Lymphocyte Recirculation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

Thalassemia and the Spleen
Thalassemia and the Spleen 4 Living with Thalassemia are developing an infection (fever, chills, sore throats, unexplained coughs, listlessness, muscle pain, etc.) and Issues in Thalassemia report them to your doctor right away. Thalassemia Care • Sometimes a splenectomy can lead to an exceptionally and the Spleen high platelet count, which can in turn lead to blood clotting. by Marie B. Martin, RN, and Craig Butler Your doctor should monitor your platelet count on a regular basis and may ask you to take baby aspirin daily. This sounds kind of frightening. Is a splenectomy really a What is the spleen? wise choice? The spleen is a small organ (normally That’s a decision that must be made in each individual case. about the size of a fist) that lies in the A doctor with significant experience with thalassemia is upper left part of the abdomen, near going to be in the best position to offer advice about this; the stomach and below the ribcage. however, most people who are splenectomized are able to What does it do? manage the challenges it presents with relatively little The spleen has a number of functions, the most important of difficulty. which are filtering blood and creating lymphocytes. It also acts as a “reservoir” of blood, keeping a certain amount on Of course, it’s best to avoid any circumstances that can lead hand for use in emergencies. to the need for a splenectomy in the first place. For a person with thalassemia, this means following a transfusion In its filtering capacity, the spleen is able to remove large regimen that keeps hemoglobin levels above 9 or 10gm/dL. -

Health Tip: Swollen Lymph "Glands" - When Should You Be Concerned?
Printer Friendly Version Page 1 of 3 Health Tip: Swollen lymph "glands" - When should you be concerned? Lymph nodes, sometimes referred to as lymph "glands", are part of the body's lymphatic system. The lymphatic system consists of a system of conduits and organized collections of lymphoid tissue that include nodes, the tonsils, and the spleen. Coursing through these channels is liquid called lymph that eventually drains into the bloodstream near the heart, but along the way, it is "filtered" by the lymph nodes. Within these lymph nodes are high concentrations of disease fighting cells, particularly lymphocytes. While performing their intended function of fighting infection, lymph nodes typically become enlarged. In fact, infection is most common reason for lymph nodes enlargement. Lymph nodes are found throughout the body, but when enlarged, are usually noticed in characteristic locations, particularly the neck, groin and armpit regions. Lymph node enlargement can be localized to one group of lymph nodes or can be generalized (involving several sites of lymph nodes). For example, enlarged lymph nodes localized to the arm pit could occur as a result of a bacterial infection in a hand wound. Generalized lymph node swelling, on the other hand, could be seen in a systemic illness such as viral mononucleosis. In addition to viral and bacterial infections, other causes for enlarged lymph nodes include immune disorders (lupus, rheumatoid arthritis, etc.), cancers affecting the lymphatic system (leukemia, lymphoma, Hodgkin's disease), and cancers that have spread (metastasized) from some other part of the body to the lymphatic system. The discovery of enlarged lymph nodes often causes concern because many people are aware that lymph node enlargement can be an early sign of cancer. -

29 Assessing the Cardiovascular and Lymphatic Systems
29 Assessing the Cardiovascular and Lymphatic Systems LEARNING OUTCOMES 1. Describe the anatomy, physiology, and functions of the 5. Explain techniques used to assess cardiovascular and cardiovascular and lymphatic systems. lymphatic structure and function. 2. Describe normal variations in cardiovascular assessment 6. Identify manifestations of impaired cardiovascular structure findings for the older adult. and functions. 3. Give examples of genetic disorders of the cardiovascular system. 4. Identify specific topics for consideration during a health history assessment interview of the patient with cardiovascu- lar or lymphatic disorders. CLINICAL COMPETENCIES 1. Complete a health history for patients having alterations in 3. Assess an ECG strip and identify normal rhythm and cardiac the structure and functions of the cardiovascular or lymphatic events and abnormal cardiac rhythm. systems. 4. Monitor the results of diagnostic tests and communicate 2. Conduct and document a physical assessment of cardiovas- abnormal findings within the interprofessional team. cular and lymphatic status. MAJOR CHAPTER CONCEPTS • Correct structure and function of the cardiovascular and • Manifestations of dysfunction, injury, and disorders affecting lymphatic systems are vital to the transport of oxygen and the cardiovascular and lymphatic systems may be detected carbon dioxide throughout the body and for the return of during a general health assessment as well as during focused excess tissue fluids back to the bloodstream. cardiovascular and lymphatic system -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Osteopathic Approach to the Spleen
Osteopathic approach to the spleen Luc Peeters and Grégoire Lason 1. Introduction the first 3 years to 4 - 6 times the birth size. The position therefore progressively becomes more lateral in place of The spleen is an organ that is all too often neglected in the original epigastric position. The spleen is found pos- the clinic, most likely because conditions of the spleen do tero-latero-superior from the stomach, its arterial supply is not tend to present a defined clinical picture. Furthermore, via the splenic artery and the left gastroepiploic artery it has long been thought that the spleen, like the tonsils, is (Figure 2). The venous drainage is via the splenic vein an organ that is superfluous in the adult. into the portal vein (Figure 2). The spleen is actually the largest lymphoid organ in the body and is implicated within the blood circulation. In the foetus it is an organ involved in haematogenesis while in the adult it produces lymphocytes. The spleen is for the blood what the lymph nodes are for the lymphatic system. The spleen also purifies and filters the blood by removing dead cells and foreign materials out of the circulation The function of red blood cell reserve is also essential for the maintenance of human activity. Osteopaths often identify splenic congestion under the influence of poor diaphragm function. Some of the symptoms that can be associated with dysfunction of the spleen are: Figure 2 – Position and vascularisation of the spleen Anaemia in children Disorders of blood development Gingivitis, painful and bleeding gums Swollen, painful tongue, dysphagia and glossitis Fatigue, hyperirritability and restlessness due to the anaemia Vertigo and tinnitus Frequent colds and infections due to decreased resis- tance Thrombocytosis Tension headaches The spleen is also considered an important organ by the osteopath as it plays a role in the immunity, the reaction of the circulation and oxygen transport during effort as well as in regulation of the blood pressure. -

In Sickness and in Health: the Immunological Roles of the Lymphatic System
International Journal of Molecular Sciences Review In Sickness and in Health: The Immunological Roles of the Lymphatic System Louise A. Johnson MRC Human Immunology Unit, MRC Weatherall Institute of Molecular Medicine, University of Oxford, John Radcliffe Hospital, Headington, Oxford OX3 9DS, UK; [email protected] Abstract: The lymphatic system plays crucial roles in immunity far beyond those of simply providing conduits for leukocytes and antigens in lymph fluid. Endothelial cells within this vasculature are dis- tinct and highly specialized to perform roles based upon their location. Afferent lymphatic capillaries have unique intercellular junctions for efficient uptake of fluid and macromolecules, while expressing chemotactic and adhesion molecules that permit selective trafficking of specific immune cell subsets. Moreover, in response to events within peripheral tissue such as inflammation or infection, soluble factors from lymphatic endothelial cells exert “remote control” to modulate leukocyte migration across high endothelial venules from the blood to lymph nodes draining the tissue. These immune hubs are highly organized and perfectly arrayed to survey antigens from peripheral tissue while optimizing encounters between antigen-presenting cells and cognate lymphocytes. Furthermore, subsets of lymphatic endothelial cells exhibit differences in gene expression relating to specific func- tions and locality within the lymph node, facilitating both innate and acquired immune responses through antigen presentation, lymph node remodeling and regulation of leukocyte entry and exit. This review details the immune cell subsets in afferent and efferent lymph, and explores the mech- anisms by which endothelial cells of the lymphatic system regulate such trafficking, for immune surveillance and tolerance during steady-state conditions, and in response to infection, acute and Citation: Johnson, L.A. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases
microorganisms Review Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases Juan Alberto Lira-Lucio 1 , Ramcés Falfán-Valencia 1 , Alejandra Ramírez-Venegas 2, Ivette Buendía-Roldán 3 , Jorge Rojas-Serrano 4 , Mayra Mejía 4 and Gloria Pérez-Rubio 1,* 1 HLA Laboratory, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.A.L.-L.); [email protected] (R.F.-V.) 2 Tobacco Smoking and COPD Research Department, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 3 Translational Research Laboratory on Aging and Pulmonary Fibrosis, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 4 Interstitial Lung Disease and Rheumatology Unit, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.R.-S.); [email protected] (M.M.) * Correspondence: [email protected]; Tel.: +52-55-5487-1700 (ext. 5152) Received: 11 June 2020; Accepted: 7 July 2020; Published: 16 July 2020 Abstract: The lung microbiome composition has critical implications in the regulation of innate and adaptive immune responses. Next-generation sequencing techniques have revolutionized the understanding of pulmonary physiology and pathology. Currently, it is clear that the lung is not a sterile place; therefore, the investigation of the participation of the pulmonary microbiome in the presentation, severity, and prognosis of multiple pathologies, such as asthma, chronic obstructive pulmonary disease, and interstitial lung diseases, contributes to a better understanding of the pathophysiology. Dysregulation of microbiota components in the microbiome–host interaction is associated with multiple lung pathologies, severity, and prognosis, making microbiome study a useful tool for the identification of potential therapeutic strategies. -
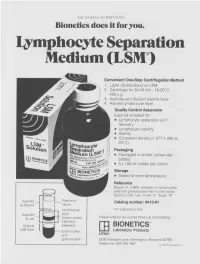
Lymphocyte Separation Medium (LSM
THE JOURNAL OF IMMUNOLOGY Bionetics does it for you. Lymphocyte Separation Medium (LSM wenient One-Step Centrifugation Method _ayer diluted blood on LSM. 2,entrifuge for 30-40 min., 18-20°C, ~.00 x g. ~,spirate and discard plasma layer -larvest lymphocyte layer. Quality Control Assurance Each lot is tested for: • Lymphocyte separation and recovery. • Lymphocyte viability. • Sterility. • Consistent density (1.077-1.080 at 20°C). Packaging • Packaged in amber, screw-cap bottles. • 5 x 100 ml bottles per carton. Storage. • Stored at room temperature. Reference Boyum, A. (1968): Isolation of mononuclear cells and granulocytes from human blood. Scand J. Clin. Lab. Invest. 21, Suppl. 97. Aspirate I IC[OI I IC~ LJI Catalog number: 8410-01 & discard serum Lymphocyte For Laboratory Use Aspirate layer & use (mononuclear Please write for our current Price List and Catalog. cells and Original platelets) ITi BIONETICS° LSM layer Erythrocytes Laboratory Products and Litton granulocytes 5516 Nicholson Lane, Kensington, Maryland 20795 Telephone: (301) 881-1557 1979 Litton Bionetics, tnc Get the most out of your high quality cytotoxic antibodies with LOW-TOX-M RABBIT COMPLEMENT LOW TOXICITY HIGH ACTIVITY Presentation: CL 3051 5 x 1 ml, lyophilized $30.00 When it comes to COMPLEMENT... come to CEDARLANE Direct orders or inquiries to: UNITED STATES: WORLDWIDE EXCEPT U.S. ,4 C~L CEDARLANE ACCURATE CHEMICAL & LABORATO RI ES SCIENTIFIC CORPORATION LIMITED 5516-8TH LINE, R.R. 2 28 TEC STREET, HICKSVtLLE, N.Y. 11801 HORNBY, ONTARIO, CANADA LOP 1E0 Telephone -

Stress and the Immune System Tracy B
4 World Health • 47th Yeor, No. 2, Morch-Aprill994 Stress and the immune system Tracy B. Herbert any people have the effects of factors as diverse as experienced the examinations, bereavement, divorce, Mconnection between stress unemployment, mental arithmetic, and getting sick. Colds, influenza, and looking after a relative with herpes and allergies seem worse Alzheimer's di sease. In general, when we are severely stressed at these studies find that stress is work or in the home. Others are related to changes in both the never sick until they go on vacation numbers of white blood cells in (that is, after the stress is over), and circulation and the quantity of then they spend the whole time antibody in the blood. Moreover, fighting the virus. Because of stress is associated with changes in intrinsic connections like these, the functioning of immune cells. many researchers are today That is, there is a relatively large exploring whether (and how) stress decrease in both lymphocyte and illness are actually linked. One proliferation and natural killer cell specific focus of this research is to activity in individuals who have study the effects of stress on the experienced stress. There seems to immune systems; after all, if stress A lymphocyte: stress may weaken the capacity be some connection between the affects immunity, that would be one of lymphocytes to combat infection. duration of the stress and the amount way in which stress could contribute of immune change. For example, the to illness. longer the stress, the greater the The function of the immune proliferation"- by incubating these decrease in the number of specific system is to protect us from cells for several days with types of white blood cells. -

Cells, Tissues and Organs of the Immune System
Immune Cells and Organs Bonnie Hylander, Ph.D. Aug 29, 2014 Dept of Immunology [email protected] Immune system Purpose/function? • First line of defense= epithelial integrity= skin, mucosal surfaces • Defense against pathogens – Inside cells= kill the infected cell (Viruses) – Systemic= kill- Bacteria, Fungi, Parasites • Two phases of response – Handle the acute infection, keep it from spreading – Prevent future infections We didn’t know…. • What triggers innate immunity- • What mediates communication between innate and adaptive immunity- Bruce A. Beutler Jules A. Hoffmann Ralph M. Steinman Jules A. Hoffmann Bruce A. Beutler Ralph M. Steinman 1996 (fruit flies) 1998 (mice) 1973 Discovered receptor proteins that can Discovered dendritic recognize bacteria and other microorganisms cells “the conductors of as they enter the body, and activate the first the immune system”. line of defense in the immune system, known DC’s activate T-cells as innate immunity. The Immune System “Although the lymphoid system consists of various separate tissues and organs, it functions as a single entity. This is mainly because its principal cellular constituents, lymphocytes, are intrinsically mobile and continuously recirculate in large number between the blood and the lymph by way of the secondary lymphoid tissues… where antigens and antigen-presenting cells are selectively localized.” -Masayuki, Nat Rev Immuno. May 2004 Not all who wander are lost….. Tolkien Lord of the Rings …..some are searching Overview of the Immune System Immune System • Cells – Innate response- several cell types – Adaptive (specific) response- lymphocytes • Organs – Primary where lymphocytes develop/mature – Secondary where mature lymphocytes and antigen presenting cells interact to initiate a specific immune response • Circulatory system- blood • Lymphatic system- lymph Cells= Leukocytes= white blood cells Plasma- with anticoagulant Granulocytes Serum- after coagulation 1.