Hypervitaminosis D with Osteosclerosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis and Treatment of Intramedullary Osteosclerosis
Abe et al. BMC Musculoskeletal Disorders (2020) 21:762 https://doi.org/10.1186/s12891-020-03758-5 CASE REPORT Open Access Diagnosis and treatment of intramedullary osteosclerosis: a report of three cases and literature review Kensaku Abe, Norio Yamamoto, Katsuhiro Hayashi, Akihiko Takeuchi* , Shinji Miwa, Kentaro Igarashi, Takashi Higuchi, Yuta Taniguchi, Hirotaka Yonezawa, Yoshihiro Araki, Sei Morinaga, Yohei Asano and Hiroyuki Tsuchiya Abstract Background: Intramedullary osteosclerosis (IMOS) is a rare condition without specific radiological findings except for the osteosclerotic lesion and is not associated with family history and infection, trauma, or systemic illness. Although the diagnosis of IMOS is confirmed after excluding other osteosclerotic lesions, IMOS is not well known because of its rarity and no specific feature. Therefore, these situations might result in delayed diagnosis. Hence, this case report aimed to investigate three cases of IMOS and discuss imaging findings and clinical outcomes. Case presentation: All three cases were examined between 2015 and 2019. The location of osteosclerotic lesions were femoral diaphyses in the 60-year-old man (Case 1) and 41-year-old woman (Case 2) and tibial diaphysis in the 44-year-old woman (Case 3). All cases complained of severe pain and showed massive diaphyseal osteosclerotic lesions in plain radiograms and computed tomography (CT) scans. Cases 2 and 3 were examined using the triphasic bone scan, and a fusiform-shaped intense area of the tracer uptake on delayed bone image was detected in both cases without (Case 2) or slightly increased vascularity (Case 3) on the blood pool image, which was reported as a specific finding of IMOS. -
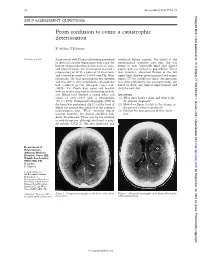
From Confusion to Coma: a Catastrophic Deterioration
52 Postgrad Med J 2001;77:52–55 Postgrad Med J: first published as 10.1136/pmj.77.903.53a on 1 January 2001. Downloaded from SELF ASSESSMENT QUESTIONS From confusion to coma: a catastrophic deterioration K Ashkan, F Johnston Answers on p 56. A previously well 45 year old woman presented ventilated before transfer. On arrival at the to the local casualty department with a one day neurosurgical intensive care unit, she was history of generalised headache, neck stiVness, found to have bilaterally fixed and dilated and blurred vision. On examination she had a pupils, with no corneal or gag reflexes. There temperature of 38°C, a pulse of 80 beats/min, was, however, abnormal flexion of the left and a blood pressure of 130/80 mm Hg. Neu- upper limb. She was given mannitol and urgent rologically, she had spontaneous eye opening repeat CT was carried out (fig 2). An operation and was able to obey commands, although she was then performed, but postoperatively she had confused speech (Glasgow coma scale failed to show any clinical improvement and (GCS), 14). Pupils were equal and reactive died the next day. with no cranial or peripheral neurological defi- cits. Blood tests showed a raised white cell Questions count of 20.9 × 109/l with a neutrophilia (1) What does figure 1 show and what is the (19.2 × 109/l). Computed tomography (CT) of diVerential diagnosis? the brain was performed (fig 1), on the basis of (2) How does figure 2 relate to the change in which the patient was referred to the regional the patient’s clinical condition? neurosurgical unit. -
Hypervitaminosis - an Emerging Pathological Condition
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Review Article Hypervitaminosis - An Emerging Pathological Condition J K Roop PG Department of Zoology, JC DAV College (Affiliated to Panjab University, Chandigarh), Dasuya-144205, District Hoshiarpur, Punjab, India ABSTRACT Vitamins are essential organic compounds that are required in small amounts to regulate various metabolic activities in the body. Prolonged and overconsumption of pharmaceutical forms of both water-soluble and fat-soluble vitamins may lead to toxicity and/or hypervitaminosis. Hypervitaminosis is an acute emerging pathological condition of the body due to excess accumulation of any of the vitamins. In case of acute poisoning with vitamin supplements/drugs, emergency assistance is required to detoxify the effects and restore the organization, structure and function of body’s tissues and organs. Sometimes death may occur due to intoxication to liver, kidney and heart. So, to manage any type of hypervitaminosis, proper diagnosis is essential to initiate eliminating the cause of its occurrence and accelerate the elimination of the supplement from the body. The present review discusses the symptoms of hypervitaminosis that seems to be a matter of concern today and management strategies to overcome toxicity or hypervitaminosis. Keywords: Hypervitaminosis, Toxicity, Vitamins, Vitamin pathology, Fat-soluble vitamin, Water- soluble vitamin. INTRODUCTION body, particularly in the liver. Vitamin B Vitamins are potent organic Complex and vitamin C are water- soluble. compounds present in small concentrations They are dissolved easily in food during in various fruits and vegetables. They cooking and a portion of these vitamins may regulate physiological functions and help in be destroyed by heating. -

The Practice and Regulatory Requirements Of
School of Public Health The Practice and Regulatory Requirements of Naturopathy and Western Herbal Medicine Vivian Lin Alan Bensoussan Stephen P. Myers Pauline McCabe Marc Cohen Sophie Hill Genevieve Howse November, 2005 Funded by the Department of Human Services, Victoria Copyright State of Victoria, Department of Human Services, 2006 This publication is copyright. No part may be reproduced by any process except in accordance with the provisions of the Copyright Act 1968 (Cth). Authorised by the State Government of Victoria, 50 Lonsdale Street Melbourne. This document may be downloaded from the following website: www.health.vic.gov.au/pracreg/naturopathy.htm ISBN-13: 978-0-9775864-0-0 ISBN-10: 0-9775864-0-5 Published by School of Public Health, La Trobe University Bundoora Victoria, 3086 Australia THE PRACTICE AND REGULATORY REQUIREMENTS OF NATUROPATHY AND WESTERN HERBAL MEDICINE CONTENTS VOLUME ONE Summary Report..........................................................................................................1 1. Introduction.......................................................................................................1 2. Methodology.....................................................................................................1 3. Key findings and recommendations..................................................................2 3.1 Definition of practice and scope of study ........................................................2 3.2 Growing use of naturopathy and WHM...........................................................3 -

Hepatic Pathology in Vitamin a Toxicity FAIRPOUR FOROUHAR, M.D.* MARTIN S
ANNALS OF CLINICAL AND LABORATORY SCIENCE, Vol. 14, No. 4 Copyright © 1984, Institute for Clinical Science, Inc. Hepatic Pathology in Vitamin A Toxicity FAIRPOUR FOROUHAR, M.D.* MARTIN S. NADEL, M.D.,t and BERNARD GONDOS, M.D.* *Department of Pathology, University of Connecticut, Farmington, CT 06032 and fDepartment of Pathology, Middlesex Memorial Hospital, Middletown, CT 06457 ABSTRACT This paper documents a case of vitamin A toxicity presenting with splenomegaly and ascites. The light microscopic, electron microscopic, and fluorescent findings are described in detail. The principal histopath ologic finding was marked perisinusoidal fibrosis. The role of Ito cells in the storage of lipid-soluble vitamins and their subsequent transformation to fibroblasts producing collagen are discussed. tient denied use of medications but admitted long Introduction time use of a self-prescribed vitamin B1-B6 combi nation, vitamin B12, iodine, and garlic. Vitamin A Liver disease resulting from vitamin A had been taken for six years, initially 75,000 units toxicity is an uncommon but well docu daily, increased to 150,000 units daily two years prior to admission because of believed problems with night mented entity.6’1414’22’26,27 The present vision for which no medical help had been sought. case provides a good model for the study Physical examination disclosed no palpable spleno of fibrosis of the space of Disse and its megaly with liver felt one cm beneath the right costal margin. An abdominal fluid wave was present. No pathophysiologic ^consequences. Similar spider angiomata were noted, and the remainder of changes also occur in other conditions re the physical examination was unremarkable. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Periapical Radiopacities
2016 self-study course two course The Ohio State University College of Dentistry is a recognized provider for ADA CERP credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to the Commission for Continuing Education Provider Recognition at www.ada.org/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education. This continuing education activity has been planned and implemented in accordance with the standards of the ADA Continuing Education Recognition Program (ADA CERP) through joint efforts between The Ohio State University College of Dentistry Office of Continuing Dental Education and the Sterilization Monitoring Service (SMS). ABOUT this COURSE… FREQUENTLY asked QUESTIONS… . READ the MATERIALS. Read and Q: Who can earn FREE CE credits? review the course materials. COMPLETE the TEST. Answer the A: EVERYONE - All dental professionals eight question test. A total of 6/8 in your office may earn free CE questions must be answered correctly credits. Each person must read the contact for credit. course materials and submit an online answer form independently. SUBMIT the ANSWER FORM ONLINE. You MUST submit your answers ONLINE at: Q: What if I did not receive a confirmation ID? us http://dentistry.osu.edu/sms-continuing-education A: Once you have fully completed your . -

Hematological Diseases and Osteoporosis
International Journal of Molecular Sciences Review Hematological Diseases and Osteoporosis , Agostino Gaudio * y , Anastasia Xourafa, Rosario Rapisarda, Luca Zanoli , Salvatore Santo Signorelli and Pietro Castellino Department of Clinical and Experimental Medicine, University of Catania, 95123 Catania, Italy; [email protected] (A.X.); [email protected] (R.R.); [email protected] (L.Z.); [email protected] (S.S.S.); [email protected] (P.C.) * Correspondence: [email protected]; Tel.: +39-095-3781842; Fax: +39-095-378-2376 Current address: UO di Medicina Interna, Policlinico “G. Rodolico”, Via S. Sofia 78, 95123 Catania, Italy. y Received: 29 April 2020; Accepted: 14 May 2020; Published: 16 May 2020 Abstract: Secondary osteoporosis is a common clinical problem faced by bone specialists, with a higher frequency in men than in women. One of several causes of secondary osteoporosis is hematological disease. There are numerous hematological diseases that can have a deleterious impact on bone health. In the literature, there is an abundance of evidence of bone involvement in patients affected by multiple myeloma, systemic mastocytosis, thalassemia, and hemophilia; some skeletal disorders are also reported in sickle cell disease. Recently, monoclonal gammopathy of undetermined significance appears to increase fracture risk, predominantly in male subjects. The pathogenetic mechanisms responsible for these bone loss effects have not yet been completely clarified. Many soluble factors, in particular cytokines that regulate bone metabolism, appear to play an important role. An integrated approach to these hematological diseases, with the help of a bone specialist, could reduce the bone fracture rate and improve the quality of life of these patients. -

Molecular Characterization of Three Canine Models of Human Rare Bone Diseases: Caffey, Van Den Ende-Gupta, and Raine Syndromes
RESEARCH ARTICLE Molecular Characterization of Three Canine Models of Human Rare Bone Diseases: Caffey, van den Ende-Gupta, and Raine Syndromes Marjo K. Hytönen1,2,3, Meharji Arumilli1,2,3, Anu K. Lappalainen4, Marta Owczarek-Lipska5, Vidhya Jagannathan5, Sruthi Hundi1,2,3, Elina Salmela1,2,3, Patrick Venta6, Eva Sarkiala4, Tarja Jokinen1,4, Daniela Gorgas7, Juha Kere2,3,8, Pekka Nieminen9, Cord Drögemüller5☯, a11111 Hannes Lohi1,2,3☯* 1 Department of Veterinary Biosciences, University of Helsinki, Helsinki, Finland, 2 Research Programs Unit, Molecular Neurology, University of Helsinki, Helsinki, Finland, 3 The Folkhälsan Institute of Genetics, Helsinki, Finland, 4 Department of Equine and Small Animal Medicine, University of Helsinki, Helsinki, Finland, 5 Institute of Genetics, Vetsuisse Faculty, University of Bern, Bern, Switzerland, 6 Department of Microbiology and Molecular Genetics, Michigan State University, East Lansing, Michigan, United States of America, 7 Division of Clinical Radiology, Department of Clinical Veterinary Medicine, Vetsuisse Faculty, OPEN ACCESS University of Bern, Bern, Switzerland, 8 Department of Biosciences and Nutrition, Karolinska Institutet, Huddinge, Sweden, 9 Department of Oral and Maxillofacial Diseases, University of Helsinki, Helsinki, Citation: Hytönen MK, Arumilli M, Lappalainen AK, Finland Owczarek-Lipska M, Jagannathan V, Hundi S, et al. ☯ (2016) Molecular Characterization of Three Canine These authors contributed equally to this work. * [email protected] Models of Human Rare Bone Diseases: Caffey, van den Ende-Gupta, and Raine Syndromes. PLoS Genet 12(5): e1006037. doi:10.1371/journal. pgen.1006037 Abstract Editor: Leigh Anne Clark, Clemson University, UNITED STATES One to two percent of all children are born with a developmental disorder requiring pediatric hospital admissions. -

Core Decompression for Avascular Necrosis (For North Carolina Only) – Community Plan Medical Policy
UnitedHealthcare® Community Plan Medical Policy Core Decompression for Avascular Necrosis (for North Carolina Only) Policy Number: CSNCT0219.01 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policies Application.......................................................................................... 1 None Coverage Rationale ........................................................................... 1 Applicable Codes .............................................................................. 1 Description of Services ..................................................................... 2 Clinical Evidence ............................................................................... 3 U.S. Food and Drug Administration ................................................ 7 References ......................................................................................... 7 Policy History/Revision Information................................................ 8 Instructions for Use ........................................................................... 8 Application This Medical Policy only applies to the state of North Carolina. Coverage Rationale Core decompression is proven and medically necessary for treating early (pre-collapse stage I and II) avascular necrosis of the femoral head. Core decompression is unproven and not medically necessary for treating late avascular necrosis of the femoral head or for avascular necrosis elsewhere, including the humeral head, the distal femur, the talus, or the -

Sclerosing Bone Dysplasias: Genetic, Clinical and Radiology Update of Hereditary and Non-Hereditary Disorders
BJR © 2016 The Authors. Published by the British Institute of Radiology Received: Revised: Accepted: http://dx.doi.org/10.1259/bjr.20150349 26 April 2015 14 December 2015 17 February 2016 Cite this article as: Boulet C, Madani H, Lenchik L, Vanhoenacker F, Amalnath DS, De Mey J, et al. Sclerosing bone dysplasias: genetic, clinical and radiology update of hereditary and non-hereditary disorders. Br J Radiol 2016; 89: 20150349. REVIEW ARTICLE Sclerosing bone dysplasias: genetic, clinical and radiology update of hereditary and non-hereditary disorders 1CEDRIC BOULET, MD, 2HARDI MADANI, FRCR, 3LEON LENCHIK, MD, 4FILIP VANHOENACKER, MD, PhD, 5DEEPAK S AMALNATH, MD, 1JOHAN DE MEY, MD, PhD and 1MICHEL DE MAESENEER, MD, PhD 1Department of Radiology, Universitair Ziekenhuis Brussel, Brussel, Belgium 2Department of Radiology, Royal Free Hospital, London, UK 3Department of Radiology, Wake Forest University, Winston Salem, NC, USA 4Department of Radiology, Universitair Ziekenhuis Anwerpen, Antwerpen, Belgium 5Department of Medicine, Indira Gandhi Medical College and Research Institute, Pondicherry, India Address correspondence to: Dr Michel De Maeseneer E-mail: [email protected] ABSTRACT There is a wide variety of hereditary and non-hereditary bone dysplasias, many with unique radiographic findings. Hereditary bony dysplasias include osteopoikilosis, osteopathia striata, osteopetrosis, progressive diaphyseal dysplasia, hereditary multiple diaphyseal sclerosis and pyknodysostosis. Non-hereditary dysplasias include melorheostosis, intramedullary osteosclerosis and overlap syndromes. Although many of these dysplasias are uncommon, radiologists should be familiar with their genetic, clinical and imaging findings to allow for differentiation from acquired causes of bony sclerosis. We present an overview of hereditary and non-hereditary bony dysplasias with focus on the pathogenesis, clinical and radiographic findings of each disorder. -

Hypophosphatasia: Enzyme Replacement Therapy Brings New Opportunities and New Challenges
PERSPECTIVE JBMR Hypophosphatasia: Enzyme Replacement Therapy Brings New Opportunities and New Challenges Michael P Whyte Department of Internal Medicine, Division of Bone and Mineral Diseases, Washington University School of Medicine, and Center for Metabolic Bone Disease and Molecular Research, Shriners Hospital for Children, St. Louis, MO, USA ABSTRACT Hypophosphatasia (HPP) is caused by loss-of-function mutation(s) of the gene that encodes the tissue-nonspecific isoenzyme of alkaline phosphatase (TNSALP). Autosomal inheritance (dominant or recessive) from among more than 300 predominantly missense defects of TNSALP (ALPL) explains HPP’s broad-ranging severity, the greatest of all skeletal diseases. In health, TNSALP is linked to cell surfaces and richly expressed in the skeleton and developing teeth. In HPP,TNSALP substrates accumulate extracellularly, including inorganic pyrophosphate (PPi), an inhibitor of mineralization. The PPi excess can cause tooth loss, rickets or osteomalacia, calcific arthropathies, and perhaps muscle weakness. Severely affected infants may seize from insufficient hydrolysis of pyridoxal 5‘- phosphate (PLP), the major extracellular vitamin B6. Now, significant successes are documented for newborns, infants, and children severely affected by HPP given asfotase alfa, a hydroxyapatite-targeted recombinant TNSALP. Since fall 2015, this biologic is approved by regulatory agencies multinationally typically for pediatric-onset HPP. Safe and effective treatment is now possible for this last rickets to have a medical therapy,