Axillary Lymph Node Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Tip: Swollen Lymph "Glands" - When Should You Be Concerned?
Printer Friendly Version Page 1 of 3 Health Tip: Swollen lymph "glands" - When should you be concerned? Lymph nodes, sometimes referred to as lymph "glands", are part of the body's lymphatic system. The lymphatic system consists of a system of conduits and organized collections of lymphoid tissue that include nodes, the tonsils, and the spleen. Coursing through these channels is liquid called lymph that eventually drains into the bloodstream near the heart, but along the way, it is "filtered" by the lymph nodes. Within these lymph nodes are high concentrations of disease fighting cells, particularly lymphocytes. While performing their intended function of fighting infection, lymph nodes typically become enlarged. In fact, infection is most common reason for lymph nodes enlargement. Lymph nodes are found throughout the body, but when enlarged, are usually noticed in characteristic locations, particularly the neck, groin and armpit regions. Lymph node enlargement can be localized to one group of lymph nodes or can be generalized (involving several sites of lymph nodes). For example, enlarged lymph nodes localized to the arm pit could occur as a result of a bacterial infection in a hand wound. Generalized lymph node swelling, on the other hand, could be seen in a systemic illness such as viral mononucleosis. In addition to viral and bacterial infections, other causes for enlarged lymph nodes include immune disorders (lupus, rheumatoid arthritis, etc.), cancers affecting the lymphatic system (leukemia, lymphoma, Hodgkin's disease), and cancers that have spread (metastasized) from some other part of the body to the lymphatic system. The discovery of enlarged lymph nodes often causes concern because many people are aware that lymph node enlargement can be an early sign of cancer. -
Follicular Lymphoma
Follicular Lymphoma What is follicular lymphoma? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines FOLLICULAR LYMPHOMA: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of follicular lymphoma and appreciate the best treatment choices available according to the subtype of follicular lymphoma. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of newly diagnosed and relapsed follicular lymphoma. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the lead author of the clinical practice guidelines for professionals, as well as two oncology nurses from the European Oncology Nursing Society (EONS). It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Follicular Lymphoma: a guide for patients - Information based on ESMO Clinical Practice Guidelines – v.2014.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO. -

The Landmark Series: Axillary Management in Breast Cancer
Ann Surg Oncol (2020) 27:724–729 https://doi.org/10.1245/s10434-019-08154-5 ORIGINAL ARTICLE – BREAST ONCOLOGY The Landmark Series: Axillary Management in Breast Cancer Carla S. Fisher, MD1, Julie A. Margenthaler, MD2, Kelly K. Hunt, MD3, and Theresa Schwartz, MD4 1Department of Surgery, Indiana University School of Medicine, Indianapolis, IN; 2Department of Surgery, Washington University School of Medicine, St. Louis, MO; 3Department of Breast Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX; 4Department of Surgery, St. Louis University, St. Louis, MO ABSTRACT The evolution in axillary management for AXILLARY MANAGEMENT IN PATIENTS patients with breast cancer has resulted in multiple dra- UNDERGOING PRIMARY SURGICAL THERAPY matic changes over the past several decades. The end result has been an overall deescalation of surgery in the axilla. For many patients with breast cancer, surgery is the first Landmark trials that have formed the basis for the current line of therapy for treatment and staging. When the Halsted treatment guidelines are reviewed herein. radical mastectomy was introduced, the axilla was seen as a transit point between the breast and distant metastatic disease, and it was believed that removal of axillary nodes Axillary management for patients with newly diagnosed was necessary to prevent distant metastatic spread. As breast cancer has undergone several practice-changing understanding of breast cancer evolved, removal of these paradigm shifts over the last few decades with the ultimate lymph nodes was not viewed as a necessary procedure to goal of reducing morbidity without compromising onco- prevent spread but rather an important component of breast logic outcomes or staging. -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -

December 2020 E-Tips Solid Tumor Rules
New Jersey State Cancer Registry December 2020 E-Tips Cancer Epidemiology Services http://www.nj.gov/health/ces (609) 633-0500 Solid Tumor Rules: December 2020 Update ICD-0-3.2 changes have also been added to applicable site modules. Most changes are minor: terminology, additional definitions, new notes and examples. In order to clarify histology coding instructions, new rules have been added and histology tables updated. These updates do not require review of already abstracted cases. The December 2020 rules replace the current rules and should be used now. SEER Strongly recommends reading the December 2020 Change Log to understand what changes were made. The updated Solid Tumor Rules may be accessed at: https://seer.cancer.gov/tools/solidtumor/ Reportability Changes for 2021 Radiation Coding Total Dose (1533) Starting 01/01/2021 the following terms are reportable: If doses across phases to a single point of region, code Sum of all phases. ** (see 2019 update below) Early or evolving melanoma in situ, or any other early or If doses are to multiple metastatic sites, code highest evolving melanoma, are reportable. dose site. If doses are to primary site and metastatic site, code dose All GIST tumors are reportable and classified as 8936/3 in from the primary site only. ICD-O-3.2. When you have two different sites, you cannot add the Nearly all thymomas are reportable; the exceptions are doses together to get the total dose. microscopic thymoma or thymoma benign (8580/0), micronodular thymoma with lymphoid stroma (8580/1), Radiation Tips and updates for 2019 and ectopic hamartomatous thymoma (8587/0). -
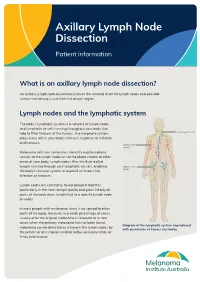
Axillary Lymph Node Dissection
Axillary Lymph Node Dissection Patient information What is an axillary lymph node dissection? An axillary lymph node dissection involves the removal of all the lymph nodes and possible tumour-containing tissue from the armpit region. Lymph nodes and the lymphatic system The body’s lymphatic system is a network of lymph nodes and lymphatic vessels running throughout your body that help to filter fluid out of the tissues. The lymphatic system plays a key role in your body’s immune response to infection and tumours. Melanoma cells can sometimes travel through lymphatic vessels to the lymph nodes or via the blood stream to other areas of your body. Lymph nodes filter the fluid (called lymph) running through your lymphatic vessels, enabling the body’s immune system to respond to threats like infection or tumours. Lymph nodes are commonly found grouped together, particularly in the neck, armpit (axilla) and groin. Nearly all parts of the body drain lymph fluid to a specific lymph node or nodes. In most people with melanoma, there is no spread to other parts of the body. However, in a small percentage of cases, usually after the original melanoma is removed or in rare cases when the primary melanoma has not been found, Diagram of the lymphatic system (reproduced melanoma can be detected as a lump in the lymph nodes by with permission of Cancer Australia). the patient or at a regular medical follow up examination or X-ray examination. In this situation, the standard treatment has been to remove all the lymph nodes in that area as often there is more than one lymph node involved. -
201028 the Lymphatic System 2 – Structure and Function of The
Copyright EMAP Publishing 2020 This article is not for distribution except for journal club use Clinical Practice Keywords Immunity/Anatomy/Stem cell production/Lymphatic system Systems of life This article has been Lymphatic system double-blind peer reviewed In this article... l How blood and immune cells are produced and developed by the lymphatic system l Clinical significance of the primary and secondary lymphoid organs l How the lymphatic system mounts an immune response and filters pathogens The lymphatic system 2: structure and function of the lymphoid organs Key points Authors Yamni Nigam is professor in biomedical science; John Knight is associate The lymphoid professor in biomedical science; both at the College of Human and Health Sciences, organs include the Swansea University. red bone marrow, thymus, spleen Abstract This article is the second in a six-part series about the lymphatic system. It and clusters of discusses the role of the lymphoid organs, which is to develop and provide immunity lymph nodes for the body. The primary lymphoid organs are the red bone marrow, in which blood and immune cells are produced, and the thymus, where T-lymphocytes mature. The Blood and immune lymph nodes and spleen are the major secondary lymphoid organs; they filter out cells are produced pathogens and maintain the population of mature lymphocytes. inside the red bone marrow, during a Citation Nigam Y, Knight J (2020) The lymphatic system 2: structure and function of process called the lymphoid organs. Nursing Times [online]; 116: 11, 44-48. haematopoiesis The thymus secretes his article discusses the major become either erythrocytes, leucocytes or hormones that are lymphoid organs and their role platelets. -
Lymphatic System
LYMPHATIC SYSTEM Associated with the Blood and Cardiovascular System http://www.lymphnotes.com/article.php/id/151/ http://www.youtube.com/watch?v=qTXTDqvPnRk http://www.scribd.com/doc/60675255/Handouts- Lymphatic-System-F11 http://www.learningace.com/doc/5949560/9178 e2f0064b410c8c8e9218bcc748e6/ama-180- course-handouts Lymphatic System Lymph Fluid Lymph Vessels Lymph Nodes Four Organs Tonsils Spleen Thymus Gland Peyer’s Patches Functions Drain from tissue spaces, protein-containing fluid that escapes from the blood capillaries Transport fats from the digestive tract to the blood Produce lymphocytes Develop Immunities Interstitial Fluid Blood pressure forces some of the blood plasma through the single-celled capillary walls Interstitial Fluid is in the spaces between cells Most is reabsorbed into the capillaries Some fluid is not and must be drained from the tissue spaces to prevent swelling or Edema. Lymphatic Capillaries – drain this fluid Lymph is the fluid when it is in the vessels Fat Absorption Lacteals – lymphatic vessels in the villi of the small intestine that absorb fats and transport them to the blood. Looks milky because of the fat content and is called chyle. Lymphatic Vessels Lymph Capillaries Larger and more permeable than blood capillaries Closed at one end Occur singly or in extensive plexuses Lymphatic Capillaries Lymphatics Combined capillaries Larger Beaded appearance Similar to veins, but thinner walls and more valves One way valves to prevent backflow Lymph goes in one direction only -
About Mastectomy and Sentinel Lymph Node Biopsy
All About Mastectomy and Sentinel Lymph Node Biopsy One of the most important goals of Moffitt Cancer Center is to provide you with quality patient care through education, research and patient care. The following information has been developed to help you understand the mastectomy and sentinel lymph node biopsy procedures for which you have been scheduled. Members of your health care team will review this information with you and answer any questions that you may have. Definitions: Mastectomy – Removal of the entire breast but not the muscles underneath. Lymph Nodes - Small bean shaped glands found in the armpit. They remove waste and fluids from the arm and breast and help fight infection. They are also call lymph glands. Sentinel Lymph Node - The first place breast cancer may metastasize (or spread) is to lymph nodes in the axilla (underarm area) on the side of the body where the cancer is. The first lymph node(s) are referred to as the sentinel lymph node(s) or the “gate keepers”. These nodes are first biopsied to determine if the cancer has spread. If cancer cells are not found in the sentinel lymph node(s) that were removed, it will not be necessary to remove the remaining lymph nodes in the arm pit. Sentinel Lymph Node Mapping and Biopsy - This procedure is a two step process. Performing the sentinel lymph node biopsy requires a small incision in your axilla. In the first step, the doctor injects a radioactive substance and/ or blue dye in the area around the tumor. Lymphatic channels (like blood vessels) carry these materials to the sentinel lymph node. -

Consensus Guideline on the Management of the Axilla in Patients with Invasive/In-Situ Breast Cancer
- Official Statement - Consensus Guideline on the Management of the Axilla in Patients With Invasive/In-Situ Breast Cancer Purpose To outline the management of the axilla for patients with invasive and in-situ breast cancer. Associated ASBrS Guidelines or Quality Measures 1. Performance and Practice Guidelines for Sentinel Lymph Node Biopsy in Breast Cancer Patients – Revised November 25, 2014 2. Performance and Practice Guidelines for Axillary Lymph Node Dissection in Breast Cancer Patients – Approved November 25, 2014 3. Quality Measure: Sentinel Lymph Node Biopsy for Invasive Breast Cancer – Approved November 4, 2010 4. Prior Position Statement: Management of the Axilla in Patients With Invasive Breast Cancer – Approved August 31, 2011 Methods A literature review inclusive of recent randomized controlled trials evaluating the use of sentinel lymph node surgery and axillary lymph node dissection for invasive and in-situ breast cancer as well as the pathologic review of sentinel lymph nodes and indications for axillary radiation was performed. This is not a complete systematic review but rather, a comprehensive review of recent relevant literature. A focused review of non-randomized controlled trials was then performed to develop consensus guidance on management of the axilla in scenarios where randomized controlled trials data is lacking. The ASBrS Research Committee developed a consensus document, which was reviewed and approved by the ASBrS Board of Directors. Summary of Data Reviewed Recommendations Based on Randomized Controlled -

Anatomy and Physiology in Relation to Compression of the Upper Limb and Thorax
Clinical REVIEW anatomy and physiology in relation to compression of the upper limb and thorax Colin Carati, Bren Gannon, Neil Piller An understanding of arterial, venous and lymphatic flow in the upper body in normal limbs and those at risk of, or with lymphoedema will greatly improve patient outcomes. However, there is much we do not know in this area, including the effects of compression upon lymphatic flow and drainage. Imaging and measuring capabilities are improving in this respect, but are often expensive and time-consuming. This, coupled with the unknown effects of individual, diurnal and seasonal variances on compression efficacy, means that future research should focus upon ways to monitor the pressure delivered by a garment, and its effects upon the fluids we are trying to control. More is known about the possible This paper will describe the vascular Key words effects of compression on the anatomy of the upper limb and axilla, pathophysiology of lymphoedema when and will outline current understanding of Anatomy used on the lower limbs (Partsch and normal and abnormal lymph drainage. It Physiology Junger, 2006). While some of these will also explain the mechanism of action Lymphatics principles can be applied to guide the use of compression garments and will detail Compression of compression on the upper body, it is the effects of compression on fluid important that the practitioner is movement. knowledgeable about the anatomy and physiology of the upper limb, axilla and Vascular drainage of the upper limb thorax, and of the anatomical and vascular It is helpful to have an understanding of Little evidence exists to support the differences that exist between the upper the vascular drainage of the upper limb, use of compression garments in the and lower limb, so that the effects of these since the lymphatic drainage follows a treatment of lymphoedema, particularly differences can be considered when using similar course (Figure 1). -

Prognostic Significance of Lymph Node Examination by the OSNA
cells Article Prognostic Significance of Lymph Node Examination by the OSNA Method in Lung Cancer Patients—Comparison with the Standard Histopathological Procedure Josef Vodicka 1 , Martin Pesta 2,3,*, Vlastimil Kulda 4 , Katerina Houfkova 2, Bohuslava Vankova 5, Jakub Sebek 1, Martin Skala 1, Jakub Fichtl 1, Kristyna Prochazkova 1 and Ondrej Topolcan 6 1 Department of Surgery, Faculty Hospital Plzen, Faculty of Medicine in Pilsen, Charles University, alej Svobody 80, 304 60 Plzen, Czech Republic; [email protected] (J.V.); [email protected] (J.S.); [email protected] (M.S.); fi[email protected] (J.F.); [email protected] (K.P.) 2 Department of Biology, Faculty of Medicine in Pilsen, Charles University, alej Svobody 76, 323 00 Plzen, Czech Republic; [email protected] 3 Biomedical Center, Faculty of Medicine in Pilsen, Charles University, alej Svobody 76, 323 00 Plzen, Czech Republic 4 Department of Medical Chemistry and Biochemistry, Faculty of Medicine in Pilsen, Charles University, Karlovarska 48, 301 66 Plzen, Czech Republic; [email protected] 5 Department of Pathology, Faculty Hospital Plzen, Faculty of Medicine in Pilsen, Charles University, Edvarda Benese 13, 305 99 Plzen, Czech Republic; [email protected] 6 Department of Immunochemistry Diagnostics, Faculty Hospital Plzen, Faculty of Medicine in Pilsen, Charles University, Edvarda Benese 13, 305 99 Plzen, Czech Republic; [email protected] * Correspondence: [email protected]; Tel.: +420-377-593-261 Received: 26 October 2020; Accepted: 1 December 2020; Published: 4 December 2020 Abstract: The aim of the study was to compare the prognostic significance of lymph node status of patients with lung cancer analyzed by three different methods: hematoxylin and eosin (H&E), immunohistochemistry of cytokeratin 19 (IHC CK19), and One-Step Nucleic Acid Amplification (OSNA).