Epidemiological Update Measles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Roraima State Site Profiling. Boa Vista and Pacaraima, Roraima State
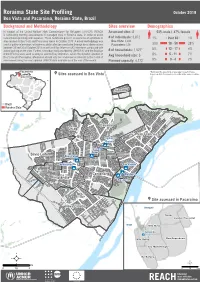
Roraima State Site Profiling October 2018 Boa Vista and Pacaraima, Roraima State, Brazil Background and Methodology Sites overview Demographics In support of the United Nations High Commissioner for Refugees (UNHCR), REACH Assessed sites: 8 53% male / 47% female 1+28+4+7+7 is conducting monthly assessments in managed sites in Roraima state, in order to assist 1+30+5+8+9 humanitarian planning and response. These factsheets present an overview of conditions in # of individuals: 3,872 1% 0ver 60 1% sites located in Boa Vista and Pacaraima towns in October 2018. A mixed methodology was Boa Vista: 3,444 used to gather information, with primary data collection conducted through direct observations Pacaraima: 428 30% 18 - 59 28% between 29 and 30 of October 2018 as well as 8 Key Informant (KI) interviews conducted with 5% 12 - 17 4% actors working on the sites. Further, secondary data provided by UNHCR KI and the Brazilian # of households: 1,527* Armed Forces were used to analyse selected key indicators. Given the dynamic situation in Avg household size: 3 8% 5 - 11 7% Boa Vista and Pacaraima, information should only be considered as relevant to the month of assessment using the most updated UNHCR data available as of the end of the month. Planned capacity: 4,172 9% 0 - 4 7% !(Pacaraima *Estimated by assuming an average household size, !( ¥Sites assessed in Boa Vista based on data from previous rounds in the same location. Boa Vista Cauamé Brazil Roraima State Cauamé União São Francisco Jardim Floresta ÔÆ Tancredo Neves Silvio Leite Nova Canaã ÔÆ ÔÆ Pintolândia São Vicente ÔÆ ÔÆ ÔÆ Centenário ÔÆ Rondon 1 Pintolândia Rondon 3 ¥Site assessed in Pacaraima Nova Cidade Venezuela Suapi Jardim Florestal Brazil Vila Nova Janokoida ÔÆ Das Orquídeas Vila Velha Ilzo Montenegro Da Balança ² ² km m 0 1,5 3 0 500 1.000 Fundo de População das Nações Unidas União Europeia Roraima site profiling October 2018 Jardim Floresta Boa Vista, Roraima State, Brazil Lat. -

Exploratory Temporal and Spatial Distribution Analysis of Dengue Notifications in Boa Vista, Roraima, Brazilian Amazon, 1999-2001†
Exploratory Temporal and Spatial Distribution Analysis of Dengue Notifications in Boa Vista, Roraima, Brazilian Amazon, 1999-2001† by Maria Goreti Rosa-Freitas*, Pantelis Tsouris**#, Alexander Sibajev***, Ellem Tatiani de Souza Weimann**, Alexandre Ubirajara Marques**, Rodrigo Lopes Ferreira** and José Francisco Luitgards-Moura*** *Laboratório de Transmissores de Hematozoários, Departamento de Entomologia, Instituto Oswaldo Cruz, Av. Brasil 4365, Manguinhos, 21045-900 Rio de Janeiro, RJ, Brasil **Núcleo Avançado de Vetores – Convênio FIOCRUZ-UFRR BR 174 S/N - Boa Vista, RR, Brasil ***Centro de Ciências Biológicas e da Saúde, UFRR, BR 174 S/N - Boa Vista, RR, Brasil Abstract In Brazil, as in the rest of the world, dengue has become the most important arthropod-borne viral disease of public health significance. Roraima state presented the highest dengue incidence coefficient in Brazil in the last few years (224.9 and 164.2 per 10,000 inhabitants in 2000 and 2001, respectively). The capital, Boa Vista, reports the highest number of dengue cases in Roraima. This study examined the temporal and spatial distribution of dengue in Boa Vista during the years 1999- 2001, based on daily notifications as recorded by local health authorities. Temporally, dengue notifications were analysed by weekly and monthly averages and age distribution and correlated to meteorological variables. Spatially, dengue coefficients, premises infestation indices, population density and income levels were allocated in a geographical information system using, Boa Vista 49 neighbourhoods as units. Dengue outbreaks displayed distinct year-to-year distribution patterns that were neither periodical nor significantly correlated to any meteorological variable. There were no preferences for age and sex. -

Um Estudo Sobre Amapá E Roraima
ISSN 1415-4765 TEXTO PARA DISCUSSÃO NO 683 Federalismo, Repasses Federais e Crescimento Econômico: um Estudo sobre Amapá e Roraima Bruno de Oliveira Cruz Carlos Wagner de Albuquerque Oliveira Brasília, novembro de 1999 ISSN 1415-4765 TEXTO PARA DISCUSSÃO NO 683 Federalismo, Repasses Federais e Crescimento Econômico: um Estudo sobre Amapá e Roraima* Bruno de Oliveira Cruz** Carlos Wagner de Albuquerque Oliveira** Brasília, novembro de 1999 * Os autores agradecem a Mônica Mora, Antônio Carlos Galvão, Herton Araújo, Nelson Zackseski, Maria Cris- tina Macdowell, Luciana Mendes, Salvador Viana e Humberto Watson pelos comentários, sugestões e auxílio para o término desta pesquisa. ** Pesquisadores da Diretoria de Políticas Regionais e Urbanas do IPEA. MINISTÉRIO DO PLANEJAMENTO, ORÇAMENTO E GESTÃO Martus Tavares – Ministro Guilherme Dias – Secretário Executivo Instituto de Pesquisa Econômica Aplicada Presidente Roberto Borges Martins DIRETORIA Eustáquio J. Reis Gustavo Maia Gomes Hubimaier Cantuária Santiago Luís Fernando Tironi Murilo Lôbo Ricardo Paes de Barros Fundação pública vinculada ao Ministério do Planejamento, Orçamento e Gestão, o IPEA fornece suporte técnico e institucional às ações governamentais e torna disponíves, para a sociedade, elementos necessários ao conhecimento e à solução dos problemas econômicos e sociais do país. Inúmeras políticas públicas e programas de desenvolvimento brasileiro são formulados a partir dos estudos e pesquisas realizados pelas equipes de especialistas do IPEA. TEXTO PARA DISCUSSÃO tem o objetivo de divulgar resultados de estudos desenvolvidos direta ou indiretamente pelo IPEA, bem como trabalhos considerados de relevância para disseminação pelo Instituto, para informar profissionais especializados e colher sugestões. Tiragem: 115 exemplares COORDENAÇÃO DO EDITORIAL Brasília – DF: SBS Q. 1, Bl. -
Chapter 3 the North- Lost in the Amazon
BRAZIL Chapter 3 The North- Lost in the Amazon Have you ever heard about Amazon rainforest? Let us learn together! The equatorial North, also known as the Amazon or Amazônia, is Brazil's largest region with total landmass of 3,869,638 square kilometers, covering 45.3 percent of the national territory. Way too big and enormous!! It is also the least inhabited part of the country. 31 BRAZIL The region has the largest rainforest of the world and is called Amazon. The word Amazon refers to the women warriors who once fought in inter-tribe in ancient times in this region of today's North Region of Brazil. It is also the name of one of the major river that passes through Brazil and flows eastward into South Atlantic. This river is also the largest of the world in terms of water carried in it. There are also numerous other rivers in the area. It is one fifth of all the earth's fresh water reserves. There are two main Amazonian cities: Manaus, capital of the State of Amazonas, and Belém, capital of the State of Pará. 32 BRAZIL Over half of the Amazon rainforest( more than 60 per cent) is located in Brazil but it is also located in other South American countries including Peru, Venezuela, Ecuador, Colombia, Guyana, Bolivia, Suriname and French Guiana. The Amazon is home to around two and a half million different insect species as well as over 40000 plant species. There are also a number of dangerous species living in the Amazon rainforest such as the “Onça Pintada” (Brazilian Puma) and anaconda. -

From Roraima, Brazil: Species Composition, Distribution, and New Records
14 1 21 ANNOTATED LIST OF SPECIES Check List 14 (1): 21–35 https://doi.org/10.15560/14.1.21 Freshwater shrimps (Crustacea, Decapoda, Caridea, Dendrobranchiata) from Roraima, Brazil: species composition, distribution, and new records Maria Aparecida Laurindo dos Santos,1 Patrícia Macedo de Castro,2, 3 Célio Magalhães4 1 Instituto Nacional de Pesquisas da Amazônia, Programa de Pós-Graduação em Biologia de Água Doce e Pesca Interior. Av. André Araújo, 2936 - Petrópolis, 69067-375 Manaus, Amazonas, Brazil. 2 Universidade Estadual de Roraima, Pró-Reitoria de Pesquisa e Pós-Graduação. Rua Sete de Setembro, 231 - Canarinho, 69306-530, Boa Vista, RR, Brazil. 3 Museu Integrado de Roraima/IACTI-RR. Av. Brigadeiro Eduardo Gomes, 2868 – Pq. Anauá, 69305-010, Boa Vista, RR, Brazil. 4 Instituto Nacional de Pesquisas da Amazônia, Coordenação de Biodiversidade. Av. André Araújo, 2936 - Petrópolis, 69067-375, Manaus, AM, Brazil Corresponding author: Célio Magalhães, [email protected] Abstract This work provides an update on the species composition and distribution of freshwater shrimps from the state of Roraima, Brazil, based on material deposited in the Brazilian collections of the Instituto Nacional de Pesquisas da Amazônia (Manaus) and the Museu Integrado de Roraima (Boa Vista). A total of 12 species (1 Sergestidae, 3 Eury- rhynchidae, and 8 Palaemonidae) are listed, of which 7 (Acetes paraguayensis Hansen, 1919; Euryrhynchus ama- zoniensis Tiefenbacher, 1978; E. burchelli Calman, 1907; E. wrzesniowskii Miers, 1877; Palaemon yuna Carvalho, Magalhães & Mantelatto, 2014; Pseudopalaemon chryseus Kensley & Walker, 1982; and Ps. gouldingi Kensley & Walker, 1982) are recorded for the first time from the state of Roraima. -

Indigenous Protagonism in Roraima and Environment Guardianship Inside the São Marcos Indigenous Land
http://dx.doi.org/10.18623/rvd.v13i26.671 INDIGENOUS PROTAGONISM IN RORAIMA AND ENVIRONMENT GUARDIANSHIP INSIDE THE SÃO MARCOS INDIGENOUS LAND Serguei Aily Franco de Camargo Doctor of Aquaculture at the São Paulo State University of Júlio de Mesquita Filho (UNESP). Master of Resource Conservation and Management at the São Paulo State University of Júlio de Mesquita Filho (UNESP). Law Professor at Estácio Atual Faculty (Boa Vista, RR). Professor at the Post Graduation Program in Fishing Sciences in the Tropics at the Federal University of Amazonas. Email: [email protected] Edson Damas da Silveira Doctor of Economic and Social-environmental Law at the Pontifical Catholic University of Paraná (PUCPR). Master of Anthropology at the Federal University of Pernambuco (UFPE) and of Economic and Social Law at the Pontifical Catholic University of Paraná (PUCPR). Law Professor at Estácio Atual Faculty in the Amazon. Professor of Indigenous Law in the Law Course at Cathedral Faculty in Boa Vista. Public Prosecutor at the Public Prosecution Office of the State of Roraima. Email: [email protected] ABSTRACT This paper presents a case study about an environmental lawsuit proposed by an indigenous citizen and signed by an indigenous lawyer aiming at preserving the environment inside the Indigenous Land of São Marcos, near Pacaraima city seat, at the border of the Indigenous Community of Ouro Preto. The case is about the irregular disposal of solid waste by the city seat inside the indigenous land and within the limits of the community where the tuxaua author of lawsuit lives. The objective of the paper is to check whether the judicialization of this environmental claim resulted in the maturation of the indigenous movement pointed out by the exercise of the full protagonism in solving problems arising from the relationship with the Brazilian State. -

FOOD ASSISTANCE FACT SHEET BRAZIL Updated April 20, 2020
FOOD ASSISTANCE FACT SHEET BRAZIL Updated April 20, 2020 The ongoing political and economic crisis in Venezuela has driven more than five million Venezuelans to flee the country since 2014, including approximately 250,000 Venezuelans who are sheltering in Brazil. SITUATION • Deteriorating political and economic conditions in Venezuela— characterized by extreme hyperinflation and a severe lack of financial means to access food and medicine—have contributed to increasing humanitarian needs, triggering an influx of Venezuelans into Brazil, as well as other countries in the region. • As of November 2019, more than 250,000 Venezuelans—many of whom remain in need of food assistance—were sheltering in Brazil, according to the Regional Interagency Coordination Platform for Refugees and Migrants from Venezuela (R4V). The population influx is straining the capacity of the Government of Brazil (GoB) to provide services in areas of the country bordering Venezuela, particularly in Roraima and Amazonas states. • In 2018, the GoB established a voluntary relocation program for Venezuelans intending to remain in Brazil. The GoB—with support from relief actors—facilitates the voluntary resettlement of Venezuelans from Amazonas and Roraima to other areas across Brazil FOOD FOR PEACE CONTRIBUTIONS to reduce the impact of population flows on the border regions and TOTAL CONTRIBUTIONS PER FISCAL YEAR (FY) provide better socioeconomic opportunities for refugees and migrants. U.S. DOLLARS METRIC TONS* FY 2019 $5.8 million — FY 2018 $2.0 million — FY 2017 — — *Metric tonnage does not reflect funding for vouchers or cash transfers RESPONSE USAID’s Office of Food for Peace (FFP) partners with the Adventist Food Vouchers 85% Development and Relief Agency (ADRA) to provide food vouchers and locally procured food aid to approximately 21,450 vulnerable Venezuelans and host community members sheltering in Amaz onas, Local, Regional, and International Bahia, Minas Gerais, Paraná, Rio Grande do Sul, and Roraima states. -

Redalyc.A List of Psocoptera (Insecta: Psocodea) from Brazil
Revista Mexicana de Biodiversidad ISSN: 1870-3453 [email protected] Universidad Nacional Autónoma de México México García Aldrete, Alfonso N.; Mockford, Edward L. A list of Psocoptera (Insecta: Psocodea) from Brazil Revista Mexicana de Biodiversidad, vol. 80, núm. 3, 2009, pp. 665-673 Universidad Nacional Autónoma de México Distrito Federal, México Available in: http://www.redalyc.org/articulo.oa?id=42515996009 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Revista Mexicana de Biodiversidad 80: 665- 673, 2009 A list of Psocoptera (Insecta: Psocodea) from Brazil Listado de Psocoptera (Insecta: Psocodea) de Brasil Alfonso N. García Aldrete1* and Edward L. Mockford 2 1Instituto de Biología, Universidad Nacional Autónoma de México, Apartado postal 70-153, 04510 México, D. F., Mexico. 2Department of Biological Sciences, Illinois State University, Campus Box 4120, Normal, Illinois 61790-4120, USA. *Correspondent: [email protected] Abstract. The species of Psocoptera currently known for Brazil are listed, with state distribution and biogeographic status. The categories of geographic distribution are discussed, as well as some of the evidence indicating that the present size of the Brazilian fauna is underestimated. Key words: Psocodea, Psocoptera, Brazil, geographic distribution. Resumen. Se listan las especies de Psocoptera actualmente registradas en Brasil, incluyendo la distribución por estado y su categoría biogeográfi ca. Se presenta alguna de la evidencia que hace suponer que el tamaño actual de la fauna de Psocoptera de Brasil está subestimada. -

Goiás Pode Ser Dividido. Roraima E Amapá, Promovidos
Goiás pode ser dividido. WBs Roraima e Amapá, promovidos. /6- th%$ A Comissão de Sistematizarão da Cons lhida pelo executivo federal, sendo que o Ficou prejudicada emenda de autoria tituinte aprovou ontem a criação de mais presidente da República deve também no do deputado Paulo Roberto (PMDB-PA), três Estados no País. Por 82. votos contra mear, até 30 dias após o resultado favorável que criava o Estado do Tapajós, unificando cinco e com cinco abstenções, aprovou do plebiscito, o governador pro témpore pa onze municípios do Pará. Seu autor susten emenda dos deputados goianos Siqueira ra um mandato "tampão" que vai coincidir tou que não haveria prejuízos para a União, Campos (PDC) e José Freire (PMDB), crian com o final do mandato dos governadores pois a região já tem infra-estrutura, mas o do o Estado de Tocantins, a ser desmembra estaduais em 1990. A Assembléia Consti senador Aluísio Chaves (PFL-PA) discursou do de Goiás; e por 90 votos contra apenas tuinte Estadual — com oito deputados fede contra a.iniciativa, argumentando que a re dois aprovou a emenda do deputado Moza- rais e três senadores — será eleita a 15 de gião não tem condições de se manter econo rildo Cavalcanti (PFL-RR) transformando novembro de 1968. Será esta Assembléia a micamente. Outra das emendas prejudica os territórios de Roraima e Amapá em Esta definir a capital definitiva. das é de autoria do deputado Chico Hum dos e estabelecendo que sua instalação se berto (PDT-MG) criando o Estado do Triân dará com a posse dos governadores, a serem A única emenda política apreciada on gulo, desmembrando o Triângulo Mineiro eleitos em 15 de novembro de 1990. -

The Economy of Roraima and the Venezuelan Flow: Evidence and Subsidies for Public Policies
THE ECONOMY OF RORAIMA AND THE VENEZUELAN FLOW: EVIDENCE AND SUBSIDIES FOR PUBLIC POLICIES The Brazilian state of Roraima is at the forefront of the country's efforts to manage the influx of Venezuelan refugees and migrants that started in 2013. Between 2013 and 2019, over 260,000 Venezuelans have applied for refugee or residency status in Brazil, with the vast majority entering through Roraima. The state is receiving help from federal authorities, UNHCR and civil society partners in managing its response to the influx and providing humanitarian assistance to the arrivals. A major initiative, the Interiorizacao voluntary relocation programme, has relocated more than 25,000 Venezuelans from Roraima to other Brazilian cities where there are more opportunities for social and economic integration. Driven by the need for data-backed analysis to inform interventions and the overall debate on the influx's impact on Roraima's society and economy, researchers – from Brazil's Department of Public Policy Analysis of Fundação Getulio Vargas (FGV DAPP), the International Migration Observatory (OBMigra) and the Federal University of Roraima (UFRR) – analysed official socioeconomic data and interviewed key actors managing the state's economy and its response to the inflow. They found that Roraima registered positive economic growth and diversification during the period of intense Venezuelan flow. Unemployment and poverty, on the other hand, rose during this time. This and other main findings and recommendations of their study are presented in this summary. DEMOGRAPHIC CHANGES The Venezuelan population in Roraima is mostly of Figure 1 of report. Population Pyramid of Roraima (2019) working age (15-64 years old), creating a visible change in Males Age range Females Roraima's population pyramid (Figure 1). -

Activities Targeting Indigenous Population
MAY/JUNE | 2021 REPORT INDIGENOUS POPULATION ACTIVITIES REPORT FOR THE INDIGENOUS POPULATION © ACNUR / FELIPE IRNALDO The May/June edition of The UN Refugee Agency (UNHCR) report on indigenous refugees and migrants in Brazil updates the registration data and population profile, in addition to the actions developed by UNHCR in these months. POPULATION PROFILE UPDATE REGISTRATION HISTORY 5900 5880 5799 5700 5512 5500 5300 5100 5020 5042 5055 5050 4981 4996 4900 May/2020 June/2020 July/2020 August/2020 September/2020 October/2020 February/2021 April/2021 June/2021 REGISTERED ON PROGRES: Indigenous peopleDISAGGREGATION registered in ProGres BY LEGAL STATUS 1% 1% 4% E’ÑEPA 49% 38% Other legal status KARIÑA Asylum seekers PEMON WARAO TOTAL: 27% WAYÚU 67% 100% 13% Refugees TOTAL: 100% 1 ACNUR | AGÊNCIA DA ONU PARA REFUGIADOS DISAGGREGATION BY SEX/AGE 00-04 05-11 12-17 18-24 25-49 50-59 60+ MALE 7% 10% 7% 7% 15% 2% 2% FEMALE 7% 9% 6% 7% 15% 3% 2% © ACNUR/FELIPE IRNALDO © ACNUR/FELIPE WORLD REFUGEE DAY: A NECESSARY LOOK AT INDIGENOUS PEOPLES With a historic record number of people being forced to abandon their homes globally, totaling more than 82.4 million people, World Refugee Day calls for a reduction in the conflicts that these flows of refugees may generate, as well as efforts to protect these groups in the midst of the COVID-19 pande- mic. For indigenous populations, the impacts of displacement are doubled, not only because of their relationship with the territory in which spiritual and survival practices are developed, but also because of the violation of human rights in their communities of origin, facing several additional challenges in the processes of seeking international protection. -

The Context of REDD+ in Brazil Drivers, Agents and Institutions
OCCASIONAL PAPER The context of REDD+ in Brazil Drivers, agents and institutions Second edition Peter H. May Brent Millikan Maria Fernanda Gebara OCCASIONAL PAPER 55 The context of REDD+ in Brazil Drivers, agents and institutions Second edition Peter H. May Brent Millikan Maria Fernanda Gebara Occasional Paper 55 © 2011 Center for International Forestry Research All rights reserved Printed in Indonesia ISBN 978-602-8693-28-8 May, P.H., Millikan, B. and Gebara, M.F. 2011 The context of REDD+ in Brazil: Drivers, agents and institutions. Occasional paper 55. 2nd edition. CIFOR, Bogor, Indonesia. Cover photo by Luke Perry CIFOR Jl. CIFOR, Situ Gede Bogor Barat 16115 Indonesia T +62 (251) 8622-622 F +62 (251) 8622-100 E [email protected] www.cifor.org Any views expressed in this paper are those of the authors. They do not necessarily represent the views of CIFOR, the authors’ institutions or the financial sponsors of this paper. Contents Abbreviations v Executive summary viii Resumo executivo x 1 Introduction 1 1.1. Current forest cover and historical overview of forest cover change 3 1.2. Review of the main drivers of forest cover change 7 1.3. Mitigation potential 16 2 Forests, land use trends and drivers of deforestation and degradation 3 2.1. Governance in the forest margins 19 2.2. Decentralisation and benefit sharing 25 2.3. Tenure issues 26 3 Institutional environment and distributional aspects 19 3.1. Political-economic context of drivers of deforestation and degradation 33 4 The political economy of deforestation and degradation 33 4.1. Broader climate change policy context 37 4.2.