M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Tip: Swollen Lymph "Glands" - When Should You Be Concerned?
Printer Friendly Version Page 1 of 3 Health Tip: Swollen lymph "glands" - When should you be concerned? Lymph nodes, sometimes referred to as lymph "glands", are part of the body's lymphatic system. The lymphatic system consists of a system of conduits and organized collections of lymphoid tissue that include nodes, the tonsils, and the spleen. Coursing through these channels is liquid called lymph that eventually drains into the bloodstream near the heart, but along the way, it is "filtered" by the lymph nodes. Within these lymph nodes are high concentrations of disease fighting cells, particularly lymphocytes. While performing their intended function of fighting infection, lymph nodes typically become enlarged. In fact, infection is most common reason for lymph nodes enlargement. Lymph nodes are found throughout the body, but when enlarged, are usually noticed in characteristic locations, particularly the neck, groin and armpit regions. Lymph node enlargement can be localized to one group of lymph nodes or can be generalized (involving several sites of lymph nodes). For example, enlarged lymph nodes localized to the arm pit could occur as a result of a bacterial infection in a hand wound. Generalized lymph node swelling, on the other hand, could be seen in a systemic illness such as viral mononucleosis. In addition to viral and bacterial infections, other causes for enlarged lymph nodes include immune disorders (lupus, rheumatoid arthritis, etc.), cancers affecting the lymphatic system (leukemia, lymphoma, Hodgkin's disease), and cancers that have spread (metastasized) from some other part of the body to the lymphatic system. The discovery of enlarged lymph nodes often causes concern because many people are aware that lymph node enlargement can be an early sign of cancer. -

Left Supraclavicular Lymphadenopathy As the Only Clinical Presentation of Prostate Cancer: a Case Report
ACTA MEDICA MARTINIANA 2017 17/2 DOI: 10.1515/acm-2017-0011 41 LEFT SUPRACLAVICULAR LYMPHADENOPATHY AS THE ONLY CLINICAL PRESENTATION OF PROSTATE CANCER: A CASE REPORT MOHANAD ABUSULTAN1, HANZEL P2, DURCANSKY D3, HAJTMAN A3. 1Department of Otorhinolaryngology, Prievidza Hospital, Slovak Republic 2Comenius University, Jessenius Faculty of Medicine and University Hospital in Martin, Clinic of Otorhinolaryngology, Head and Neck Surgery, Martin, Slovak Republic 3Department of Pathology, Prievidza Hospital, Slovak Republic A bstract Prostate cancer usually metastasis to the regional lymph nodes and can rarely metastases to nonregional supradi- aphragmatic lymph nodes. Cervical lymph node metastasis of prostate cancer is extremely rare. However, it should be considered in the differential diagnosis of cervical lymphadenopathy in male patients with adenocarcinoma of unknown primary site. In this report we present a rare case of metastatic prostate adenocarcinoma with left supra- clavicular lymphadenopathy as the only clinical presentation with no other evidence of metastasis to the regional lymph nodes or bone metastasis. Key words: Prostate cancer, Supraclavicular lymphadenopathy, Metastasis INTRODUCTION Most of cancer metastasis to the cervical lymph nodes is from cancers of the mucosal surfaces of the upper aerodigestive tract. The second most common source of metastasis is nonmucosal tumors in the head and neck such as salivary glands, thyroid glands and skin [1]. Cancers originating from sites other than the head and neck can rarely metastasize to the cervical lymph nodes. However, neoplasms of the genitourinary tract make up a sig- nificant proportion of these cancers and should be considered in the differential diagnosis of neoplastic lesions of the head and neck [2]. -

Axillary Lymph Nodes in Breast Cancer Patients: Sonographic Evaluation*
Pinheiro DJPCArtigo et al. / deLinfonodos Revisão axilares – avaliação ultrassonográfica Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica* Axillary lymph nodes in breast cancer patients: sonographic evaluation Denise Joffily Pereira da Costa Pinheiro1, Simone Elias2, Afonso Celso Pinto Nazário3 Pinheiro DJPC, Elias S, Nazário ACP. Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica. Radiol Bras. 2014 Jul/Ago; 47(4):240–244. Resumo O estadiamento axilar nas pacientes portadoras de câncer de mama inicial é fator essencial no planejamento terapêutico. Atualmente este é realizado durante o tratamento cirúrgico, mas há uma tendência em buscar técnicas pré-operatórias e de menor morbidade para avaliação dos linfonodos axilares. A ultrassonografia é um exame amplamente usado para esta finalidade e muitas vezes associado a punção aspirativa por agulha fina ou por agulha grossa. Entretanto, os critérios ultrassonográficos de suspeição para linfonodos axilares não apresentam valores preditivos significativos, gerando resultados discrepantes em estudos sobre sensibilidade e especificidade do método. O objetivo deste trabalho é realizar uma revisão na literatura médica sobre a ultrassonografia no estadiamento axilar e as principais alterações morfológicas do linfonodo metastático. Unitermos: Câncer de mama; Linfonodos axilares; Ultrassonografia; Aspectos morfológicos. Abstract Axillary staging of patients with early-stage breast cancer is essential in the treatment planning. Currently such staging is intraoperatively performed, but there is a tendency to seek a preoperative and less invasive technique to detect lymph node metastasis. Ultrasonography is widely utilized for this purpose, many times in association with fine-needle aspiration biopsy or core needle biopsy. However, the sonographic criteria for determining malignancy in axillary lymph nodes do not present significant predictive values, producing discrepant results in studies evaluating the sensitivity and specificity of this method. -
Impact of the Number of Dissected Axillary Lymph Nodes on Survival
ISSN: 2643-4563 Nabil et al. Int J Oncol Res 2019, 2:015 DOI: 10.23937/2643-4563/1710015 Volume 2 | Issue 1 International Journal of Open Access Oncology Research RESEARCH ARTICLE Impact of the Number of Dissected Axillary Lymph Nodes on Survival in Breast Cancer Patients Emad Eldin Nabil1, Ahmed M Maklad2,3, Ashraf Elyamany4,5*, Emad Gomaa6 and Moamen M Ali3,7 1Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 2Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 3King Fahad Medical City, Riyadh, KSA 4 Medical Oncology Department, SECI, Assiut University, Egypt Check for updates 5King Saud Medical City, Riyadh, KSA 6General Surgery Department, Sohag University Hospitals, Egypt 7Medical Physics, Radiation Oncology Department, SECI, Assiut University, Egypt *Corresponding author: Ashraf Elyamany, Medical Oncology Department, SECI, Assiut University, Egypt; King Saud Medical City, Riyadh, KSA Abstract regard median OS for patients having more than 10 LN excised was for N0, N1, N2, N3 5.57, 5.94, 4.97, 4.61 years Background: For patients with breast cancer, axillary dis- respectively while in the other group having less than 10 LN section was a standard treatment, especially with patient excised OS was 5.4, 5.14, 5.14 years respectively with P = with positive metastases in the sentinel nodes. For some 0.117. Regarding Lymphedema There was highly significant patients axillary dissection might be over-treatment, includ- difference between both arms p value 0.000, with higher ing those who have had a mastectomy. Especially with grades in arm I (moderate 17 cases and 6 cases severe the new trend of many radiation-therapy centers, provide edema). -

Microlymphatic Surgery for the Treatment of Iatrogenic Lymphedema
Microlymphatic Surgery for the Treatment of Iatrogenic Lymphedema Corinne Becker, MDa, Julie V. Vasile, MDb,*, Joshua L. Levine, MDb, Bernardo N. Batista, MDa, Rebecca M. Studinger, MDb, Constance M. Chen, MDb, Marc Riquet, MDc KEYWORDS Lymphedema Treatment Autologous lymph node transplantation (ALNT) Microsurgical vascularized lymph node transfer Iatrogenic Secondary Brachial plexus neuropathy Infection KEY POINTS Autologous lymph node transplant or microsurgical vascularized lymph node transfer (ALNT) is a surgical treatment option for lymphedema, which brings vascularized, VEGF-C producing tissue into the previously operated field to promote lymphangiogenesis and bridge the distal obstructed lymphatic system with the proximal lymphatic system. Additionally, lymph nodes with important immunologic function are brought into the fibrotic and damaged tissue. ALNT can cure lymphedema, reduce the risk of infection and cellulitis, and improve brachial plexus neuropathies. ALNT can also be combined with breast reconstruction flaps to be an elegant treatment for a breast cancer patient. OVERVIEW: NATURE OF THE PROBLEM Clinically, patients develop firm subcutaneous tissue, progressing to overgrowth and fibrosis. Lymphedema is a result of disruption to the Lymphedema is a common chronic and progres- lymphatic transport system, leading to accumula- sive condition that can occur after cancer treat- tion of protein-rich lymph fluid in the interstitial ment. The reported incidence of lymphedema space. The accumulation of edematous fluid mani- varies because of varying methods of assess- fests as soft and pitting edema seen in early ment,1–3 the long follow-up required for diagnosing lymphedema. Progression to nonpitting and irre- lymphedema, and the lack of patient education versible enlargement of the extremity is thought regarding lymphedema.4 In one 20-year follow-up to be the result of 2 mechanisms: of patients with breast cancer treated with mastec- 1. -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section -

ANATOMIC and PATHOLOGIC ASSESSMENT of FELINE LYMPH NODES USING COMPUTED TOMOGRAPHY and ULTRASONOGRAPHY Mauricio Tobón Restrepo
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en Doctorand: Mauricio Tobón Restrepo Directores: Yvonne Espada Gerlach & Rosa Novellas Torroja Tesi Doctoral Barcelona, 29 de juliol de 2016 This thesis has received financial support from the Colombian government through the “Francisco José de Caldas” scholarship program of COLCIENCIAS and from the Corporación Universitaria Lasallista. DEDICATED TO A los que son la razón y la misión de esta tesis… LOS GATOS. A mis padres y hermanos. A Ismael. Vor mijn poffertje. ACKNOWLEDGMENTS Tal vez es la parte que se pensaría más fácil de escribir, pero sin duda se juntan muchos sentimientos al momento de mirar atrás y ver todo lo que has aprendido y todas las personas que han estado a tu lado dándote una palabra de aliento… y es ahí cuando se asoma la lágrima… Sin duda alguna, comienzo agradeciendo a los propietarios de todos los gatos incluidos en este estudio, sin ellos esto no habría sido posible. A continuación agradezco a mis directoras de tesis, la Dra. Rosa Novellas y la Dra. Yvonne Espada. Muchas gracias por creer en mí, por apoyarme y por tenerme tanta paciencia. -

The Size of Lymph Nodes in the Neck on Sonograms As a Radiologic Criterion for Metastasis: How Reliable Is It?
AJNR Am J Neuroradiol 19:695–700, April 1998 The Size of Lymph Nodes in the Neck on Sonograms as a Radiologic Criterion for Metastasis: How Reliable Is It? Michiel W. M. van den Brekel, Jonas A. Castelijns, and Gordon B. Snow PURPOSE: A definition of cut-off points for nodal size is essential to determine whether cervical lymph nodes are metastatic or not. Because the currently used size criteria are defined for random populations of patients with head and neck cancer, we set out to study whether these criteria are optimal for patients without palpable metastases in different levels of the neck. We defined optimal size criteria for sonography by calculating the sensitivity and specificity of different size cut-off points. METHODS: We compared the sensitivity and specificity of different size cut-off points as measured on sonograms for various levels in the neck in a series of 117 patients with and 131 patients without palpable neck metastases. RESULTS: A minimum axial diameter of 7 mm for level II and 6 mm for the rest of the neck revealed the optimal compromise between sensitivity and specificity in necks without palpable metastases. For all necks together (with and without palpable metastases), the criteria were 1 to 2 mm larger. CONCLUSION: Our findings indicate that the current sonographic size criteria used for random patient populations are not optimal for necks without palpable metastases, nor can the same cut-off points be used for all levels in the neck. The management of lymph node metastases in the cious lymph nodes may convert both selective neck neck in patients with squamous cell carcinoma of the treatment and a wait-and-see policy to more secure upper air and food passages is a continuing source of comprehensive treatment of all levels of the neck (6). -
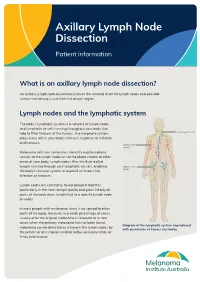
Axillary Lymph Node Dissection
Axillary Lymph Node Dissection Patient information What is an axillary lymph node dissection? An axillary lymph node dissection involves the removal of all the lymph nodes and possible tumour-containing tissue from the armpit region. Lymph nodes and the lymphatic system The body’s lymphatic system is a network of lymph nodes and lymphatic vessels running throughout your body that help to filter fluid out of the tissues. The lymphatic system plays a key role in your body’s immune response to infection and tumours. Melanoma cells can sometimes travel through lymphatic vessels to the lymph nodes or via the blood stream to other areas of your body. Lymph nodes filter the fluid (called lymph) running through your lymphatic vessels, enabling the body’s immune system to respond to threats like infection or tumours. Lymph nodes are commonly found grouped together, particularly in the neck, armpit (axilla) and groin. Nearly all parts of the body drain lymph fluid to a specific lymph node or nodes. In most people with melanoma, there is no spread to other parts of the body. However, in a small percentage of cases, usually after the original melanoma is removed or in rare cases when the primary melanoma has not been found, Diagram of the lymphatic system (reproduced melanoma can be detected as a lump in the lymph nodes by with permission of Cancer Australia). the patient or at a regular medical follow up examination or X-ray examination. In this situation, the standard treatment has been to remove all the lymph nodes in that area as often there is more than one lymph node involved. -

Lymphatic Drainage of the Breast: from Theory to Surgical Practice
Int. J. Morphol., 27(3):873-878, 2009. Lymphatic Drainage of the Breast: from Theory to Surgical Practice Drenaje Linfático de la Mama: desde la Teoría a la Práctica Quirúrgica *José Humberto Tavares Guerreiro Fregnani & **José Rafael Macéa FREGNANI, J. H. T. G. & MACÉA, J. R. Lymphatic drainage of the breast: from theory to surgical practice. Int. J. Morphol., 27(3):873-878, 2009. SUMMARY: Until recently, complete removal of axillary lymph nodes was performed as part of the treatment of breast cancer. Sentinel lymph node biopsy (SLNB) in selected cases has reduced the number of cases of wide axillary dissection and the related morbidity. Knowledge of breast lymphatic drainage is essential for understanding the principles behind SLNB and also for performing safe and correct axillary lymphonodectomy. This paper describes in detail the anatomical issues relating to breast lymphatic drainage and the correlated axillary and extra-axillary lymph nodes. In addition, it shows the application of this theoretical knowledge to surgical practice, especially with regard to SLNB and lymphonodectomy. The surgical nomenclature is compared with the current International Anatomical Terminology. KEY WORDS: Lymphatic drainage, Sentinel lymph node biopsy, Breast cancer. INTRODUCTION Breast cancer is the most frequent type of tumor changes to the sensitivity of the upper limb, posterior scapular among women, accounting for approximately one quarter dislocation (winged scapula syndrome), brachial plexus of all tumors in women. It has been estimated that more than lesions, axillary vessel thrombosis and lesions, skin necrosis one million new cases occur worldwide annually. Breast and pectoral muscle atrophy, among others (Torresan et al., cancer is responsible for significant morbidity and mortality 2002; Kim et al., 2006). -
201028 the Lymphatic System 2 – Structure and Function of The
Copyright EMAP Publishing 2020 This article is not for distribution except for journal club use Clinical Practice Keywords Immunity/Anatomy/Stem cell production/Lymphatic system Systems of life This article has been Lymphatic system double-blind peer reviewed In this article... l How blood and immune cells are produced and developed by the lymphatic system l Clinical significance of the primary and secondary lymphoid organs l How the lymphatic system mounts an immune response and filters pathogens The lymphatic system 2: structure and function of the lymphoid organs Key points Authors Yamni Nigam is professor in biomedical science; John Knight is associate The lymphoid professor in biomedical science; both at the College of Human and Health Sciences, organs include the Swansea University. red bone marrow, thymus, spleen Abstract This article is the second in a six-part series about the lymphatic system. It and clusters of discusses the role of the lymphoid organs, which is to develop and provide immunity lymph nodes for the body. The primary lymphoid organs are the red bone marrow, in which blood and immune cells are produced, and the thymus, where T-lymphocytes mature. The Blood and immune lymph nodes and spleen are the major secondary lymphoid organs; they filter out cells are produced pathogens and maintain the population of mature lymphocytes. inside the red bone marrow, during a Citation Nigam Y, Knight J (2020) The lymphatic system 2: structure and function of process called the lymphoid organs. Nursing Times [online]; 116: 11, 44-48. haematopoiesis The thymus secretes his article discusses the major become either erythrocytes, leucocytes or hormones that are lymphoid organs and their role platelets. -
Lymphatic System
LYMPHATIC SYSTEM Associated with the Blood and Cardiovascular System http://www.lymphnotes.com/article.php/id/151/ http://www.youtube.com/watch?v=qTXTDqvPnRk http://www.scribd.com/doc/60675255/Handouts- Lymphatic-System-F11 http://www.learningace.com/doc/5949560/9178 e2f0064b410c8c8e9218bcc748e6/ama-180- course-handouts Lymphatic System Lymph Fluid Lymph Vessels Lymph Nodes Four Organs Tonsils Spleen Thymus Gland Peyer’s Patches Functions Drain from tissue spaces, protein-containing fluid that escapes from the blood capillaries Transport fats from the digestive tract to the blood Produce lymphocytes Develop Immunities Interstitial Fluid Blood pressure forces some of the blood plasma through the single-celled capillary walls Interstitial Fluid is in the spaces between cells Most is reabsorbed into the capillaries Some fluid is not and must be drained from the tissue spaces to prevent swelling or Edema. Lymphatic Capillaries – drain this fluid Lymph is the fluid when it is in the vessels Fat Absorption Lacteals – lymphatic vessels in the villi of the small intestine that absorb fats and transport them to the blood. Looks milky because of the fat content and is called chyle. Lymphatic Vessels Lymph Capillaries Larger and more permeable than blood capillaries Closed at one end Occur singly or in extensive plexuses Lymphatic Capillaries Lymphatics Combined capillaries Larger Beaded appearance Similar to veins, but thinner walls and more valves One way valves to prevent backflow Lymph goes in one direction only