Nutrition Reference Man
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
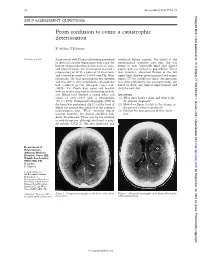
From Confusion to Coma: a Catastrophic Deterioration
52 Postgrad Med J 2001;77:52–55 Postgrad Med J: first published as 10.1136/pmj.77.903.53a on 1 January 2001. Downloaded from SELF ASSESSMENT QUESTIONS From confusion to coma: a catastrophic deterioration K Ashkan, F Johnston Answers on p 56. A previously well 45 year old woman presented ventilated before transfer. On arrival at the to the local casualty department with a one day neurosurgical intensive care unit, she was history of generalised headache, neck stiVness, found to have bilaterally fixed and dilated and blurred vision. On examination she had a pupils, with no corneal or gag reflexes. There temperature of 38°C, a pulse of 80 beats/min, was, however, abnormal flexion of the left and a blood pressure of 130/80 mm Hg. Neu- upper limb. She was given mannitol and urgent rologically, she had spontaneous eye opening repeat CT was carried out (fig 2). An operation and was able to obey commands, although she was then performed, but postoperatively she had confused speech (Glasgow coma scale failed to show any clinical improvement and (GCS), 14). Pupils were equal and reactive died the next day. with no cranial or peripheral neurological defi- cits. Blood tests showed a raised white cell Questions count of 20.9 × 109/l with a neutrophilia (1) What does figure 1 show and what is the (19.2 × 109/l). Computed tomography (CT) of diVerential diagnosis? the brain was performed (fig 1), on the basis of (2) How does figure 2 relate to the change in which the patient was referred to the regional the patient’s clinical condition? neurosurgical unit. -
Hypervitaminosis - an Emerging Pathological Condition
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Review Article Hypervitaminosis - An Emerging Pathological Condition J K Roop PG Department of Zoology, JC DAV College (Affiliated to Panjab University, Chandigarh), Dasuya-144205, District Hoshiarpur, Punjab, India ABSTRACT Vitamins are essential organic compounds that are required in small amounts to regulate various metabolic activities in the body. Prolonged and overconsumption of pharmaceutical forms of both water-soluble and fat-soluble vitamins may lead to toxicity and/or hypervitaminosis. Hypervitaminosis is an acute emerging pathological condition of the body due to excess accumulation of any of the vitamins. In case of acute poisoning with vitamin supplements/drugs, emergency assistance is required to detoxify the effects and restore the organization, structure and function of body’s tissues and organs. Sometimes death may occur due to intoxication to liver, kidney and heart. So, to manage any type of hypervitaminosis, proper diagnosis is essential to initiate eliminating the cause of its occurrence and accelerate the elimination of the supplement from the body. The present review discusses the symptoms of hypervitaminosis that seems to be a matter of concern today and management strategies to overcome toxicity or hypervitaminosis. Keywords: Hypervitaminosis, Toxicity, Vitamins, Vitamin pathology, Fat-soluble vitamin, Water- soluble vitamin. INTRODUCTION body, particularly in the liver. Vitamin B Vitamins are potent organic Complex and vitamin C are water- soluble. compounds present in small concentrations They are dissolved easily in food during in various fruits and vegetables. They cooking and a portion of these vitamins may regulate physiological functions and help in be destroyed by heating. -

The Practice and Regulatory Requirements Of
School of Public Health The Practice and Regulatory Requirements of Naturopathy and Western Herbal Medicine Vivian Lin Alan Bensoussan Stephen P. Myers Pauline McCabe Marc Cohen Sophie Hill Genevieve Howse November, 2005 Funded by the Department of Human Services, Victoria Copyright State of Victoria, Department of Human Services, 2006 This publication is copyright. No part may be reproduced by any process except in accordance with the provisions of the Copyright Act 1968 (Cth). Authorised by the State Government of Victoria, 50 Lonsdale Street Melbourne. This document may be downloaded from the following website: www.health.vic.gov.au/pracreg/naturopathy.htm ISBN-13: 978-0-9775864-0-0 ISBN-10: 0-9775864-0-5 Published by School of Public Health, La Trobe University Bundoora Victoria, 3086 Australia THE PRACTICE AND REGULATORY REQUIREMENTS OF NATUROPATHY AND WESTERN HERBAL MEDICINE CONTENTS VOLUME ONE Summary Report..........................................................................................................1 1. Introduction.......................................................................................................1 2. Methodology.....................................................................................................1 3. Key findings and recommendations..................................................................2 3.1 Definition of practice and scope of study ........................................................2 3.2 Growing use of naturopathy and WHM...........................................................3 -

Hepatic Pathology in Vitamin a Toxicity FAIRPOUR FOROUHAR, M.D.* MARTIN S
ANNALS OF CLINICAL AND LABORATORY SCIENCE, Vol. 14, No. 4 Copyright © 1984, Institute for Clinical Science, Inc. Hepatic Pathology in Vitamin A Toxicity FAIRPOUR FOROUHAR, M.D.* MARTIN S. NADEL, M.D.,t and BERNARD GONDOS, M.D.* *Department of Pathology, University of Connecticut, Farmington, CT 06032 and fDepartment of Pathology, Middlesex Memorial Hospital, Middletown, CT 06457 ABSTRACT This paper documents a case of vitamin A toxicity presenting with splenomegaly and ascites. The light microscopic, electron microscopic, and fluorescent findings are described in detail. The principal histopath ologic finding was marked perisinusoidal fibrosis. The role of Ito cells in the storage of lipid-soluble vitamins and their subsequent transformation to fibroblasts producing collagen are discussed. tient denied use of medications but admitted long Introduction time use of a self-prescribed vitamin B1-B6 combi nation, vitamin B12, iodine, and garlic. Vitamin A Liver disease resulting from vitamin A had been taken for six years, initially 75,000 units toxicity is an uncommon but well docu daily, increased to 150,000 units daily two years prior to admission because of believed problems with night mented entity.6’1414’22’26,27 The present vision for which no medical help had been sought. case provides a good model for the study Physical examination disclosed no palpable spleno of fibrosis of the space of Disse and its megaly with liver felt one cm beneath the right costal margin. An abdominal fluid wave was present. No pathophysiologic ^consequences. Similar spider angiomata were noted, and the remainder of changes also occur in other conditions re the physical examination was unremarkable. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Nutrition Journal of Parenteral and Enteral
Journal of Parenteral and Enteral Nutrition http://pen.sagepub.com/ Micronutrient Supplementation in Adult Nutrition Therapy: Practical Considerations Krishnan Sriram and Vassyl A. Lonchyna JPEN J Parenter Enteral Nutr 2009 33: 548 originally published online 19 May 2009 DOI: 10.1177/0148607108328470 The online version of this article can be found at: http://pen.sagepub.com/content/33/5/548 Published by: http://www.sagepublications.com On behalf of: The American Society for Parenteral & Enteral Nutrition Additional services and information for Journal of Parenteral and Enteral Nutrition can be found at: Email Alerts: http://pen.sagepub.com/cgi/alerts Subscriptions: http://pen.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Aug 27, 2009 OnlineFirst Version of Record - May 19, 2009 What is This? Downloaded from pen.sagepub.com by Karrie Derenski on April 1, 2013 Review Journal of Parenteral and Enteral Nutrition Volume 33 Number 5 September/October 2009 548-562 Micronutrient Supplementation in © 2009 American Society for Parenteral and Enteral Nutrition 10.1177/0148607108328470 Adult Nutrition Therapy: http://jpen.sagepub.com hosted at Practical Considerations http://online.sagepub.com Krishnan Sriram, MD, FRCS(C) FACS1; and Vassyl A. Lonchyna, MD, FACS2 Financial disclosure: none declared. Preexisting micronutrient (vitamins and trace elements) defi- for selenium (Se) and zinc (Zn). In practice, a multivitamin ciencies are often present in hospitalized patients. Deficiencies preparation and a multiple trace element admixture (containing occur due to inadequate or inappropriate administration, Zn, Se, copper, chromium, and manganese) are added to par- increased or altered requirements, and increased losses, affect- enteral nutrition formulations. -

AACT Herbal Dietary Supplements SIG Abstracts July 2017
AACT Herbal Dietary Supplements SIG Abstracts July 2017 1. A nationwide study of the incidence rate of herb-induced liver injury in Korea. Cho JH, Oh DS, Hong SH, Ko H, Lee NH, Park SE, Han CW, Kim SM, Kim YC, Kim KS, Choi CW, Shin SM, Kim KT, Choi HS, Lee JH, Kim JY, Kang JY, Lee DS, Ahn YC, Son CG. Arch Toxicol. 2017 Jun 20. doi: 10.1007/s00204-017-2007-9. [Epub ahead of print] Discrepant incidence has been reported regarding the incidence of herb-induced liver injury (HILI). To address the growing worldwide concern of HILI, we evaluated the risk of HILI in a nationwide prospective study. Between April 2013 and January 2016, 1001 inpatients (360 males and 641 females) from 10 tertiary hospitals throughout South Korea were treated with herbal drugs and had their liver enzymes periodically measured. A total of six patients met the criteria for HILI with RUCAM scores ranging from 4 to 7. All these participants were women and developed the hepatocellular type of HILI. One HILI participant met the criteria for Hy's law; however, none of six cases presented clinical symptoms related to liver injury. This is the first nationwide prospective study that estimated the extent of the incidence of HILI [total: 0.60%, 95% confidence interval (CI) 0.12-1.08; women: 0.95%, 95% CI 0.19-1.68] and described its features in hospitalized participants. DOI: 10.1007/s00204-017-2007-9 PMID: 28634823 2. Hepatotoxicity associated with weight loss or sports dietary supplements, including OxyELITE Pro™ - United States, 2013. -

Pharmacology
STATE ESTABLISHMENT «DNIPROPETROVSK MEDICAL ACADEMY OF HEALTH MINISTRY OF UKRAINE» V.I. MAMCHUR, V.I. OPRYSHKO, А.А. NEFEDOV, A.E. LIEVYKH, E.V.KHOMIAK PHARMACOLOGY WORKBOOK FOR PRACTICAL CLASSES FOR FOREIGN STUDENTS STOMATOLOGY DEPARTMENT DNEPROPETROVSK - 2016 2 UDC: 378.180.6:61:615(075.5) Pharmacology. Workbook for practical classes for foreign stomatology students / V.Y. Mamchur, V.I. Opryshko, A.A. Nefedov. - Dnepropetrovsk, 2016. – 186 p. Reviewed by: N.I. Voloshchuk - MD, Professor of Pharmacology "Vinnitsa N.I. Pirogov National Medical University.‖ L.V. Savchenkova – Doctor of Medicine, Professor, Head of the Department of Clinical Pharmacology, State Establishment ―Lugansk state medical university‖ E.A. Podpletnyaya – Doctor of Pharmacy, Professor, Head of the Department of General and Clinical Pharmacy, State Establishment ―Dnipropetrovsk medical academy of Health Ministry of Ukraine‖ Approved and recommended for publication by the CMC of State Establishment ―Dnipropetrovsk medical academy of Health Ministry of Ukraine‖ (protocol №3 from 25.12.2012). The educational tutorial contains materials for practical classes and final module control on Pharmacology. The tutorial was prepared to improve self-learning of Pharmacology and optimization of practical classes. It contains questions for self-study for practical classes and final module control, prescription tasks, pharmacological terms that students must know in a particular topic, medical forms of main drugs, multiple choice questions (tests) for self- control, basic and additional references. This tutorial is also a student workbook that provides the entire scope of student’s work during Pharmacology course according to the credit-modular system. The tutorial was drawn up in accordance with the working program on Pharmacology approved by CMC of SE ―Dnipropetrovsk medical academy of Health Ministry of Ukraine‖ on the basis of the standard program on Pharmacology for stomatology students of III - IV levels of accreditation in the specialties Stomatology – 7.110105, Kiev 2011. -

Poison Or Medicine, Toxin Or Drug?
Fact or Fiction? Jack W. Dini 1537 Desoto Way Livermore, CA 94550 E-mail: [email protected] Poison or Medicine, Toxin or Drug? “Poisons surround us. It’s not just too ing disorder often strikes those who Tomas Dolinay notes, “The data from much of a bad thing like arsenic that depend on small motor skills: musi- this work leads to a tempting specula- can cause trouble, it’s too much of cians, writers, surgeons. After treat- tion that inhaled CO might be useful in nearly anything. Too much vitamin ments with botulinum toxin, Fleisher minimizing VILI.”5 A, hypervitaminosis A, can cause liver is performing and touring again, and Small amounts of carbon monoxide damage. Too much vitamin D can recently released his first two-handed might alleviate symptoms of multiple damage the kidneys. Too much water recording in 40 years.1 sclerosis, a study in mice suggests. The can result in hyponatremia, a dilution finding may offer a treatment for MS, of the blood’s salt content, which which strikes when a person’s immune disrupts brain heart, and muscle func- Table 1 system damages the fatty sheaths that tion,” reports Cathy Newman.1 Hold a nickel in your hand. protect nerve fibers in the brain and However, more and more research Here’s how many lethal doses equal spinal cord.4 studies are revealing that a little bit that nickel’s weight1 Other studies of laboratory animals of some poisons can be quite helpful suggest that carbon monoxide in small to human health. Examples include Thallium 5 doses can prevent injury to blood ves- botulinum, carbon monoxide, hydro- 1080 Rat Poison 7 sels caused by surgery. -

Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment
This is a background paper for discussion. It does not reflect the views of the Committee and should not be cited. TOX/2012/16 COMMITTEE ON TOXICITY OF CHEMICALS IN FOOD, CONSUMER PRODUCTS AND THE ENVIRONMENT Review of potential risks from high levels of vitamin A in infant nutrition Introduction 1. The COT has been asked to provide advice on allergenicity of food and toxicity of chemicals in food, in support of a review by the Scientific Advisory Committee on Nutrition (SACN) of Government recommendations on complementary and young child feeding. An initial paper (TOX/2012/03), highlighting some of the areas requiring consideration was discussed by the COT in February, 2012. Members noted that data on exposure of weaning infants to vitamin A from liver and dietary supplements were limited. Toxicological information relevant to infants was also sparse therefore it was agreed that a more in-depth review was needed to consider risks to infants. Identity 2. Vitamin A is a lipid soluble, light yellow substance, which is an essential micronutrient responsible for promoting normal growth, vision and immunity. Vitamin A is effectively a group of lipid soluble compounds which are related to all-trans- retinol. It can be found in animals and animal-based products, as retinyl esters (most commonly retinyl palmitate), enriched fortified foods and supplements. Vitamin A can lead to adverse effects when there is a deficiency or excess of the nutrient (Perrotta, et al., 2003). Figure 1: Structural formula of retinol (C20H30O) 3. Collectively, retinol and retinyl esters are preformed vitamin A and are often referred to as retinoids. -
THE MINISTRY of HEALTH of UKRAINE NATIONAL UNIVERSITY of PHARMACY KROK WITHOUT PROBLEMS Study Guide for License Test Preparing
THE MINISTRY OF HEALTH OF UKRAINE NATIONAL UNIVERSITY OF PHARMACY THE DEPARTMENT OF PHARMACOLOGY Shtrygol’ S.Yu., Vereitinova V.P., Kudina O.V., Kononenko A.V. KROK WITHOUT PROBLEMS Study guide for license test preparing «Krok-1 Pharmacy» Kharkov-2019 Contents General pharmacology ............... 4 37. Pyracetam 38 80. Vicasol 59 Medicines affecting the respiratory system ................................................................................................................................................... 38 Medicines ........................... 10 81. Heparin 59 38. Acetylcysteine 38 Medicines affecting afferent 82. Dicumarol 61 39. Glaucin 39 Vitamin-containing medicines ....................................................................................................................................................................... 61 innervations: ............................. 10 Local anesthetics ................................................................40. Ambroxol................................ ................................41 83................................. Retinol .......................... 10 61 1. Lidocain 10 41. Theophylline 41 84. Alpha-tocopherol 62 2. Novocaine 11 42. Cromoline sodium 41 85. Ascorutinum 62 Medicines affecting efferent Cardiotonic medicines ................................................................86. Pyridoxine................................ ................................63 .................................................. 41 43. Digoxin 41 innervations: ............................ -

Vitamin D Toxicity
Post N Med 2016; XXIX(10): 756-759 ©Borgis *Ewa Marcinowska-Suchowierska1, Paweł Płudowski2 Vitamin D toxicity Zatrucie witaminą D 1Department of Geriatric, Internal Medicine and Metabolic Bone Disease, Centre of Postgraduate Medical Education, Warsaw Head of Department: Professor Marek Tałałaj, MD, PhD 2Department of Biochemistry, Radioimmunology and Experimental Medicine, The Children’s Memorial Health Institute, Warsaw Head of Department: Professor Roman Janas, PhD Keywords Summary vitamin D, 25(OH)D, toxicity, clinical Vitamin D toxicity (VDT), also called hypervitaminosis D, is a rare but potentially serious symptoms and management condition that occurs when an individual has excessive 25(OH)D levels in the bloodstream. Vitamin D toxicity is usually caused by extremely high doses of vitamin D supplements, not by diet or skin exposure to the sun. The main clinical consequence of VDT is elevated Słowa kluczowe serum calcium level (hypercalcemia) and a variety of nonspecific symptoms. The literature witamina D, 25(OH)D, toksyczność, reports that hypercalcemia due to overdosed vitamin D may appear if serum 25(OH)D objawy kliniczne, leczenie levels are higher than 150-200 ng/ml. Many different mechanisms have been proposed to account for VDT, including the vitamin D metabolite itself, VDR number, activity of 1 al- fa-hydroxylase, inhibition of vitamin D catabolism, and the capacity of VDBP. Mounting evidence that higher levels of vitamin D may have beneficial effects on bone and cellular health may predispose to enhanced administration of vitamin D and increased frequency of VDT. Hypercalcemia from VDT is rare, but a dangerous state for the organism and should receive adequate and sensible treatment.