presence of open skull sutures and multiple wormian bones. This rare syndrome is of utmost importance in dentistry due to presence of multiple supernumerary teeth, facial bones deformities and deranged eruption patterns. We are reporting a classical case of cleidocranial dysplasia in 20 year old patient. Keywords: Cleidocranial dysplasia, Marie and Sainton disease, Mutational dysostosis, Cleidocranialdysostosis, Autosomal dominant Access this article online mandibular symphysis are less common findings of Quick Response cleidocranial dysostosis1,10,11. Code: Website: Dental findings in cleidocranialdysostosis are www.innovativepublication.com characterized by a decreased eruptive force of both primary and permanent dentition, prolonged retention of primary teeth12 and an increase in odontogenesis DOI: 10.5958/2395-6194.2015.00009.0 leading to an excessive number of supernumerary teeth13. The clinical findings of cleidocranialdysostosis although present at birth are often either missed or INTRODUCTION diagnosed at a much later time. Cleidocranialdysostosis Cleidocranialdysostosis is a rare congenital defect may be identified by family history, excessive mobility primarily affecting bones which undergo intra- of shoulders and radiographic pathognomonic findings membranous ossification i.e. -

Morphological and Topographical Study of Wormian Bones in Cadaver Dry Skulls
Original article Morphological and topographical study of Wormian bones in cadaver dry skulls Murlimanju, BV.*, Prabhu, LV., Ashraf, CM., Kumar, CG., Rai, R. and Maheshwari, C. Department of Anatomy, Manipal University, Centre for Basic Sciences, Kasturba Medical College, Mangalore, India *E-mail: [email protected] Abstract Introduction: The Wormian bones are formations associated with insufficient rate of suture closure and regarded as epigenetic and hypostotic traits. It was reported that there exists racial variability among the incidence of these bones. In the present study, the aims were to find the incidence of Wormian bones in Indian skulls and to analyze them topographically. Material and methods: The study included 78 human adult dry skulls of Indian population which were obtained from the neuroanatomy laboratory of our institution. They were macroscopically observed for the incidence and topographical distribution of the Wormian bones. Results: The Wormian bones were observed in 57 skulls (73.1%) of our series. Remaining 21 skulls (26.9%) didn’t show these variant bones. They were observed at the lambdoid suture in 56.4% cases (44 skulls; 14-bilateral; 18-right side; 12-left side), at the asterion in 17.9% (14 skulls; 3-bilateral; 2-right side; 9-left side), at the pterion in 11.5% (9 skulls; 4-right side; 5-left side), at the coronal suture in 1.3% (only one skull) and at the sagittal suture in 1.3% cases (only one skull). Conclusion: The current study observed Wormian bones in 73.1% of the cases from Indian population. This incidence rate is slightly higher compared to other reports and may be due to racial variations. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

CASE REPORT Osteopathic Manipulative Treatment to Resolve
CASE REPORT Osteopathic Manipulative Treatment to Resolve Head and Neck Pain After Tooth Extraction Patricia M. Meyer, DO, MS Sharon M. Gustowski, DO, MPH Pain is a common occurrence after tooth extraction and fter dental extraction, the majority of patients have is usually localized to the extraction site. However, clinical Apain lasting less than 1 week that can be controlled experience shows that patients may also have pain in by analgesics. The length, type, and severity of pain vary the head or neck in the weeks after this procedure. The as a result of multiple factors, such as the difficulty of the authors present a case representative of these findings. extraction procedure, the patient’s health status and atti - In the case, cranial and cervical somatic dysfunction in tude, and the patient’s sex. 1 Other pain syndromes that a patient who had undergone tooth extraction was may occur weeks after the procedure—though rare— resolved through the use of osteopathic manipulative include neuropathic pain, temporomandibular disorder, 2,3 treatment. This case emphasizes the need to include a cluster headache, 4,5 and neck and head pain caused by dental history when evaluating head and neck pain as somatic dysfunction. 6,7 Prolonged and nonresolving pain part of comprehensive osteopathic medical care. The should be investigated for such conditions as rheumatologic case can also serve as a foundation for a detailed discus - diseases, tumors, migraine headache, or myofascial pain sion regarding how to effectively incorporate osteopathic syndrome. manipulative treatment into primary care practice for The etiologic characteristics of head and neck pain patients who present with head or neck pain after tooth after dental procedures are multifactorial, depending on extraction. -
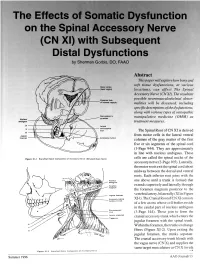
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO Abstract This paper will explore how bony and soft tissue dysfunctions, at various Motor codes (head region) locations, can affect The Spinal Accessory Nerve (CN XI). The resultant possible neuromusculoskeletal abnor- Posterior limb of internal capsule malities will be discussed, including specific descriptions of the dysfunctions, along with various types of osteopathic DBOUSSFigon In pyramids manipulative medicine (OMM) as Nucleus amblguus treatment measures. IX Lateral X corticospinal tract The Spinal Root of CN XI is derived XI Jugular from motor cells in the lateral ventral foramen Accessory nucleus columns of the gray matter of the first five or six segments of the spinal cord (1-Page 944). They are approximately in line with nucleus ambiguus. These Flgure XI-I Branchtal Motot Component of Accessory Nerve (Elevated Brain Sterol cells are called the spinal nuclei of the accessory nerve (2-Page 105). Laterally, the motor roots exit the spinal cord about midway between the dorsal and ventral roots. Each inferior root joins with the one above until a trunk is formed that extends superiorly and laterally through the foramen magnum posterior to the Jugular lor•men vertebral artery, bilaterally (XI in Figure Accessory (spinal XI-1). The Cranial Root of CN XI consists nucleus CI-CS of a few axons whose cell bodies reside in the caudal part of nucleus ambiguus Sternomesiod (cull (3-Page 144). These join to form the Lent or scapulae cranial accessory trunk which enters the Trap-axles jugular foramen with the spinal trunk. -

Supplementary Information For
Supplementary Information for An Abundance of Developmental Anomalies and Abnormalities in Pleistocene People Erik Trinkaus Department of Anthropology, Washington University, Saint Louis MO 63130 Corresponding author: Erik Trinkaus Email: [email protected] This PDF file includes: Supplementary text Figures S1 to S57 Table S1 References 1 to 421 for SI reference citations Introduction Although they have been considered to be an inconvenience for the morphological analysis of human paleontological remains, it has become appreciated that various pathological lesions and other abnormalities or rare variants in human fossil remains might provide insights into Pleistocene human biology and behavior (following similar trends in Holocene bioarcheology). In this context, even though there were earlier paleopathological assessments in monographic treatments of human remains (e.g., 1-3), it has become common to provide details on abnormalities in primary descriptions of human fossils (e.g., 4-12), as well as assessments of specific lesions on known and novel remains [see references in Wu et al. (13, 14) and below]. These works have been joined by doctoral dissertation assessments of patterns of Pleistocene human lesions (e.g., 15-18). The paleopathological attention has been primarily on the documentation and differential diagnosis of the abnormalities of individual fossil remains, leading to the growing paleopathological literature on Pleistocene specimens and their lesions. There have been some considerations of the overall patterns of the lesions, but those assessments have been concerned primarily with non-specific stress indicators and traumatic lesions (e.g., 13, 15, 19-21), with variable considerations of issues of survival 1 w ww.pnas.org/cgi/doi/10.1073/pnas.1814989115 and especially the inferred social support of the afflicted (e.g., 22-27). -

Cranial Suture Mesenchymal Stem Cells: Insights and Advances
biomolecules Review Cranial Suture Mesenchymal Stem Cells: Insights and Advances Bo Li 1, Yigan Wang 1, Yi Fan 2, Takehito Ouchi 3 , Zhihe Zhao 1,* and Longjiang Li 4,* 1 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Orthodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] (B.L.); [email protected] (Y.W.) 2 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Cariology and Endodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] 3 Department of Physiology, Tokyo Dental College, Tokyo 1010061, Japan; [email protected] 4 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Head and Neck Oncology, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China * Correspondence: [email protected] (Z.Z.); [email protected] (L.L.) Abstract: The cranial bones constitute the protective structures of the skull, which surround and protect the brain. Due to the limited repair capacity, the reconstruction and regeneration of skull defects are considered as an unmet clinical need and challenge. Previously, it has been proposed that the periosteum and dura mater provide reparative progenitors for cranial bones homeostasis and injury repair. In addition, it has also been speculated that the cranial mesenchymal stem cells reside in the perivascular niche of the diploe, namely, the soft spongy cancellous bone between the interior and exterior layers of cortical bone of the skull, which resembles the skeletal stem cells’ distribution pattern of the long bone within the bone marrow. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Significance of Differences in Patency Among Cranial Sutures ORIGINAL
ORIGINAL CONTRIBUTION Significance of Differences in Patency Among Cranial Sutures Rosanna C. Sabini, DO David E. Elkowitz, DO Objective: To evaluate the gross external characteristics of Because the human body is highly adaptive, and many dif- the coronal, lambdoid, and sagittal sutures in human cadaver ferences exist among sutures,3,7,9 it would be unreasonable to skulls and determine if a difference exists in terms of patency, assume that age is the only factor that contributes to the sex, and age. changes in sutures. Such notions would explain suture mor- phology solely in terms of intrinsic factors,16 such as genetics. Methods: The coronal, lambdoid, and sagittal sutures were Although intrinsic factors may be an influence, extrinsic or described using a modified grading scale to quantify sutural environmental factors such as tensile forces, a growing brain, patency. An open suture was graded as 0, a fused suture as and active muscle demands, are more likely to affect the char- 1, and an obliterated suture as 2, 3, or 4, depending on the acteristics of sutures.1,5,6,9–11,17–20 extent of obliteration. The effects of extrinsic factors on the morphologic changes Results: Thirty-six skulls were examined, including 17 female in sutures is evident.1–3,6,7,9,11,17–20 These changes include an and 19 male (age range, 56–101 y). When compared with the increase in complexity, the number and length of bony inter- sagittal suture, the lambdoid suture was significantly more digitations, and a prolongation of the time to complete suture likely to be patent and least likely to be obliterated. -

Percutaneous Facial Nerve Stimulation JMR 2015; 1(2): 68-69
The Journal of Medical Research 2015; 1(2): 68-69 Mini Review Percutaneous facial nerve stimulation JMR 2015; 1(2): 68-69 March- April Jayita Poduval ISSN: 2395-7565 Associate Professor, Department of ENT, Pondicherry Institute of Medical Sciences, Kalapet, Puducherry- 605014, © 2015, All rights reserved India www.medicinearticle.com Abstract Introduction: Facial nerve paralysis is a commonly encountered clinical entity. Bell’s palsy is the most frequently observed manifestation of facial paralysis, and is diagnosed and treated mainly on the basis of history and clinical examination. Some other cases of facial paralysis would however require more objective, intensive and reliable means of evaluation in order to facilitate optimum management. Method: When the diagnosis of facial paralysis is in doubt, electrodiagnostic tests are a useful method of evaluation. This paper discusses the technique by which these tests are performed using percutaneous facial nerve stimulation. It also discusses the method of interpretation of these test results. Conclusion: Though percutaneous facial nerve stimulation is a reliable and objective method of diagnosis, there are certain limitations to its use which must be borne in mind by the clinician. Keywords: Facial paralysis, Electro diagnostic tests, Facial nerve stimulation. Introduction Electro diagnostic tests were pioneered by Duchenne in 1872 and popularized by Campbell in 1954 [1]. Electro diagnostic tests are employed for the objective evaluation of physiologic injury to nerves and to estimate the prognosis of nerve lesions. Seddon classified nerve injury into 3 broad types- neuropraxia, axonotmesis and neurotmesis [2]. This was further elaborated by Sunderland into 5 degrees- neuropraxia(electrical conduction block), axonotmesis (disruption of the axon with intact endoneurium), disruption of the axon along with perineurium, disruption of the epineurium (partial transection),and disruption of the nerve funicle (complete transection) [3].