Variation of Leptomeningeal Hemorrhage Localizations in Feti
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Occipitomastoid Suture As a Novel Landmark to Identify The
The Occipitomastoid Suture as a Novel Landmark to Identify the Occipital Groove and Proximal Segment of the Occipital Artery Halima Tabani MD; Sirin Gandhi MD; Roberto Rodriguez Rubio MD; Michael T. Lawton MD; Arnau Benet M.D. University of California, San Francisco Introduction Results Conclusions The occipital artery (OA) is commonly used as a In 71.5% of the specimens the OA ran in a groove, The OMS is a key landmark for localizing the donor for posterior circulation bypass procedures. while it carved an impression in the rest of the proximal OA. The OMS can be followed inferiorly Localization of OA during harvesting is important to cases (28.5%). In none of the specimens the OA prevent inadvertent damage to the donor. The was found to run in a bony canal. In 68.6% of the from the asterion to the OA groove, thereby proximal portion of the OA is found in the occipital cases, the OMS was found to be medial to the OA localizing the proximal OA. Inadvertent damage to groove. The occipitomastoid suture (OMS) is located groove or impression while in 31.4%, it ran the proximal OA may be avoided by identifying the between the occipital bone and the mastoid portion centrally through the OA groove or impression OMS and dissecting medial to it, since in majority of the temporal bone. This study aimed to assess (Figure 1). The OMS was never found lateral to the of cases, the proximal OA will be located lateral to the relationship between the OMS and the occipital OA it groove, in order to facilitate localization of the proximal portion of OA while harvesting it for bypass Learning Objectives 1.To understand the relationship between the Figure 1 occipital groove and the occiptomastoid suture 2.To understand the potential use of occipitomastoid suture as a landmark to identify the proximal Methods segment of OA in the occipital groove Thirty-five dry skulls were assessed bilaterally (n=70) to study the bony landmarks that can be used to identify and locate the proximal segment of OA. -

Nervous System - PNS and CNS
Nervous System - PNS AND CNS Locate the following structures on the appropriate model or diagram. Understand the function of ea Neuron Spinal nerves Cerebrum axon cervical plexus cerebral hemisphere dendrite phrenic cerebral cortex cell body gray matter Schwann cell brachial plexus white matter node of Ranvier axillary gyrus (convolution) myelin sheath radial longitudinal fissure neurolemma median falx cerebri Nissl bodies ulnar central sulcus synaptic knobs lateral sulcus synaptic vesicles lumbar plexus frontal lobe femoral parietal lobe Spinal Cord obturator occipital lobe central canal temporal lobe posterior column sacral plexus insula lateral column sciatic corpus callosum anterior column tibial olfactory bulb posterior sulcus common fibular olfactory tract anterior fissure superficial fibular posterior horn deep fibular Diencephalon lateral horn thalamus anterior horn intercostal nerves intermediate mass gray commissure hypothalamus conus medularis Autonomic NS infundibulum dorsal nerve root sympathetic trunk pituitary gland dorsal root ganglion ganglia (paravertebral) pineal gland ventral nerve root mammillary bodies spinal nerve Brainstem optic nerve cauda equina = medulla, pons, mid, optic tract filum terminale cranial nerves optic chiasm Meninges Midbrain dura mater cerebral peduncles Cranial Nerves dural sinus superior colliculus I olfactory epidural space inferior colliculus II optic arachnoid mater III oculomotor subarachnoid space Pons IV trochlear arachnoid granulations (villi) V trigeminal pia mater Medulla Oblongata VI abducens choroid plexus pyramids VII facial denticulate ligament olive VIII vestibulocochlear IX glossopharyngeal Cerebellum X vagus Ventricles cerebellar hemisphere XI accessory lateral ventricles vermis XII hypoglossal septum pellucidum transverse fissure third ventricle tentorium cerebelli cerebral aqueduct falx cerebelli fourth ventricle arbor vitae. -

Chapter 22 TEMPORAL BONE FRACTURES
Temporal Bone Fractures Chapter 22 TEMPORAL BONE FRACTURES † CARLOS R. ESQUIVEL, MD,* AND NICHOLAS J. SCALZITTI, MD INTRODUCTION INITIAL EVALUATION FRACTURE CLASSIFICATION RADIOGRAPHIC EVALUATION MANAGEMENT OF INJURIES Facial Nerve Injury Hearing Loss Cerebrospinal Fluid Leak and Use of Antibiotic Therapy SPECIAL CONSIDERATIONS FOR WARTIME INJURIES Acute Management CASE PRESENTATIONS Case Study 22-1 Case Study 22-2 *Lieutenant Colonel (Retired), Medical Corps, US Air Force; Clinical Director, Department of Defense, Hearing Center of Excellence, Wilford Hall Ambulatory Surgical Center, 59th Medical Wing, Lackland Air Force Base, Texas 78236 †Captain, Medical Corps, US Air Force; Resident Otolaryngologist, San Antonio Military Medical Center, 3551 Roger Brooke Drive, Joint Base San Antonio, Fort Sam Houston, Texas 78234 267 Otolaryngology/Head and Neck Combat Casualty Care INTRODUCTION The conflicts in Iraq and Afghanistan have resulted age to the deeper structures of the middle and inner in large numbers of head and neck injuries to NATO ear, as well as the brain. Special arrangement of the (North Atlantic Treaty Organization) and Afghan ser- outer and middle ear is essential for efficient capture vice members. Improvised explosive devices, mortars, and transduction of sound energy to the inner ear in and suicide bombs are the weapons of choice during order for hearing to take place. This efficiency relies this conflict. The resultant injuries are high-velocity on a functional anatomical relationship of a taut tym- projectile injuries. Relatively little is known about the panic membrane connected to a mobile, intact ossicular precise incidence and prevalence of isolated closed chain. Traumatic forces that disrupt this relationship temporal bone fractures in theater. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

CASE REPORT Osteopathic Manipulative Treatment to Resolve
CASE REPORT Osteopathic Manipulative Treatment to Resolve Head and Neck Pain After Tooth Extraction Patricia M. Meyer, DO, MS Sharon M. Gustowski, DO, MPH Pain is a common occurrence after tooth extraction and fter dental extraction, the majority of patients have is usually localized to the extraction site. However, clinical Apain lasting less than 1 week that can be controlled experience shows that patients may also have pain in by analgesics. The length, type, and severity of pain vary the head or neck in the weeks after this procedure. The as a result of multiple factors, such as the difficulty of the authors present a case representative of these findings. extraction procedure, the patient’s health status and atti - In the case, cranial and cervical somatic dysfunction in tude, and the patient’s sex. 1 Other pain syndromes that a patient who had undergone tooth extraction was may occur weeks after the procedure—though rare— resolved through the use of osteopathic manipulative include neuropathic pain, temporomandibular disorder, 2,3 treatment. This case emphasizes the need to include a cluster headache, 4,5 and neck and head pain caused by dental history when evaluating head and neck pain as somatic dysfunction. 6,7 Prolonged and nonresolving pain part of comprehensive osteopathic medical care. The should be investigated for such conditions as rheumatologic case can also serve as a foundation for a detailed discus - diseases, tumors, migraine headache, or myofascial pain sion regarding how to effectively incorporate osteopathic syndrome. manipulative treatment into primary care practice for The etiologic characteristics of head and neck pain patients who present with head or neck pain after tooth after dental procedures are multifactorial, depending on extraction. -
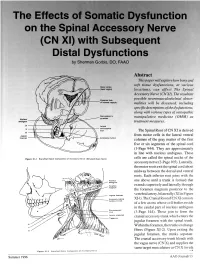
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO
The Effects of Somatic Dysfunction on the Spinal Accessory Nerve (CN XI) with Subsequent Distal Dysfunctions by Sherman Gorbis, DO, FAAO Abstract This paper will explore how bony and soft tissue dysfunctions, at various Motor codes (head region) locations, can affect The Spinal Accessory Nerve (CN XI). The resultant possible neuromusculoskeletal abnor- Posterior limb of internal capsule malities will be discussed, including specific descriptions of the dysfunctions, along with various types of osteopathic DBOUSSFigon In pyramids manipulative medicine (OMM) as Nucleus amblguus treatment measures. IX Lateral X corticospinal tract The Spinal Root of CN XI is derived XI Jugular from motor cells in the lateral ventral foramen Accessory nucleus columns of the gray matter of the first five or six segments of the spinal cord (1-Page 944). They are approximately in line with nucleus ambiguus. These Flgure XI-I Branchtal Motot Component of Accessory Nerve (Elevated Brain Sterol cells are called the spinal nuclei of the accessory nerve (2-Page 105). Laterally, the motor roots exit the spinal cord about midway between the dorsal and ventral roots. Each inferior root joins with the one above until a trunk is formed that extends superiorly and laterally through the foramen magnum posterior to the Jugular lor•men vertebral artery, bilaterally (XI in Figure Accessory (spinal XI-1). The Cranial Root of CN XI consists nucleus CI-CS of a few axons whose cell bodies reside in the caudal part of nucleus ambiguus Sternomesiod (cull (3-Page 144). These join to form the Lent or scapulae cranial accessory trunk which enters the Trap-axles jugular foramen with the spinal trunk. -

Frontal Lobe Anterior Corpora Commissure Quadrigemina Superior Colliculus Optic Chiasm Inferior Colliculus
Chapter 16 The Nervous System The Brain and Cranial Nerves Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc. Introduction • The brain is a complex three-dimensional structure that performs a bewildering array of functions • Think of the brain as an organic computer • However, the brain is far more versatile than a computer • The brain is far more complex than the spinal cord • The brain consists of roughly 20 billion neurons © 2015 Pearson Education, Inc. An Introduction to the Organization of the Brain • Embryology of the Brain • The CNS begins as a neural tube • The lumen of the tube (neurocoel) is filled with fluid • The lumen of the tube will expand thus forming the various ventricles of the brain • In the fourth week of development, the cephalic area of the neural tube enlarges to form: • Prosencephalon • Mesencephalon • Rhombencephalon © 2015 Pearson Education, Inc. Table 16.1 Development of the Human Brain © 2015 Pearson Education, Inc. An Introduction to the Organization of the Brain • Embryology of the Brain (continued) • Prosencephalon eventually develops to form: • Telencephalon forms: • Cerebrum • Diencephalon forms: • Epithalamus, thalamus, and hypothalamus. © 2015 Pearson Education, Inc. Table 16.1 Development of the Human Brain © 2015 Pearson Education, Inc. An Introduction to the Organization of the Brain • Embryology of the Brain (continued) • Mesencephalon • Does not subdivide • Becomes the midbrain © 2015 Pearson Education, Inc. Table 16.1 Development of the Human Brain © 2015 Pearson Education, Inc. An Introduction to the Organization of the Brain • Embryology of the Brain (continued) • Rhombencephalon • Eventually develops to form: • Metencephalon: forms the pons and cerebellum • Myelencephalon: forms the medulla oblongata © 2015 Pearson Education, Inc. -
Prezentace Aplikace Powerpoint
MENINGES AND CEREBROSPINAL FLUID Konstantinos Choulakis Konstantinos Choulakis Meninges • Dura Mater • Aracnoid Mater • Pia Mater Dura Mater Spinal Dura mater Cranial Dura mater It forms a tube (saccus durrae matris spinalis) which start It is firmly attached to the periostium of the skull from which it receives from foramen magnus and extends to second segment of small blood vessels, branches of meningeal vessels (inappropriate name) the sacrum. It is pierced by spinal nerve roots. The spinal which occur in periostium. canal wall is coverd by periostium, then there is dura mater. The cranial dura mater has several features of importance especially, Between dura mater and periostium there is a , so called especially the dural reflections (derivatives) and the dural venous epidural space, which is filled with adipose tissue and a sinuses(see blood supply) venous plexus , the plexus venosi vertebrales interni Dura mater is attached to avascular arachnoid mater. Between them there is a potential space, so called subdural space which contains a small amount of interstitial fluid. Enables arachnoid mater to slide against dura mater. Dural Reflections The dura separates into two layers at dural reflections (also known as dural folds), places where the inner dural layer is reflected as sheet-like protrusions into the cranial cavity. There are two main dural reflections: • The tentorium cerebelli exists between and separates the cerebellum and • The falx cerebri, which separates the two hemispheres of the brain, is located in the brainstem from the occipital lobes of the cerebrum. The peripheral border of longitudinal cerebral fissure between the hemispheres. Its free edge is close to corpus tentorium is attached to the upper edges of the petrous bones and to the calosum. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -
Skull, Brain and Cranial Nerves
Skull, Brain and Cranial Nerves Head and Neck Continued Skull Part of Axial Skeleton Cranial bones = cranium Enclose and protect brain Attachment for head + neck muscles pg 149 Facial bones =framework of face Form cavities for sense organs Opening for air + food passage Hold teeth Anchor face muscles Bones of Skull Flat bones: thin, flattened, some curve Sutures: immovable joints joining bones Calvaria = Skullcap =Vault Superior, Lateral, Posterior part of skull Floor = Base Inferior part of skull 85 openings in skull Spinal cord, blood vessels, nerves Cranial Fossae Created by bony ridges Supports, encircles brain 3 Fossae Anterior Middle Posterior Other small cavities in skull Middle Ear, Inner Ear Nasal Orbit pg 153 Skull through Life Ossifies late in 2nd month of development Frontal + Mandible start as 2 halves-then fuse Skull bones separated by unossified membranes = Fontanels Allow compression of skull during delivery Mostly replaced w/bone after 1st year Growth of Skull ½ adult size by age 9 months ¾ adult size by 2 years 100% adult size by 8-9 years Face enlarges between ages 6-13 years The Brain 4 Parts Cerebrum Diencephalon Brain Stem Pons Medulla Midbrain Cerebellum Gray matter surrounded by White matter pg 348 Meninges: 3 membranes around brain and spinal cord Made of Connective tissue Functions Cover, Protect CNS Enclose, protect blood vessels supplying CNS Contain CSF 3 Layers Dura Mater (external) Arachnoid Mater (middle) pg 375 Pia Mater (internal) Meninges (continued) Dura mater Strongest, -

Duplication of Falx Cerebelli, Occipital Sinus, and Internal Occipital Crest
Romanian Journal of Morphology and Embryology 2009, 50(1):107–110 ORIGINAL PAPER Duplication of falx cerebelli, occipital sinus, and internal occipital crest SUJATHA D’COSTA, A. KRISHNAMURTHY, S. R. NAYAK, SAMPATH MADHYASTA, LATHA V. PRABHU, JIJI P. J, ANU V. RANADE, MANGALA M. PAI, RAJANIGANDHA VADGAONKAR, C. GANESH KUMAR, RAJALAKSHMI RAI Department of Anatomy, Centre for Basic Sciences, Kasturba Medical College, Bejai, Mangalore, Karnataka, India Abstract The incidence of variations of falx cerebelli was studied in 52 adult cadavers of south Indian origin, at Kasturba Medical College Mangalore, after removal of calvaria. In eight (15.4%) cases, we observed duplicated falx cerebelli along with duplicated occipital sinus and internal occipital crest. The length and the distance between each of the falces were measured. The mean length of the right falces cerebelli was 38 mm and the left was 41 mm. The mean distance between these two falces was 20 mm. No marginal sinus was detected. Each of the falces cerebelli had distinct base and apex and possessed a distinct occipital venous sinus on each attached border. These sinuses were noted to drain into the left and right transverse sinus respectively. After detaching the dura mater from inner bony surface of the occipital bone, it was noted that there were two distinct internal occipital crests arising and diverging inferiorly near the posterolateral borders of foramen magnum. The brain from these cadavers appeared grossly normal with no defect of the vermis. Neurosurgeons and neuroradiologists should be aware of such variations, as these could be potential sources of hemorrhage during suboccipital approaches or may lead to erroneous interpretations of imaging of the posterior cranial fossa. -

The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1
Open Access Review Article DOI: 10.7759/cureus.8697 The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1 Bruno Bordoni 1 1. Physical Medicine and Rehabilitation, Foundation Don Carlo Gnocchi, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract In osteopathic manual medicine (OMM), there are several approaches for patient assessment and treatment. One of these is the five diaphragm model (tentorium cerebelli, tongue, thoracic outlet, diaphragm, and pelvic floor), whose foundations are part of another historical model: respiratory-circulatory. The myofascial continuity, anterior and posterior, supports the notion the human body cannot be divided into segments but is a continuum of matter, fluids, and emotions. In this first part, the neurological relationships of the tentorium cerebelli and the lingual muscle complex will be highlighted, underlining the complex interactions and anastomoses, through the most current scientific data and an accurate review of the topic. In the second part, I will describe the neurological relationships of the thoracic outlet, the respiratory diaphragm and the pelvic floor, with clinical reflections. In literature, to my knowledge, it is the first time that the different neurological relationships of these anatomical segments have been discussed, highlighting the constant neurological continuity of the five diaphragms. Categories: Medical Education, Anatomy, Osteopathic Medicine Keywords: diaphragm, osteopathic, fascia, myofascial, fascintegrity,