Axillary Lymph Node Dissection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Tip: Swollen Lymph "Glands" - When Should You Be Concerned?
Printer Friendly Version Page 1 of 3 Health Tip: Swollen lymph "glands" - When should you be concerned? Lymph nodes, sometimes referred to as lymph "glands", are part of the body's lymphatic system. The lymphatic system consists of a system of conduits and organized collections of lymphoid tissue that include nodes, the tonsils, and the spleen. Coursing through these channels is liquid called lymph that eventually drains into the bloodstream near the heart, but along the way, it is "filtered" by the lymph nodes. Within these lymph nodes are high concentrations of disease fighting cells, particularly lymphocytes. While performing their intended function of fighting infection, lymph nodes typically become enlarged. In fact, infection is most common reason for lymph nodes enlargement. Lymph nodes are found throughout the body, but when enlarged, are usually noticed in characteristic locations, particularly the neck, groin and armpit regions. Lymph node enlargement can be localized to one group of lymph nodes or can be generalized (involving several sites of lymph nodes). For example, enlarged lymph nodes localized to the arm pit could occur as a result of a bacterial infection in a hand wound. Generalized lymph node swelling, on the other hand, could be seen in a systemic illness such as viral mononucleosis. In addition to viral and bacterial infections, other causes for enlarged lymph nodes include immune disorders (lupus, rheumatoid arthritis, etc.), cancers affecting the lymphatic system (leukemia, lymphoma, Hodgkin's disease), and cancers that have spread (metastasized) from some other part of the body to the lymphatic system. The discovery of enlarged lymph nodes often causes concern because many people are aware that lymph node enlargement can be an early sign of cancer. -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -
201028 the Lymphatic System 2 – Structure and Function of The
Copyright EMAP Publishing 2020 This article is not for distribution except for journal club use Clinical Practice Keywords Immunity/Anatomy/Stem cell production/Lymphatic system Systems of life This article has been Lymphatic system double-blind peer reviewed In this article... l How blood and immune cells are produced and developed by the lymphatic system l Clinical significance of the primary and secondary lymphoid organs l How the lymphatic system mounts an immune response and filters pathogens The lymphatic system 2: structure and function of the lymphoid organs Key points Authors Yamni Nigam is professor in biomedical science; John Knight is associate The lymphoid professor in biomedical science; both at the College of Human and Health Sciences, organs include the Swansea University. red bone marrow, thymus, spleen Abstract This article is the second in a six-part series about the lymphatic system. It and clusters of discusses the role of the lymphoid organs, which is to develop and provide immunity lymph nodes for the body. The primary lymphoid organs are the red bone marrow, in which blood and immune cells are produced, and the thymus, where T-lymphocytes mature. The Blood and immune lymph nodes and spleen are the major secondary lymphoid organs; they filter out cells are produced pathogens and maintain the population of mature lymphocytes. inside the red bone marrow, during a Citation Nigam Y, Knight J (2020) The lymphatic system 2: structure and function of process called the lymphoid organs. Nursing Times [online]; 116: 11, 44-48. haematopoiesis The thymus secretes his article discusses the major become either erythrocytes, leucocytes or hormones that are lymphoid organs and their role platelets. -
Lymphatic System
LYMPHATIC SYSTEM Associated with the Blood and Cardiovascular System http://www.lymphnotes.com/article.php/id/151/ http://www.youtube.com/watch?v=qTXTDqvPnRk http://www.scribd.com/doc/60675255/Handouts- Lymphatic-System-F11 http://www.learningace.com/doc/5949560/9178 e2f0064b410c8c8e9218bcc748e6/ama-180- course-handouts Lymphatic System Lymph Fluid Lymph Vessels Lymph Nodes Four Organs Tonsils Spleen Thymus Gland Peyer’s Patches Functions Drain from tissue spaces, protein-containing fluid that escapes from the blood capillaries Transport fats from the digestive tract to the blood Produce lymphocytes Develop Immunities Interstitial Fluid Blood pressure forces some of the blood plasma through the single-celled capillary walls Interstitial Fluid is in the spaces between cells Most is reabsorbed into the capillaries Some fluid is not and must be drained from the tissue spaces to prevent swelling or Edema. Lymphatic Capillaries – drain this fluid Lymph is the fluid when it is in the vessels Fat Absorption Lacteals – lymphatic vessels in the villi of the small intestine that absorb fats and transport them to the blood. Looks milky because of the fat content and is called chyle. Lymphatic Vessels Lymph Capillaries Larger and more permeable than blood capillaries Closed at one end Occur singly or in extensive plexuses Lymphatic Capillaries Lymphatics Combined capillaries Larger Beaded appearance Similar to veins, but thinner walls and more valves One way valves to prevent backflow Lymph goes in one direction only -

Anatomy and Physiology in Relation to Compression of the Upper Limb and Thorax
Clinical REVIEW anatomy and physiology in relation to compression of the upper limb and thorax Colin Carati, Bren Gannon, Neil Piller An understanding of arterial, venous and lymphatic flow in the upper body in normal limbs and those at risk of, or with lymphoedema will greatly improve patient outcomes. However, there is much we do not know in this area, including the effects of compression upon lymphatic flow and drainage. Imaging and measuring capabilities are improving in this respect, but are often expensive and time-consuming. This, coupled with the unknown effects of individual, diurnal and seasonal variances on compression efficacy, means that future research should focus upon ways to monitor the pressure delivered by a garment, and its effects upon the fluids we are trying to control. More is known about the possible This paper will describe the vascular Key words effects of compression on the anatomy of the upper limb and axilla, pathophysiology of lymphoedema when and will outline current understanding of Anatomy used on the lower limbs (Partsch and normal and abnormal lymph drainage. It Physiology Junger, 2006). While some of these will also explain the mechanism of action Lymphatics principles can be applied to guide the use of compression garments and will detail Compression of compression on the upper body, it is the effects of compression on fluid important that the practitioner is movement. knowledgeable about the anatomy and physiology of the upper limb, axilla and Vascular drainage of the upper limb thorax, and of the anatomical and vascular It is helpful to have an understanding of Little evidence exists to support the differences that exist between the upper the vascular drainage of the upper limb, use of compression garments in the and lower limb, so that the effects of these since the lymphatic drainage follows a treatment of lymphoedema, particularly differences can be considered when using similar course (Figure 1). -

Page 1 Chapter 19: the Lymphatic System
Chapter 19: The Lymphatic System Pathogens: Microscopic organisms that cause disease Viruses Bacteria Fungi Protists Chapter 19: Lymphatic System Lymphoid System: • Defends body against external (e.g., pathogens) and internal (e.g., cancer cells) threats Composed of: 1) Lymph: Fluid portion (resembles plasma) 2) Lymphatic vessels: One-way flow; empty into veins 3) Lymphoid tissues / organs (e.g., spleen) Functions: • Produce / maintain / distribute lymphocytes Lymphocytes: • Recognize and respond to threats: a) Pathogens b) Abnormal body cells c) Foreign proteins • Return excess fluids to bloodstream • Distributes hormones / nutrients / waste products Page 1 1 Chapter 19: Lymphatic System Similar to Marieb & Hoehn – Figure 19.1 Flow of Lymph: • Originate as pockets Lymphatic Capillaries • Large diameters / thin walls • One-way valves (external) • Multi-layered walls Lymphatic Vessels • Travel with blood vessels • One-way valves (internal) Two Types: Collecting Vessels • Superficial (e.g., skin) • Deep (e.g., skeletal muscle) Lymphatic Trunks Lymphatic Ducts Chapter 19: Lymphatic System Similar to Marieb & Hoehn – Figure 19.2 Flow of Lymph: • Lymph from right side of • Lymph from left side of body above diaphragm head, neck, and thorax Thoracic Duct: • Begins inferior to diaphragm • Empties into left subclavian vein Right Lymphatic Duct: • Empties into right subclavian vein Cisterna chyli • Lymph from abdomen, Lymphedema: Fluid build up in tissues due to pelvis, and lower limbs blockage of lymph drainage Page 2 2 Chapter 19: Lymphatic -
Hand and Arm Guidelines After Your Axillary Lymph Node Dissection
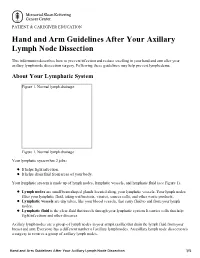
PATIENT & CAREGIVER EDUCATION Hand and Arm Guidelines After Your Axillary Lymph Node Dissection This information describes how to prevent infection and reduce swelling in your hand and arm after your axillary lymph node dissection surgery. Following these guidelines may help prevent lymphedema. About Your Lymphatic System Figure 1. Normal lymph drainage Figure 1. Normal lymph drainage Your lymphatic system has 2 jobs: It helps fight infection. It helps drain fluid from areas of your body. Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1). Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products. Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes. Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases. Axillary lymph nodes are a group of lymph nodes in your armpit (axilla) that drain the lymph fluid from your breast and arm. Everyone has a different number of axillary lymph nodes. An axillary lymph node dissection is a surgery to remove a group of axillary lymph nodes. Hand and Arm Guidelines After Your Axillary Lymph Node Dissection 1/5 About Lymphedema Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema. -

Lymphocyte Recirculation
Lymphocyte Recirculation Chapter 15 Naïve lymphocytes enter lymph nodes Lymphocyte Migration and from the blood circulation Lymphocytes return Inflammation to blood via the thoracic duct Antigens from infected area go to lymph nodes via the lymphatic system I. Primary Lymphoid II. Secondary - Lymph Nodes -Spleen -MALT Lymphatic vessels Leukocytes are constantly moving between sites where - Collect interstitial fluid and carry antigens may be It (lymph), via a system of encountered: progressively larger vessels, into regional lymph nodes. 1 2 - Spleen (via afferent lymphatic vessels). - Lymph nodes - Other secondary -Lymph leaves the lymph nodes lymphoid tissues via efferent lymphatic vessels, - Other tissues – which eventually drain back especially skin and into the circulatory system (via mucosal surfaces the thoracic duct). 3 Leukocytes accumulate at sites of inflammation 1 CHOICES: Antigen capture: (APC) or 1) If no antigen is present: lymphocytes Macrophages: capture and process particulate routinely enter and leave secondary lymphoid antigens (via phagocytosis) tissues Dendritic cells: capture and process non- 2) If antigen enters the secondary lymphoid particulate antigens (via endocytosis) tissue: Lymphocyte proliferation in response to antigen B cells: capture and process antigens that bind to occurs within the lymphoid tissue. surface BCR (via endocytosis) After several days, antigen-activated lymphocytes begin leaving the lymphoid tissue. Dendritic cells: originate in bone marrow, capture antigen within tissues and transport antigen to secondary lymphoid tissue. Lymphocytes can enter lymphoid tissues in two ways: 1 1) Direct entry into lymph nodes via afferent lymphatics 2) Entry from blood capillaries across specialized endothelial cells (high-walled endothelial cells) present in the postcapillary venules (High Endothelial Venules= HEV) within the secondary 2 lymphoid tissue. -
The Lymphatic System
Freephone helpline 0808 808 5555 [email protected] www.lymphoma-action.org.uk The lymphatic system Lymphoma is a cancer of the lymphatic system. The lymphatic system is part of your immune system, which helps protect you from infection. It is spread throughout your body, like blood vessels, and it has many different parts. This page tells you about the different parts of the lymphatic system and what they do. On this page What is the lymphatic system? Lymph Lymph nodes Bone marrow Thymus Spleen Tonsils and adenoids Mucosa-associated lymphoid tissue The lymphatic system and lymphoma What is the lymphatic system and what does it do? The lymphatic system runs throughout the body, like your blood circulatory system. The lymphatic system carries a fluid called ‘lymph’ around the body in lymph vessels (tubes). The fluid passes through lymph nodes (glands), which are spread throughout your body. Figure: The lymphatic system (lymph vessels and lymph nodes are shown in green) The lymphatic system also includes organs and tissues that are places where immune system cells collect. These include the parts of the body that make cells for the immune system: the bone marrow the thymus. They also include areas where immune cells collect, ready to fight infection: lymph nodes the spleen the tonsils and adenoids mucosa-associated lymphoid tissue. The lymphatic system defends your body against disease by removing germs (bacteria, viruses and parasites) and toxins (poisons). It also helps to destroy cells that are old, damaged or have become abnormal. It has other important functions too: As a drainage system, it removes excess fluid and waste from your tissues and returns it to your bloodstream. -
Axillary Lymph Nodes
FACTS FOR LIFE Axillary Lymph Nodes Lymphatic system and axillary nodes Lymph nodes are part of the lymphatic system, which carries waste products and other materials away from the cells in your body. These materials are carried to the lymph nodes in a colorless fluid called lymph. Lymph nodes filter this fluid before it returns to the blood stream. Lymph nodes also store white blood cells (called lymphocytes) that help fight infection. Lymph nodes in the underarm are called the axillary [AK-sil-air-e] nodes, and are important in determining breast cancer stage and the likelihood that breast cancer has spread to other parts of the body. During surgery, some axillary nodes are removed to see if cancer cells are present. Axillary nodes and breast cancer The lymphatic system runs throughout the body. The axillary nodes form a chain from the underarm to the collarbone. Level 1 nodes are located in the underarm and receive most of the lymph fluid from collarbone the breast. Level 2 nodes are farther up and receive the level 3 fluid from Level 1 and some fluid from the breast and level 2 chest wall. Level 3 nodes are below the collarbone and supraclavicular level 1 receive fluid from Levels 1 and 2 and from the upper nodes part of the breast and chest wall. Supraclavicular lymph nodes are located above the collarbone. When internal breast cancer develops, Level 1 nodes are usually mammary affected first. nodes To determine whether or not lymph nodes are involved in the breast cancer, axillary nodes are often removed from Levels 1 and 2 during surgery. -
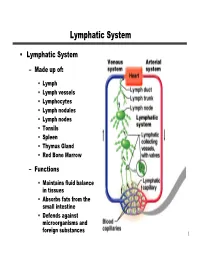
Lymphatic System
Lymphatic System • Lymphatic System – M ade up of: • Lymph • Lymph vessels • Lymphocytes • Lymph nodules • Lymph nodes • Tonsils • Spleen • Thymus Gland • Red Bone M arrow – Functions • M aintains fluid balance in tissues • Absorbs fats from the small intestine • Defends against microorganisms and foreign substances 1 Lymphatic System • Lymph Capillaries – Lack a basement membrane – Epithelial cells loosely overlap – Lymph Transport 2 3 4 Lymphatic System • Lymph Trunks and Ducts 5 Lymphatic System • Lymphoid Cells – Lymphocytes • “M ain W arriors” • Produced w here? • Protect against antigens • Tw o major types – T Cells » Orchestrate the immune response » Some are direct killers that destroy foreign antigens – B Cells » Produce plasma cells that in turn produce antibodies 6 Lymphatic System – Lymphoid M acrophages • Eat and destroy foreign antigens • Play a role in activating T Cells – Dendritic Cells • Function like macrophages • Appear spiny • Found in lymphoid tissues – Reticular Cells • Produce the fibrous stroma located in lymphoid organs 7 Lymphatic System • Lymphoid Tissues – Houses lymphocytes – Provides a “check point” for lymphocytes and macrophages to w ork – Composed of several types • ReticuarCT – Found in all lymphoid organs except the thymus gland » M acrophages live on the fibers » Lymphocytes live in the spaces betw een the fibers 8 Lymphatic System • Diffuse Lymphatic Tissue – Scattered reticular tissue elements found in virtually all body organs – Larger numbers are found in mucous membranes • Lymphoid Follicles (nodules) -

Axillary Lymph Nodes and Breast Cancer
AXILLARY LYMPH NODES Lymphatic system and axillary nodes The lymphatic system runs through the body. It carries lymph from tissues and organs to lymph nodes. Lymph nodes are small clumps of immune cells that act as filters for the lymphatic system. They also store white blood cells that help fight illness. The lymph nodes in the underarm are called axillary lymph nodes. If breast cancer spreads, this is the first place it’s likely to go. During breast surgery, some axillary nodes may be removed to see if they contain cancer. This helps determine breast cancer stage and guide treatment. Lymph node status is related to tumor size. The larger the tumor, the more likely it is the breast cancer has spread to the lymph nodes (lymph node-positive). Sentinel node biopsy To see if cancer has spread to the axillary lymph nodes, The lymphatic system runs through the body. most people have a sentinel node biopsy. Before or during the procedure, a radioactive substance (called a tracer) and/ or a blue dye is injected into the breast. The first lymph supraclavicular nodes nodes to absorb the tracer or dye are called the sentinel nodes. These are also the first lymph nodes where breast cancer is likely to spread. internal mammary The surgeon removes the sentinel nodes and sends them nodes to the lab. When the surgeon removes the sentinel nodes, it doesn’t mean there’s cancer in the nodes. It means a pathologist needs to check the nodes for cancer. If the nodes contain cancer, more lymph nodes may be removed.