Gross Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Do Bridging Veins Rupture Into the Virtual Subdural Space?
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.47.2.121 on 1 February 1984. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1984;47:121-127 Why do bridging veins rupture into the virtual subdural space? T YAMASHIMA, RL FRIEDE From the Department ofNeuropathology, University of Gottingen, Gottingen, Federal Republic of Germany SUMMARY Electron microscopic data on human bridging veins show thin walls of variable thick- ness, circumferential arrangement of collagen fibres and a lack of outer reinforcement by arach- noid trabecules, all contributory to the subdural portion of the vein being more fragile than its subarachnoid portion. These features explain the laceration of veins and the subdural location of resultant haematomas. Most subdural haematomas due to venous bleeding walls are delicate, lacking muscle fibres, with only a have been attributed to lacerations in bridging veins. thin fibrous wall and a thin elastic lamina adjacent to These veins form short trunks passing directly from the endothelial layer. The conclusions of these two the brain to the dura mater, almost at right angles to authors, have gained wide acceptance, although guest. Protected by copyright. both. Between these two points, bridging veins take there was little evidence concerning the fragility of a straight course with no tortuosity to allow for the the vein walls. possible displacement of brain.' Trotter2 speculated The purpose of the present communication is to that subdural haematomas are invariably due to provide electron microscopic data on tissue fixed in trauma tearing large veins, an interpretation situ, which might throw some light on to the lacera- elaborated by Krauland.3 According to Leary,4 the tion mechanism of bridging veins and its relationship common sources of subdural haematomas are rup- to the development of subdural haematoma. -

Diseases of Salivary Glands: Review
ISSN: 1812–1217 Diseases of Salivary Glands: Review Alhan D Al-Moula Department of Dental Basic Science BDS, MSc (Assist Lect) College of Dentistry, University of Mosul اخلﻻضة امخجوًف امفموي تُئة رطبة، حتخوي ػىل طبلة ركِلة من امسائل ثدغى انوؼاب ثغطي امسطوح ادلاخوَة و متﻷ امفراغات تني ااطَة امفموًة و اﻷس نان. انوؼاب سائل مؼلد، ًنذج من امغدد انوؼاتَة، اذلي ًوؼة دورا" ىاما" يف اﶈافظة ػىل سﻻمة امفم. املرىض اذلٍن ؼًاهون من هلص يف اﻷفراز انوؼايب حكون دلهيم مشبلك يف اﻷلك، امخحدث، و امبوع و ًطبحون غرضة مﻷههتاابت يف اﻷغش َة ااطَة و امنخر املندرش يف اﻷس نان. ًوخد ثﻻثة أزواج من امغدد انوؼاتَة ام ئرُسة – امغدة امنكفِة، امغدة حتت امفكِة، و حتت انوساهَة، موضؼيا ٍكون خارج امخجوًف امفموي، يف حمفظة و ميخد هظاهما املنَوي مَفرغ افرازاهتا. وًوخد أًضا" امؼدًد من امغدد انوؼاتَة امطغرية ، انوساهَة، اتحنكِة، ادلىوزيًة، انوساهَة احلنكِة وما كبل امرخوًة، ٍكون موضؼيا مﻷسفل و مضن امغشاء ااطي، غري حماطة مبحفظة مع هجاز كنَوي كطري. افرازات امغدد انوؼاتَة ام ئرُسة مُست مدشاهبة. امغدة امفكِة ثفرز مؼاب مطيل غين ابﻷمِﻻز، وامغدة حتت امفكِة ثنذج مؼاب غين اباط، أما امغدة حتت انوساهَة ثنذج مؼااب" مزخا". ثبؼا" ميذه اﻷخذﻻفات، انوؼاب املوحود يق امفم ٌشار امَو مكزجي. ح كرَة املزجي انوؼايب مُس ثس َطا" واملادة اﻷضافِة اموػة من لك املفرزات انوؼاتَة، اكمؼدًد من امربوثُنات ثنذلل ثرسػة وثوخطق هبدروكس َل اﻷتُذاًت مﻷس نان و سطوح ااطَة امفموًة. ثبدأ أمراض امغدد انوؼاتَة ػادة تخغريات اندرة يف املفرزات و ام كرتَة، وىذه امخغريات ثؤثر اثهواي" من خﻻل جشلك انووحية اجلرثومِة و املوح، اميت تدورىا ثؤدي اىل خنور مذفش َة وأمراض وس َج دامعة. ىذه اﻷمراض ميكن أن ثطبح شدًدة تؼد املؼاجلة امشؼاغَة ﻷن امؼدًد من احلاﻻت اجليازًة )مثل امسكري، امخوَف اهكُيس( ثؤثر يف اجلراين انوؼايب، و ٌش خيك املرض من حفاف يف امفم. -
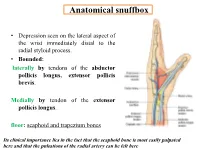
Anatomical Snuffbox
Anatomical snuffbox • Depression seen on the lateral aspect of the wrist immediately distal to the radial styloid process. • Bounded: laterally by tendons of the abductor pollicis longus, extensor pollicis brevis. Medially by tendon of the extensor pollicis longus. floor: scaphoid and trapezium bones Its clinical importance lies in the fact that the scaphoid bone is most easily palpated here and that the pulsations of the radial artery can be felt here Anatomical snuffbox Anatomical snuffbox • Contents: 2) Origin of the 1) The radial artery cephalic vein pass subcutaneously over the snuffbox. 3) Superficial branch of the radial nerve pass subcutaneously over the snuffbox. Blood supply of the hand Anastomoses occur between the radial and ulnar arteries via the superficial and deep palmar arches The Deep palmar arch is formed mainly by the radial artery while the superficial palmar arch is formed mainly by the ulnar artery 3-On entering the palm, it curves laterally behind (deep) the palmar 4-The arch is aponeurosis and in front completed on (superficial) of the long flexor the lateral side tendons forming by the the superficial palmar arch superficial branch of the radial artery. 2-Then it gives off its deep branch of which runs in front of the FR , and joins the radial artery to complete the deep palmar arch 1-Enters the hand anterior (superficial) to the Superficial flexor retinaculum palmar branch of radial artery through Guyon’s canal Radial artery 5-The superficial palmar arch gives off digital arteries from its convexity which pass to the fingers and supply them Superficial palmar arch Deep palmar branch of ulnar artery Superficial palmar branch of radial artery Ulnar artery Radial artery Radial Artery first dorsal interosseous muscle 1-From the floor of the anatomical snuff-box the radial artery leaves the dorsum of the hand by turning forward between the two heads of the first dorsal interosseous muscle. -

Variant Origins of Arteries in the Carotid Triangle - a Case Report
Case Report 281 Variant Origins of Arteries in the Carotid Triangle - A Case Report B. V. Murlimanju, MD; Latha V. Prabhu, MS; Mangala M. Pai, MD; Dhanya Jayaprakash, MBBS; Vasudha V. Saralaya, MS The left superior laryngeal artery was observed arising from the external carotid artery instead of the superior thyroid artery in the cadaver of an approximately 70 year-old Asian man. In addition, on the same side, the superior thyroid artery arose from the common carotid artery 2 cm before the bifurcation instead of its usual origin from the external carotid artery. From the external carotid artery, the lingual and facial arteries arose from the com- mon linguofacial trunk. The nerves in the carotid triangle were normal in course. No varia- tions were observed on the right side carotid system. The multiple variations in this case have not been previously described. The embryogenesis of this combination of variations is not clear, but the anatomic consequences may have important clinical implications. As angiography has gained popularity in diagnostic approaches in recent years, it is essential to be aware of these variations so that they are not overlooked in differential diagnoses. (Chang Gung Med J 2012;35:281-4) Key words: artery, superior laryngeal, superior thyroid, common carotid, external carotid, vari- ant origin natomical variations in the carotid triangle in the STA from the left CCA is reported here. In the Athe neck are important, especially during surgi- literature, a few variations in origin have been cal and radiological intervention in the region. reported for both arteries,(1-3) but the combination of Normally, the superior laryngeal artery (SLA) is a variations reported in this case has not been previ- branch of the superior thyroid artery (STA). -

Dynamic Assessment of Venous Anatomy and Function in Neurosurgery with Real-Time Intraoperative Multimodal Ultrasound: Technical Note
NEUROSURGICAL FOCUS Neurosurg Focus 45 (1):E6, 2018 Dynamic assessment of venous anatomy and function in neurosurgery with real-time intraoperative multimodal ultrasound: technical note Francesco Prada, MD,1,2 Massimiliano Del Bene, MD,1,3 Giovanni Mauri, MD,4 Massimo Lamperti, MD,5 Davide Vailati, MD,6 Carla Richetta, MD,7 Marco Saini, MD,1 Davide Santuari, MD,8 M. Yashar S. Kalani, MD, PhD,2 and Francesco DiMeco, MD1,9 1Department of Neurosurgery, Fondazione IRCCS Istituto Neurologico C. Besta, Milan, Italy; 2Department of Neurological Surgery, University of Virginia Health Science Center, Charlottesville, Virginia; Departments of 3Experimental Oncology and 4Radiology, European Institute of Oncology, Milan, Italy; 5Anesthesiology Unit, Cleveland Clinic, Abu Dhabi, United Arab Emirates; 6Anesthesiology Unit, Ospedale di Circolo di Melegnano, Presidio di Vizzolo Predabissi, Milan, Italy; 7Department of Neurosurgery, Sourasky Medical Center, Tel Aviv, Israel; 8Department of Vascular Surgery, Ospedale S. Carlo, Milan, Italy; and 9Department of Neurological Surgery, Johns Hopkins Medical School, Baltimore, Maryland The relevance of the cerebral venous system is often underestimated during neurosurgical procedures. Damage to this draining system can have catastrophic implications for the patient. Surgical decision-making and planning must consider each component of the venous compartment, from the medullary draining vein to the dural sinuses and extracranial veins. Intraoperative ultrasound (ioUS) permits the real-time study of venous compartments using different modalities, thus allowing complete characterization of their anatomical and functional features. The B-mode (brightness mode) offers a high-resolution anatomical representation of veins and their relationships with lesions. Doppler modalities (color, power, spectral) allow the study of blood flow and identification of vessels to distinguish their functional characteristics. -

Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions
Int. J. Morphol., 34(3):1063-1068, 2016. Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions Topografía Infraclavicular de los Fascículos del Plexo Braquial en Diferentes Posiciones del Miembro Superior Daniel Alves dos Santos*; Amilton Iatecola*; Cesar Adriano Dias Vecina*; Eduardo Jose Caldeira**; Ricardo Noboro Isayama**; Erivelto Luis Chacon**; Marianna Carla Alves**; Evanisi Teresa Palomari***; Maria Jose Salete Viotto**** & Marcelo Rodrigues da Cunha*,** ALVES DOS SANTOS, D.; IATECOLA, A.; DIAS VECINA, C. A.; CALDEIRA, E. J.; NOBORO ISAYAMA, R.; CHACON, E. L.; ALVES, M. C.; PALOMARI, E. T.; SALETE VIOTTO, M. J. & RODRIGUES DA CUNHA, M. Infraclavicular topography of the brachial plexus fascicles in different upper limb positions. Int. J. Morphol., 34 (3):1063-1068, 2016. SUMMARY: Brachial plexus neuropathies are common complaints among patients seen at orthopedic clinics. The causes range from traumatic to occupational factors and symptoms include paresthesia, paresis, and functional disability of the upper limb. Treatment can be surgical or conservative, but detailed knowledge of the brachial plexus is required in both cases to avoid iatrogenic injuries and to facilitate anesthetic block, preventing possible vascular punctures. Therefore, the objective of this study was to evaluate the topography of the infraclavicular brachial plexus fascicles in different upper limb positions adopted during some clinical procedures. A formalin- preserved, adult, male cadaver was used. The infraclavicular and axillary regions were dissected and the distance of the brachial plexus fascicles from adjacent bone structures was measured. No anatomical variation in the formation of the brachial plexus was observed. The metric relationships between the brachial plexus and adjacent bone prominences differed depending on the degree of shoulder abduction. -

Head & Neck Surgery Course
Head & Neck Surgery Course Parapharyngeal space: surgical anatomy Dr Pierfrancesco PELLICCIA Pr Benjamin LALLEMANT Service ORL et CMF CHU de Nîmes CH de Arles Introduction • Potential deep neck space • Shaped as an inverted pyramid • Base of the pyramid: skull base • Apex of the pyramid: greater cornu of the hyoid bone Introduction • 2 compartments – Prestyloid – Poststyloid Anatomy: boundaries • Superior: small portion of temporal bone • Inferior: junction of the posterior belly of the digastric and the hyoid bone Anatomy: boundaries Anatomy: boundaries • Posterior: deep fascia and paravertebral muscle • Anterior: pterygomandibular raphe and medial pterygoid muscle fascia Anatomy: boundaries • Medial: pharynx (pharyngobasilar fascia, pharyngeal wall, buccopharyngeal fascia) • Lateral: superficial layer of deep fascia • Medial pterygoid muscle fascia • Mandibular ramus • Retromandibular portion of the deep lobe of the parotid gland • Posterior belly of digastric muscle • 2 ligaments – Sphenomandibular ligament – Stylomandibular ligament Aponeurosis and ligaments Aponeurosis and ligaments • Stylopharyngeal aponeurosis: separates parapharyngeal spaces to two compartments: – Prestyloid – Poststyloid • Cloison sagittale: separates parapharyngeal and retropharyngeal space Aponeurosis and ligaments Stylopharyngeal aponeurosis Muscles stylohyoidien Stylopharyngeal , And styloglossus muscles Prestyloid compartment Contents: – Retromandibular portion of the deep lobe of the parotid gland – Minor or ectopic salivary gland – CN V branch to tensor -

Deep Neck Infections 55
Deep Neck Infections 55 Behrad B. Aynehchi Gady Har-El Deep neck space infections (DNSIs) are a relatively penetrating trauma, surgical instrument trauma, spread infrequent entity in the postpenicillin era. Their occur- from superfi cial infections, necrotic malignant nodes, rence, however, poses considerable challenges in diagnosis mastoiditis with resultant Bezold abscess, and unknown and treatment and they may result in potentially serious causes (3–5). In inner cities, where intravenous drug or even fatal complications in the absence of timely rec- abuse (IVDA) is more common, there is a higher preva- ognition. The advent of antibiotics has led to a continu- lence of infections of the jugular vein and carotid sheath ing evolution in etiology, presentation, clinical course, and from contaminated needles (6–8). The emerging practice antimicrobial resistance patterns. These trends combined of “shotgunning” crack cocaine has been associated with with the complex anatomy of the head and neck under- retropharyngeal abscesses as well (9). These purulent col- score the importance of clinical suspicion and thorough lections from direct inoculation, however, seem to have a diagnostic evaluation. Proper management of a recog- more benign clinical course compared to those spreading nized DNSI begins with securing the airway. Despite recent from infl amed tissue (10). Congenital anomalies includ- advances in imaging and conservative medical manage- ing thyroglossal duct cysts and branchial cleft anomalies ment, surgical drainage remains a mainstay in the treat- must also be considered, particularly in cases where no ment in many cases. apparent source can be readily identifi ed. Regardless of the etiology, infection and infl ammation can spread through- Q1 ETIOLOGY out the various regions via arteries, veins, lymphatics, or direct extension along fascial planes. -

Distal Radial Approach Through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention
Korean Circ J. 2018 Dec;48(12):1131-1134 https://doi.org/10.4070/kcj.2018.0293 pISSN 1738-5520·eISSN 1738-5555 Editorial Distal Radial Approach through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention Jae-Hyung Roh, MD, PhD, and Jae-Hwan Lee , MD, PhD Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea ► See the article “Feasibility of Coronary Angiography and Percutaneous Coronary Intervention via Left Snuffbox Approach” in volume 48 on page 1120. Received: Aug 27, 2018 The anatomical snuffbox, also known as the radial fossa, is a triangular-shaped depression Accepted: Sep 17, 2018 on the radial, dorsal aspect of the hand at the level of the carpal bones. It is clearly observed Figure 1 1)2) Correspondence to when the thumb is extended ( ). The bottom of the snuffbox is supported by carpal Jae-Hwan Lee, MD, PhD bones composed of the scaphoid and trapezium. The medial and lateral borders are bounded Division of Cardiology, Department of Internal by tendons of the extensor pollicis longus and the extensor pollicis brevis, respectively. The Medicine, Chungnam National University proximal border is formed by the styloid process of the radius. Within this narrow triangular Hospital, Chungnam National University space, various structures are located, including the distal radial artery (RA), a branch of the School of Medicine, 282, Munhwa-ro, Jung-gu, radial nerve, and the cephalic vein. Daejeon 35015, Korea. E-mail: [email protected] The anatomy of the hand arteries is illustrated in Figure 2. -

Ultrasound-Guided Access of the Distal Radial Artery at the Anatomical Snuffbox for Catheter-Based Vascular Interventions: a Technical Guide
Title: Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. Authors: Anastasia Hadjivassiliou, MBBS, BSc; Ferdinand Kiemeneij, M.D, PhD; Sandeep Nathan, M.D, MSc; Darren Klass, M.D, PhD DOI: 10.4244/EIJ-D-19-00555 Citation: Hadjivassiliou A, Kiemeneij F, Nathan S, Klass D. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. EuroIntervention 2019; Jaa-625 2019, doi: 10.4244/EIJ-D-19-00555 Manuscript submission date: 10 June 2019 Revisions received: 24 July 2019 Accepted date: 01 August 2019 Online publication date: 06 August 2019 Disclaimer: This is a PDF file of a "Just accepted article". This PDF has been published online early without copy editing/typesetting as a service to the Journal's readership (having early access to this data). Copy editing/typesetting will commence shortly. Unforeseen errors may arise during the proofing process and as such Europa Digital & Publishing exercise their legal rights concerning these potential circumstances. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide Anastasia Hadjivassiliou, MBBS, BSc1; Ferdinand Kiemeneij, MD, PhD2; Sandeep Nathan, MD, MSc3; Darren Klass, MD, PhD1 1. Department of Interventional Radiology, Vancouver General Hospital, University of British Columbia, Canada 2. Department of Cardiology, Tergooi Hospital, Blaricum, the Netherlands 3. University of Chicago Medicine, Chicago, IL, USA Short title: Ultrasound guided distal radial artery access at the anatomical snuffbox Corresponding author: Dr Darren Klass Department of Radiology, Vancouver General Hospital 899 West 12th Avenue, V5Z 1M9, Vancouver, BC, Canada Email address: [email protected] Disclaimer : As a public service to our readership, this article -- peer reviewed by the Editors of EuroIntervention - has been published immediately upon acceptance as it was received. -

Trigeminal Nerve, Mandibular Division Basic Anatomy and a Bit More
The palate and the faucial isthmus He who guards his mouth and his tongue keeps himself from calamity. Proverbs 21:23 Ph.D., Dr. David Lendvai Parts of the oral cavity Parts of the oral cavity 1. Vestibule of the oral cavity Borders: - lips and cheek (bucca) - dental arches 2. Oral cavity proper Borders: - roof: hard and soft palate - floor: oral diaphragm (mylohoid m.) - antero-laterally: dental arches - posteriorly: isthmus of the fauces Etrance of the oral cavity - Philtrum - Upper & lower lip - Angulus - Rubor labii - Nasolabial groove (Facial palsy) Sobotta Szentágothai - Réthelyi Aspectus anterior 1 zygomatic process 2 frontal process 2 4 alveolar process 1 4 Faller (left) lateral aspect 1 zygomatic process 2 frontal process 3 orbital surface 4 alveolar process 2 3 Sobotta 1 4 Faller (right) Medial aspect Sobotta Superior aspect Sobotta Inferior aspect Sobotta http://www.almanahmedical.eu Sobotta Florian Dental – Dr. S. Kovách Fehér Fehér Szél Szél http://www.hc-bios.com Structures of the hard palate - incisive papilla - palatine rugae - palatine raphe - torus Hard and soft palate Muscles of the soft palate - Levator veli palatini m. - Tensor veli palatini m. - Palatoglossus m. - Palatopharyngeus m. - M. uvulae Muscles of the soft palate Muscles of the soft palate Structures of the hard and soft palate - mucous membrane - palatine glands - bone / muscles Histology of the hard palate Mucoperiosteum Histology of the soft palate NASAL SURFACE - pseudostratified ciliated columnar epithelium - lamina propria - mucous glands - striated -

Normal Gross and Histologic Features of the Gastrointestinal Tract
NORMAL GROSS AND HISTOLOGIC 1 FEATURES OF THE GASTROINTESTINAL TRACT THE NORMAL ESOPHAGUS left gastric, left phrenic, and left hepatic accessory arteries. Veins in the proximal and mid esopha- Anatomy gus drain into the systemic circulation, whereas Gross Anatomy. The adult esophagus is a the short gastric and left gastric veins of the muscular tube measuring approximately 25 cm portal system drain the distal esophagus. Linear and extending from the lower border of the cri- arrays of large caliber veins are unique to the distal coid cartilage to the gastroesophageal junction. esophagus and can be a helpful clue to the site of It lies posterior to the trachea and left atrium a biopsy when extensive cardiac-type mucosa is in the mediastinum but deviates slightly to the present near the gastroesophageal junction (4). left before descending to the diaphragm, where Lymphatic vessels are present in all layers of the it traverses the hiatus and enters the abdomen. esophagus. They drain to paratracheal and deep The subdiaphragmatic esophagus lies against cervical lymph nodes in the cervical esophagus, the posterior surface of the left hepatic lobe (1). bronchial and posterior mediastinal lymph nodes The International Classification of Diseases in the thoracic esophagus, and left gastric lymph and the American Joint Commission on Cancer nodes in the abdominal esophagus. divide the esophagus into upper, middle, and lower thirds, whereas endoscopists measure distance to points in the esophagus relative to the incisors (2). The esophagus begins 15 cm from the incisors and extends 40 cm from the incisors in the average adult (3). The upper and lower esophageal sphincters represent areas of increased resting tone but lack anatomic landmarks; they are located 15 to 18 cm from the incisors and slightly proximal to the gastroesophageal junction, respectively.