Thieme: Lymphedema Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section -

ANATOMIC and PATHOLOGIC ASSESSMENT of FELINE LYMPH NODES USING COMPUTED TOMOGRAPHY and ULTRASONOGRAPHY Mauricio Tobón Restrepo
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en Doctorand: Mauricio Tobón Restrepo Directores: Yvonne Espada Gerlach & Rosa Novellas Torroja Tesi Doctoral Barcelona, 29 de juliol de 2016 This thesis has received financial support from the Colombian government through the “Francisco José de Caldas” scholarship program of COLCIENCIAS and from the Corporación Universitaria Lasallista. DEDICATED TO A los que son la razón y la misión de esta tesis… LOS GATOS. A mis padres y hermanos. A Ismael. Vor mijn poffertje. ACKNOWLEDGMENTS Tal vez es la parte que se pensaría más fácil de escribir, pero sin duda se juntan muchos sentimientos al momento de mirar atrás y ver todo lo que has aprendido y todas las personas que han estado a tu lado dándote una palabra de aliento… y es ahí cuando se asoma la lágrima… Sin duda alguna, comienzo agradeciendo a los propietarios de todos los gatos incluidos en este estudio, sin ellos esto no habría sido posible. A continuación agradezco a mis directoras de tesis, la Dra. Rosa Novellas y la Dra. Yvonne Espada. Muchas gracias por creer en mí, por apoyarme y por tenerme tanta paciencia. -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -

Normal Gross and Histologic Features of the Gastrointestinal Tract
NORMAL GROSS AND HISTOLOGIC 1 FEATURES OF THE GASTROINTESTINAL TRACT THE NORMAL ESOPHAGUS left gastric, left phrenic, and left hepatic accessory arteries. Veins in the proximal and mid esopha- Anatomy gus drain into the systemic circulation, whereas Gross Anatomy. The adult esophagus is a the short gastric and left gastric veins of the muscular tube measuring approximately 25 cm portal system drain the distal esophagus. Linear and extending from the lower border of the cri- arrays of large caliber veins are unique to the distal coid cartilage to the gastroesophageal junction. esophagus and can be a helpful clue to the site of It lies posterior to the trachea and left atrium a biopsy when extensive cardiac-type mucosa is in the mediastinum but deviates slightly to the present near the gastroesophageal junction (4). left before descending to the diaphragm, where Lymphatic vessels are present in all layers of the it traverses the hiatus and enters the abdomen. esophagus. They drain to paratracheal and deep The subdiaphragmatic esophagus lies against cervical lymph nodes in the cervical esophagus, the posterior surface of the left hepatic lobe (1). bronchial and posterior mediastinal lymph nodes The International Classification of Diseases in the thoracic esophagus, and left gastric lymph and the American Joint Commission on Cancer nodes in the abdominal esophagus. divide the esophagus into upper, middle, and lower thirds, whereas endoscopists measure distance to points in the esophagus relative to the incisors (2). The esophagus begins 15 cm from the incisors and extends 40 cm from the incisors in the average adult (3). The upper and lower esophageal sphincters represent areas of increased resting tone but lack anatomic landmarks; they are located 15 to 18 cm from the incisors and slightly proximal to the gastroesophageal junction, respectively. -

Lymphatic System
WEGENER, W. (1972): Synopsis erblicher Depigmentierungsanomalien. Dtsch. Tierärztl. Wschr. 79, 64-68. — WESTENDORF, P. (1974): Der Haarwechsel der Haussaugetiere. Diss., Hannover: — Woop, J. C. (1968): Skin diseases of domestic animals. Vet. Record 82, 214-220. ZACHERL, M. K., & M. WEISER (1963): Ober den Mineralstoffgehalt von Rinderhaaren. Wien. Tier-arztl. Mschr. 50, 62-69. Lymphatic system Examination of the lymphatic system is important for many reasons. On the one hand, lymph nodes and lymph vessels can become affected, and show characteristic lesions, in various infectious diseases, such as actinobacillosis, tuberculosis, purulent infections and mycotic lymphadenitis, and particularly bovine leukosis. On the other hand, the lymphatic system participates in pathological processes within the drainage area of a particular part by means of reactive (or metastatic) swelling, tenderness or hardening; such changes provide information about affected organs which may be concealed and inaccessible for clinical examination. Finally, abnormal enlargement of a lymph node may affect the function of adjoining organs by pressure or by infiltration. In this connexion, when taking the case history the veterinary surgeon may put questions concerning -the prior occurrence of losses through disease of the "glands" (i.e. bovine leukosis), and the results of any official blood tests; also whether recently purchased cattle came from herds, officially free from leukosis or not. The general examination (p. 6S) may have already detected abnormal enlargement of one or more lymph nodes. Clinical examination o£ the lymphatic system takes the form if inspection and palpation of accessible lymph nodes, and if necessary the course of the lymphatics. If there is suspicion of leukosis, a blood sample must be taken for white cell count or for serological testing. -

Ministry of Education and Science of Ukraine Sumy State University 0
Ministry of Education and Science of Ukraine Sumy State University 0 Ministry of Education and Science of Ukraine Sumy State University SPLANCHNOLOGY, CARDIOVASCULAR AND IMMUNE SYSTEMS STUDY GUIDE Recommended by the Academic Council of Sumy State University Sumy Sumy State University 2016 1 УДК 611.1/.6+612.1+612.017.1](072) ББК 28.863.5я73 С72 Composite authors: V. I. Bumeister, Doctor of Biological Sciences, Professor; L. G. Sulim, Senior Lecturer; O. O. Prykhodko, Candidate of Medical Sciences, Assistant; O. S. Yarmolenko, Candidate of Medical Sciences, Assistant Reviewers: I. L. Kolisnyk – Associate Professor Ph. D., Kharkiv National Medical University; M. V. Pogorelov – Doctor of Medical Sciences, Sumy State University Recommended for publication by Academic Council of Sumy State University as а study guide (minutes № 5 of 10.11.2016) Splanchnology Cardiovascular and Immune Systems : study guide / С72 V. I. Bumeister, L. G. Sulim, O. O. Prykhodko, O. S. Yarmolenko. – Sumy : Sumy State University, 2016. – 253 p. This manual is intended for the students of medical higher educational institutions of IV accreditation level who study Human Anatomy in the English language. Посібник рекомендований для студентів вищих медичних навчальних закладів IV рівня акредитації, які вивчають анатомію людини англійською мовою. УДК 611.1/.6+612.1+612.017.1](072) ББК 28.863.5я73 © Bumeister V. I., Sulim L G., Prykhodko О. O., Yarmolenko O. S., 2016 © Sumy State University, 2016 2 Hippocratic Oath «Ὄμνυμι Ἀπόλλωνα ἰητρὸν, καὶ Ἀσκληπιὸν, καὶ Ὑγείαν, καὶ Πανάκειαν, καὶ θεοὺς πάντας τε καὶ πάσας, ἵστορας ποιεύμενος, ἐπιτελέα ποιήσειν κατὰ δύναμιν καὶ κρίσιν ἐμὴν ὅρκον τόνδε καὶ ξυγγραφὴν τήνδε. -
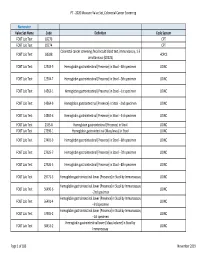
2020 Measure Value Set Colorectal Cancer Screening
PT ‐ 2020 Measure Value Set_Colorectal Cancer Screening Numerator Value Set Name Code Definition Code System FOBT Lab Test 82270 CPT FOBT Lab Test 82274 CPT Colorectal cancer screening; fecal occult blood test, immunoassay, 1‐3 FOBT Lab Test G0328 HCPCS simultaneous (G0328) FOBT Lab Test 12503‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐4th specimen LOINC FOBT Lab Test 12504‐7 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐5th specimen LOINC FOBT Lab Test 14563‐1 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐1st specimen LOINC FOBT Lab Test 14564‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐2nd specimen LOINC FOBT Lab Test 14565‐6 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐3rd specimen LOINC FOBT Lab Test 2335‐8 Hemoglobin.gastrointestinal [Presence] in Stool LOINC FOBT Lab Test 27396‐1 Hemoglobin.gastrointestinal [Mass/mass] in Stool LOINC FOBT Lab Test 27401‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐6th specimen LOINC FOBT Lab Test 27925‐7 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐7th specimen LOINC FOBT Lab Test 27926‐5 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐8th specimen LOINC FOBT Lab Test 29771‐3 Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay LOINC Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 56490‐6 LOINC ‐‐2nd specimen Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 56491‐4 LOINC ‐‐3rd specimen Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 57905‐2 -

Incidence, Morbidity and Mortality of Patients with Achalasia in England: Findings from a Nationwide Hospital Database and 4 Million Population Based Data
Incidence, morbidity and mortality of patients with achalasia in England: findings from a nationwide hospital database and 4 million population based data Appendix A: International Classification of Disease codes for Achalasia (HES) K22 – Achalasia of cardia Appendix B: Read codes (The Health Improvement Network) Appendix B1: Achalasia codes Clinical code Description J100.00 Achalasia of cardia Appendix B2: Clinical codes used to identify Hypertension, Diabetes and lipid lowering drugs Diabetes Clinical code Description C10..00 Diabetes mellitus C100.00 Diabetes mellitus with no mention of complication C100000 Diabetes mellitus, juvenile type, no mention of complication C100011 Insulin dependent diabetes mellitus C100100 Diabetes mellitus, adult onset, no mention of complication C100111 Maturity onset diabetes C100112 Non-insulin dependent diabetes mellitus C100z00 Diabetes mellitus NOS with no mention of complication C101.00 Diabetes mellitus with ketoacidosis C101000 Diabetes mellitus, juvenile type, with ketoacidosis C101100 Diabetes mellitus, adult onset, with ketoacidosis C101y00 Other specified diabetes mellitus with ketoacidosis C101z00 Diabetes mellitus NOS with ketoacidosis C102.00 Diabetes mellitus with hyperosmolar coma C102000 Diabetes mellitus, juvenile type, with hyperosmolar coma C102100 Diabetes mellitus, adult onset, with hyperosmolar coma C102z00 Diabetes mellitus NOS with hyperosmolar coma C103.00 Diabetes mellitus with ketoacidotic coma C103000 Diabetes mellitus, juvenile type, with ketoacidotic coma C103100 Diabetes -

Computed Tomographic Studies of Characteristics of Selected Canine Lymph Nodes Relevant to Staging and Treatment of Solid Tumours
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Saskatchewan's Research Archive Computed Tomographic Studies of Characteristics of Selected Canine Lymph Nodes Relevant to Staging and Treatment of Solid Tumours A Thesis Submitted to the College of Graduate and Postdoctoral Studies In Partial Fulfillment of the Requirements For the Degree of Master of Science In the Department of Small Animal Clinical Sciences University of Saskatchewan Saskatoon By Dr. Katherine Sweet, DVM © Copyright Katherine Sweet, June, 2017. All rights reserved. PERMISSION TO USE In presenting this thesis/dissertation in partial fulfillment of the requirements for a Postgraduate degree from the University of Saskatchewan, I agree that the Libraries of this University may make it freely available for inspection. I further agree that permission for copying of this thesis/dissertation in any manner, in whole or in part, for scholarly purposes may be granted by the professor or professors who supervised my thesis/dissertation work or, in their absence, by the Head of the Department or the Dean of the College in which my thesis work was done. It is understood that any copying or publication or use of this thesis/dissertation or parts thereof for financial gain shall not be allowed without my written permission. It is also understood that due recognition shall be given to me and to the University of Saskatchewan in any scholarly use which may be made of any material in my thesis/dissertation. Requests for permission -

18.1 Acute Postoperative Complications M
18 Postoperative Complications 18.1 Acute Postoperative Complications M. Seitz, B. Schlenker, Ch. Stief 18.1.1 Postoperative Bleeding 364 18.1.5 Abdominal Wound Dehiscence 403 18.1.1.1 Overview 364 18.1.5.1 Synonyms 403 18.1.1.2 Incidence and Risk Factors 365 18.1.5.2 Overview and Incidence 403 18.1.1.3 Detection and Clinical Signs 365 18.1.5.3 Risk Factors 404 18.1.1.4 Workup 366 18.1.5.4 Clinical Signs and Complications 404 18.1.1.5 Management 366 18.1.5.5 Prevention 405 18.1.1.6 Special Conditions 371 18.1.5.6 Management 405 18.1.2 Chest Pain and Dyspnea 373 18.1.6 Chylous Ascites 410 18.1.2.1 Overview 373 18.1.6.1 Overview 410 18.1.2.2 Cardiovascular System Disorders 373 18.1.6.2 Risk Factors and Pathogenesis 410 18.1.2.3 Postoperative Pulmonary Complications 373 18.1.6.3 Prevention 412 Pulmonary Embolism 373 18.1.6.4 Detection and Workup 413 Pleural Effusions 375 18.1.6.5 Management 413 Atelectasis 376 Infection/Pneumonia 376 18.1.7 Deep Venous Thrombosis 414 Tube Thoracostomy 376 18.1.7.1 Overview and Incidence 414 18.1.3 Acute Abdomen 377 18.1.7.2 Risk Factors 414 18.1.3.1 Initial Management 377 18.1.7.3 Detection and Clinical Findings 415 18.1.4 18.1.7.4 Management 415 Postoperative Fever 378 Unfractionated Heparin 415 18.1.4.1 Overview 378 Low-Molecular-Weight Heparin 415 18.1.4.2 Incidence 379 Long-Term Therapy 416 18.1.4.3 Definition 379 18.1.4.4 Risk Factors and Prevention 379 18.1.8 Lymphoceles 416 18.1.4.5 Detection and Work-Up 382 18.1.8.1 Anatomy and Physiology 416 Pulmonary 382 18.1.8.2 Overview 419 Urinary Tract 382 -

Magnetic Resonance Imaging and Endorectal Ultrasound for Diagnosis
Burdan et al. European Journal of Medical Research (2015) 20:4 DOI 10.1186/s40001-014-0078-0 EUROPEAN JOURNAL OF MEDICAL RESEARCH REVIEW Open Access Magnetic resonance imaging and endorectal ultrasound for diagnosis of rectal lesions Franciszek Burdan1,2*, Iwona Sudol-Szopinska3,4, Elzbieta Staroslawska1, Malgorzata Kolodziejczak5, Robert Klepacz6, Agnieszka Mocarska1, Marek Caban1, Iwonna Zelazowska-Cieslinska1 and Justyna Szumilo6 Abstract Endorectal ultrasonography (ERUS) and magnetic resonance imaging (MRI) allow exploring the morphology of the rectum in detail. Use of such data, especially assessment of the rectal wall, is an important tool for ascertaining the perianal fistula localization as well as stage of the cancer and planning it appropriate treatment, as stage T3 tumors are usually treated with neoadjuvant therapy, whereas T2 tumors are initially managed surgically. The only advantage of ERUS over MRI is the possibility of assessing T1 tumors that could be treated by transanal endoscopic microsurgery. However, MRI is better for visualizing most radiological prognostic features in rectal or anal cancer such as a circumferential resection margin less than 1 mm, T stage at T1-T2 or T3 tumors with extramural extension less than 5 mm, absence of extramural vascular invasion, N stage at N0/N1, and tumors located in the middle or upper third of the rectum. It can also evaluate the intersphincteric space or levator ani muscle involvement. Increased signal on diffusion weighted imaging (DWI) and low apparent diffusion coefficient (ADC) values as well as an irregular contour and heterogeneous internal signal intensity seem to predict the involvement of pelvic lymphatic nodes better than their size alone.