Lymphocyte-Activation Gene 3 (LAG-3) Immune Pathway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ENSG Gene Encodes Effector TCR Pathway Costimulation Inhibitory/Exhaustion Synapse/Adhesion Chemokines/Receptors
ENSG Gene Encodes Effector TCR pathway Costimulation Inhibitory/exhaustion Synapse/adhesion Chemokines/receptors ENSG00000111537 IFNG IFNg x ENSG00000109471 IL2 IL-2 x ENSG00000232810 TNF TNFa x ENSG00000271503 CCL5 CCL5 x x ENSG00000139187 KLRG1 Klrg1 x ENSG00000117560 FASLG Fas ligand x ENSG00000121858 TNFSF10 TRAIL x ENSG00000134545 KLRC1 Klrc1 / NKG2A x ENSG00000213809 KLRK1 Klrk1 / NKG2D x ENSG00000188389 PDCD1 PD-1 x x ENSG00000117281 CD160 CD160 x x ENSG00000134460 IL2RA IL-2 receptor x subunit alpha ENSG00000110324 IL10RA IL-10 receptor x subunit alpha ENSG00000115604 IL18R1 IL-18 receptor 1 x ENSG00000115607 IL18RAP IL-18 receptor x accessory protein ENSG00000081985 IL12RB2 IL-12 receptor x beta 2 ENSG00000186810 CXCR3 CXCR3 x x ENSG00000005844 ITGAL CD11a x ENSG00000160255 ITGB2 CD18; Integrin x x beta-2 ENSG00000156886 ITGAD CD11d x ENSG00000140678 ITGAX; CD11c x x Integrin alpha-X ENSG00000115232 ITGA4 CD49d; Integrin x x alpha-4 ENSG00000169896 ITGAM CD11b; Integrin x x alpha-M ENSG00000138378 STAT4 Stat4 x ENSG00000115415 STAT1 Stat1 x ENSG00000170581 STAT2 Stat2 x ENSG00000126561 STAT5a Stat5a x ENSG00000162434 JAK1 Jak1 x ENSG00000100453 GZMB Granzyme B x ENSG00000145649 GZMA Granzyme A x ENSG00000180644 PRF1 Perforin 1 x ENSG00000115523 GNLY Granulysin x ENSG00000100450 GZMH Granzyme H x ENSG00000113088 GZMK Granzyme K x ENSG00000057657 PRDM1 Blimp-1 x ENSG00000073861 TBX21 T-bet x ENSG00000115738 ID2 ID2 x ENSG00000176083 ZNF683 Hobit x ENSG00000137265 IRF4 Interferon x regulatory factor 4 ENSG00000140968 IRF8 Interferon -

A1068-CD86 Polyclonal Antibody
BioVision 05/16 For research use only CD86 Polyclonal Antibody CATALOG NO: A1068-100 ALTERNATIVE NAMES: T-lymphocyte activation antigen CD86, Activation B7-2 antigen, B70, BU63, CTLA-4 counter-receptor B72, FUN-1, CD86, CD86, CD28LG2 Western blot analysis of CD86 in NCI-H292 cell line lysate AMOUNT: 100 µl IMMUNOGEN: KLH conjugated synthetic peptide between 269-298 amino acids from the C-terminal region of human CD86. MOLECULAR WEIGHT: 37 kDa HOST/ISOTYPE: Rabbit IgG SPECIES REACTIVITY: Human PURIFICATION: This antibody is purified through a protein A column, followed by peptide affinity purification. FORM: Liquid FORMULATION: Supplied in PBS with 0.09% (W/V) sodium azide. STORAGE CONDITIONS: Maintain refrigerated at 2-8°C for up to 6 months. For long term RELATED PRODUCTS storage store at -20°C in small aliquots to prevent freeze-thaw cycles. DESCRIPTION: This gene encodes a type I membrane protein that is a member of the immunoglobulin superfamily. This protein is expressed by Human CellExp™ B7-2 /CD86, human recombinant (Cat. No. 7496-10, -50) antigen-presenting cells, and it is the ligand for two proteins at the CD86 (Human) ELISA Kit (Cat. No. K4175-100) cell surface of T cells, CD28 antigen and cytotoxic T-lymphocyte- Human CellExp™LAG3 /CD223, human recombinant (Cat. No. 7278-10, -50) associated protein 4. Binding of this protein with CD28 antigen is a costimulatory signal for activation of the T-cell. Binding of this CD223 (LAG3) Polyclonal Antibody (Cat. No. A1067-100) protein with cytotoxic T-lymphocyte-associated protein 4 negatively regulates T-cell activation and diminishes the immune response. -

Selectins in Cancer Immunity
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2018 Selectins in cancer immunity Borsig, Lubor Abstract: Selectins are vascular adhesion molecules that mediate physiological responses such as inflam- mation, immunity and hemostasis. During cancer progression, selectins promote various steps enabling the interactions between tumor cells and the blood constituents, including platelets, endothelial cells and leukocytes. Selectins are carbohydrate-binding molecules that bind to sialylated, fucosylated glycan structures. The increased selectin ligand expression on tumor cells correlates with enhanced metastasis and poor prognosis for cancer patients. While, many studies focused on the role of selectin as a mediator of tumor cell adhesion and extravasation during metastasis, there is evidence for selectins to activate signaling cascade that regulates immune responses within a tumor microenvironment. L-Selectin binding induces activation of leukocytes, which can be further modulated by selectin-mediated interactions with platelets and endothelial cells. Selectin ligand on leukocytes, PSGL-1, triggers intracellular signaling in leukocytes that are induced through platelet’s P-selectin or endothelial E-selectin binding. In this review, I summarize the evidence for selectin-induced immune modulation in cancer progression that represents a possible target for controlling tumor immunity. DOI: https://doi.org/10.1093/glycob/cwx105 Posted at the Zurich Open Repository and -

Molecular and Clinical Characterization of LAG3 in Breast Cancer Through 2994 Samples
Molecular and Clinical Characterization of LAG3 in Breast Cancer Through 2994 Samples Qiang Liu Chinese Academy of Medical Sciences & Peking Union Medical College Yihang Qi ( [email protected] ) Chinese Academy of Medical Sciences and Peking Union Medical College https://orcid.org/0000-0001- 7589-0333 Jie Zhai Chinese Academy of Medical Sciences & Peking Union Medical College Xiangyi Kong Chinese Academy of Medical Sciences & Peking Union Medical College Xiangyu Wang Chinese Academy of Medical Sciences & Peking Union Medical College Yi Fang Chinese Academy of Medical Sciences & Peking Union Medical College Jing Wang Chinese Academy of Medical Sciences & Peking Union Medical College Research Keywords: Cancer immunotherapy, CD223, LAG3, Immune response, Inammatory activity Posted Date: June 19th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-36422/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/33 Abstract Background Despite the promising impact of cancer immunotherapy targeting CTLA4 and PD1/PDL1, a large number of cancer patients fail to respond. LAG3 (Lymphocyte Activating 3), also named CD233, is a protein Coding gene served as alternative inhibitory receptors to be targeted in the clinic. The impact of LAG3 on immune cell populations and co-regulation of immune response in breast cancer remained largely unknown. Methods To characterize the role of LAG3 in breast cancer, we investigated transcriptome data and associated clinical information derived from a total of 2994 breast cancer patients. Results We observed that LAG3 was closely correlated with major molecular and clinical characteristics, and was more likely to be enriched in higher malignant subtype, suggesting LAG3 was a potential biomarker of triple-negative breast cancer. -

Diabetes in the Absence of LAG-3 Cutting Edge
Cutting Edge: Accelerated Autoimmune Diabetes in the Absence of LAG-3 Maria Bettini, Andrea L. Szymczak-Workman, Karen Forbes, Ashley H. Castellaw, Mark Selby, Xiaoyu Pan, This information is current as Charles G. Drake, Alan J. Korman and Dario A. A. Vignali of September 24, 2021. J Immunol 2011; 187:3493-3498; Prepublished online 26 August 2011; doi: 10.4049/jimmunol.1100714 http://www.jimmunol.org/content/187/7/3493 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2011/08/26/jimmunol.110071 Material 4.DC1 http://www.jimmunol.org/ References This article cites 25 articles, 11 of which you can access for free at: http://www.jimmunol.org/content/187/7/3493.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 24, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Cutting Edge: Accelerated Autoimmune Diabetes in the Absence of LAG-3 Maria Bettini,* Andrea L. -

5.01.591 Immune Checkpoint Inhibitors
MEDICAL POLICY – 5.01.591 Immune Checkpoint Inhibitors Effective Date: Sept. 1, 2021 RELATED POLICIES/GUIDELINES: Last Revised: Aug. 10, 2021 5.01.543 General Medical Necessity Criteria for Companion Diagnostics Related Replaces: N/A to Drug Approval 5.01.589 BRAF and MEK Inhibitors Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Chemotherapy, often called chemo, is cancer treatment that uses drugs. Radiation and surgery treat one area of cancer. But chemo usually travels through the bloodstream to treat the whole body. Treating the whole body is called a systemic treatment. Immunotherapy is a new type of cancer treatment that helps the body’s immune cells fight the cancer more effectively. Cancer cells sometimes “hide” from the body’s cells that are designed to search for cells that don’t belong, like cancer cells or bacteria. Immune checkpoint inhibitors are drugs that block the way that cancer cells do this and so help the immune cells find them so they can be stopped. It is one of the ways we can make the environment less friendly to the cancer and slow its growth. Current immunotherapy drugs are complex molecules that must be given through a vein (intravenous). In the future, some may be given by a shot (injection) the patient could inject without help. This policy gives information about immunotherapy drugs and the criteria for when they may be medically necessary. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. -

Point Mutation in CD19 Facilitates Immune Escape of B Cell Lymphoma from CAR-T Cell Therapy
Open access Original research J Immunother Cancer: first published as 10.1136/jitc-2020-001150 on 6 October 2020. Downloaded from Point mutation in CD19 facilitates immune escape of B cell lymphoma from CAR- T cell therapy 1 1 1 1 1 1 Zhen Zhang, Xinfeng Chen, Yonggui Tian, Feng Li , Xuan Zhao, Jinyan Liu, 1 1,2,3,4 Chang Yao, Yi Zhang To cite: Zhang Z, Chen X, ABSTRACT relapses after CD19 CAR-T cell therapy are Tian Y, et al. Point mutation Background Tumor relapse due to mutation in CD19 can attributed to the antigen loss, indicating an in CD19 facilitates immune hinder the efficacy of chimeric antigen receptor (CAR)- T urgent need for investigating the mechanisms escape of B cell lymphoma from cell therapy. Herein, we focused on lymphoma patients CAR- T cell therapy. Journal underlying recurrence and for improving whose B cells exhibited a point mutation in CD19 of B cells 4 5 for ImmunoTherapy of Cancer the efficacy of CAR- T cell therapy. Inter- 2020; :e001150. doi:10.1136/ after CAR-T cell infusion. 8 + estingly, one of the specific mechanisms jitc-2020-001150 Methods The CAR- T and CD19 B cells from peripheral blood or bone marrow were assessed using flow of tumor escape that has been reported cytometry. Genome sequencing was conducted to identify suggests that exon mutations affecting the ► Additional material is + published online only. To view, the molecular characteristics of CAR- T and CD19 B cells CD19 gene and its splicing isoforms, leading please visit the journal online from pre-rela pse and postrelapse samples. -

LAG-3: from Molecular Functions to Clinical Applications
Open access Review J Immunother Cancer: first published as 10.1136/jitc-2020-001014 on 13 September 2020. Downloaded from LAG-3: from molecular functions to clinical applications Takumi Maruhashi , Daisuke Sugiura , Il- mi Okazaki , Taku Okazaki To cite: Maruhashi T, Sugiura D, ABSTRACT (PD-1) and cytotoxic T lymphocyte antigen Okazaki I, et al. LAG-3: from To prevent the destruction of tissues owing to excessive 4 (CTLA-4) significantly improved the molecular functions to clinical and/or inappropriate immune responses, immune outcomes of patients with diverse cancer applications. Journal for cells are under strict check by various regulatory ImmunoTherapy of Cancer types, revolutionizing cancer treatment. The mechanisms at multiple points. Inhibitory coreceptors, 2020;8:e001014. doi:10.1136/ success of these therapies verified that inhib- including programmed cell death 1 (PD-1) and cytotoxic jitc-2020-001014 itory coreceptors serve as critical checkpoints T lymphocyte antigen 4 (CTLA-4), serve as critical checkpoints in restricting immune responses against for immune cells to not attack the tumor Accepted 29 July 2020 self- tissues and tumor cells. Immune checkpoint inhibitors cells as well as self-tissues. However, response that block PD-1 and CTLA-4 pathways significantly rates are typically lower and immune-related improved the outcomes of patients with diverse cancer adverse events (irAEs) are also observed in types and have revolutionized cancer treatment. However, patients administered with immune check- response rates to such therapies are rather limited, and point inhibitors. This is indicative of the immune-rela ted adverse events are also observed in a continued need to decipher the complex substantial patient population, leading to the urgent need biology of inhibitory coreceptors to increase for novel therapeutics with higher efficacy and lower response rates and prevent such unwanted toxicity. -

Fundamental Mechanisms of Immune Checkpoint Blockade Therapy
Published OnlineFirst August 16, 2018; DOI: 10.1158/2159-8290.CD-18-0367 REVIEW Fundamental Mechanisms of Immune Checkpoint Blockade Therapy Spencer C. Wei 1 , Colm R. Duffy 1 , and James P. Allison 1 , 2 ABSTRACT Immune checkpoint blockade is able to induce durable responses across multiple types of cancer, which has enabled the oncology community to begin to envision potentially curative therapeutic approaches. However, the remarkable responses to immunotherapies are currently limited to a minority of patients and indications, highlighting the need for more effec- tive and novel approaches. Indeed, an extraordinary amount of preclinical and clinical investigation is exploring the therapeutic potential of negative and positive costimulatory molecules. Insights into the underlying biological mechanisms and functions of these molecules have, however, lagged signifi cantly behind. Such understanding will be essential for the rational design of next-generation immunothera- pies. Here, we review the current state of our understanding of T-cell costimulatory mechanisms and checkpoint blockade, primarily of CTLA4 and PD-1, and highlight conceptual gaps in knowledge. signifi cance: This review provides an overview of immune checkpoint blockade therapy from a basic biology and immunologic perspective for the cancer research community. Cancer Discov; 8(9); 1–18. ©2018 AACR. INTRODUCTION dogma and recent conceptual advances related to the mecha- nisms of action of anti–PD-1 and anti-CTLA4 therapies Immune checkpoint blockade therapies are now FDA in the context of antitumor immunity. These discussions approved for the treatment of a broad range of tumor types highlight the importance of understanding the underlying ( Table 1 ), with approval likely for additional indications fundamental biological phenomena for effective transla- in the near future. -
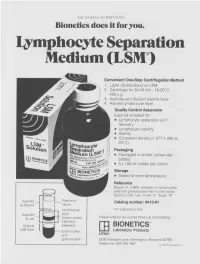
Lymphocyte Separation Medium (LSM
THE JOURNAL OF IMMUNOLOGY Bionetics does it for you. Lymphocyte Separation Medium (LSM wenient One-Step Centrifugation Method _ayer diluted blood on LSM. 2,entrifuge for 30-40 min., 18-20°C, ~.00 x g. ~,spirate and discard plasma layer -larvest lymphocyte layer. Quality Control Assurance Each lot is tested for: • Lymphocyte separation and recovery. • Lymphocyte viability. • Sterility. • Consistent density (1.077-1.080 at 20°C). Packaging • Packaged in amber, screw-cap bottles. • 5 x 100 ml bottles per carton. Storage. • Stored at room temperature. Reference Boyum, A. (1968): Isolation of mononuclear cells and granulocytes from human blood. Scand J. Clin. Lab. Invest. 21, Suppl. 97. Aspirate I IC[OI I IC~ LJI Catalog number: 8410-01 & discard serum Lymphocyte For Laboratory Use Aspirate layer & use (mononuclear Please write for our current Price List and Catalog. cells and Original platelets) ITi BIONETICS° LSM layer Erythrocytes Laboratory Products and Litton granulocytes 5516 Nicholson Lane, Kensington, Maryland 20795 Telephone: (301) 881-1557 1979 Litton Bionetics, tnc Get the most out of your high quality cytotoxic antibodies with LOW-TOX-M RABBIT COMPLEMENT LOW TOXICITY HIGH ACTIVITY Presentation: CL 3051 5 x 1 ml, lyophilized $30.00 When it comes to COMPLEMENT... come to CEDARLANE Direct orders or inquiries to: UNITED STATES: WORLDWIDE EXCEPT U.S. ,4 C~L CEDARLANE ACCURATE CHEMICAL & LABORATO RI ES SCIENTIFIC CORPORATION LIMITED 5516-8TH LINE, R.R. 2 28 TEC STREET, HICKSVtLLE, N.Y. 11801 HORNBY, ONTARIO, CANADA LOP 1E0 Telephone -

Stress and the Immune System Tracy B
4 World Health • 47th Yeor, No. 2, Morch-Aprill994 Stress and the immune system Tracy B. Herbert any people have the effects of factors as diverse as experienced the examinations, bereavement, divorce, Mconnection between stress unemployment, mental arithmetic, and getting sick. Colds, influenza, and looking after a relative with herpes and allergies seem worse Alzheimer's di sease. In general, when we are severely stressed at these studies find that stress is work or in the home. Others are related to changes in both the never sick until they go on vacation numbers of white blood cells in (that is, after the stress is over), and circulation and the quantity of then they spend the whole time antibody in the blood. Moreover, fighting the virus. Because of stress is associated with changes in intrinsic connections like these, the functioning of immune cells. many researchers are today That is, there is a relatively large exploring whether (and how) stress decrease in both lymphocyte and illness are actually linked. One proliferation and natural killer cell specific focus of this research is to activity in individuals who have study the effects of stress on the experienced stress. There seems to immune systems; after all, if stress A lymphocyte: stress may weaken the capacity be some connection between the affects immunity, that would be one of lymphocytes to combat infection. duration of the stress and the amount way in which stress could contribute of immune change. For example, the to illness. longer the stress, the greater the The function of the immune proliferation"- by incubating these decrease in the number of specific system is to protect us from cells for several days with types of white blood cells. -

Coordination of T Cell Activation and Migration Through Formation of the Immunological Synapse
Coordination of T Cell Activation and Migration through Formation of the Immunological Synapse MICHAEL L. DUSTIN Program in Molecular Pathogenesis, Skirball Institute of Biomolecular Medicine and the Department of Pathology, New York University School of Medicine, New York, New York 10016, USA ABSTRACT: T cell activation is based on interactions of T cell antigen receptors with MHC-peptide complexes in a specialized cell–cell junction between the T cell and antigen-presenting cell—the immunological synapse. The immunolog- ical synapse coordinates naïve T cell activation and migration by stopping T cell migration with antigen-presenting cells bearing appropriate major histo- compatibility complex (MHC) peptide complexes. At the same time, the immu- nological synapse allows full T cell activation through sustained signaling over a period of several hours. The immunological synapse supports activation in the absence of continued T cell migration, which is required for T cell activa- tion through serial encounters. Src and Syk family kinases are activated early in immunological synapse formation, but this signaling process returns to the basal level after 30 min; at the same time, the interactions between T cell re- ceptors (TCRs) and MHC peptides are stabilized within the immunological synapse. The molecular pattern of the mature synapse in helper T cells is a self- stabilized structure that is correlated with cytokine production and prolifera- tion. I propose that this molecular pattern and its specific biochemical constit- uents are necessary