Enteric Nervous System Regulation of Intestinal Stem Cell Differentiation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’S Disease
life Review The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’s Disease Gianfranco Natale 1,2,* , Larisa Ryskalin 1 , Gabriele Morucci 1 , Gloria Lazzeri 1, Alessandro Frati 3,4 and Francesco Fornai 1,4 1 Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, 56126 Pisa, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (G.L.); [email protected] (F.F.) 2 Museum of Human Anatomy “Filippo Civinini”, University of Pisa, 56126 Pisa, Italy 3 Neurosurgery Division, Human Neurosciences Department, Sapienza University of Rome, 00135 Rome, Italy; [email protected] 4 Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) Neuromed, 86077 Pozzilli, Italy * Correspondence: [email protected] Abstract: The gastrointestinal (GI) tract is provided with a peculiar nervous network, known as the enteric nervous system (ENS), which is dedicated to the fine control of digestive functions. This forms a complex network, which includes several types of neurons, as well as glial cells. Despite extensive studies, a comprehensive classification of these neurons is still lacking. The complexity of ENS is magnified by a multiple control of the central nervous system, and bidirectional communication between various central nervous areas and the gut occurs. This lends substance to the complexity of the microbiota–gut–brain axis, which represents the network governing homeostasis through nervous, endocrine, immune, and metabolic pathways. The present manuscript is dedicated to Citation: Natale, G.; Ryskalin, L.; identifying various neuronal cytotypes belonging to ENS in baseline conditions. -

The Enteric Nervous System: a Second Brain
The Enteric Nervous System: A Second Brain MICHAEL D. GERSHON Columbia University Once dismissed as a simple collection of relay ganglia, the enteric nervous system is now recognized as a complex, integrative brain in its own right. Although we still are unable to relate complex behaviors such as gut motility and secretion to the activity of individual neurons, work in that area is proceeding briskly--and will lead to rapid advances in the management of functional bowel disease. Dr. Gershon is Professor and Chair, Department of Anatomy and Cell Biology, Columbia University College of Physicians and Surgeons, New York. In addition to numerous scientific publications, he is the author of The Second Brain (Harper Collins, New York, 1998). Structurally and neurochemically, the enteric nervous system (ENS) is a brain unto itself. Within those yards of tubing lies a complex web of microcircuitry driven by more neurotransmitters and neuromodulators than can be found anywhere else in the peripheral nervous system. These allow the ENS to perform many of its tasks in the absence of central nervous system (CNS) control--a unique endowment that has permitted enteric neurobiologists to investigate nerve cell ontogeny and chemical mediation of reflex behavior in a laboratory setting. Recognition of the importance of this work as a basis for developing effective therapies for functional bowel disease, coupled with the recent, unexpected discovery of major enteric defects following the knockout of murine genes not previously known to affect the gut, has produced a groundswell of interest that has attracted some of the best investigators to the field. Add to this that the ENS provides the closest thing we have to a window on the brain, and one begins to understand why the bowel--the second brain--is finally receiving the attention it deserves. -

Pin Faculty Directory
Harvard University Program in Neuroscience Faculty Directory 2019—2020 April 22, 2020 Disclaimer Please note that in the following descripons of faculty members, only students from the Program in Neuroscience are listed. You cannot assume that if no students are listed, it is a small or inacve lab. Many faculty members are very acve in other programs such as Biological and Biomedical Sciences, Molecular and Cellular Biology, etc. If you find you are interested in the descripon of a lab’s research, you should contact the faculty member (or go to the lab’s website) to find out how big the lab is, how many graduate students are doing there thesis work there, etc. Program in Neuroscience Faculty Albers, Mark (MGH-East)) De Bivort, Benjamin (Harvard/OEB) Kaplan, Joshua (MGH/HMS/Neurobio) Rosenberg, Paul (BCH/Neurology) Andermann, Mark (BIDMC) Dettmer, Ulf (BWH) Karmacharya, Rakesh (MGH) Rotenberg, Alex (BCH/Neurology) Anderson, Matthew (BIDMC) Do, Michael (BCH—Neurobio) Khurana, Vikram (BWH) Sabatini, Bernardo (HMS/Neurobio) Anthony, Todd (BCH/Neurobio) Dong, Min (BCH) Kim, Kwang-Soo (McLean) Sahay, Amar (MGH) Arlotta, Paola (Harvard/SCRB) Drugowitsch, Jan (HMS/Neurobio) Kocsis, Bernat (BIDMC) Sahin, Mustafa (BCH/Neurobio) Assad, John (HMS/Neurobio) Dulac, Catherine (Harvard/MCB) Kreiman, Gabriel (BCH/Neurobio) Samuel, Aravi (Harvard/ Physics) Bacskai, Brian (MGH/East) Dymecki, Susan(HMS/Genetics) LaVoie, Matthew (BWH) Sanes, Joshua (Harvard/MCB) Baker, Justin (McLean) Engert, Florian (Harvard/MCB) Lee, Wei-Chung (BCH/Neurobio) Saper, Clifford -

Identification of a Rhythmic Firing Pattern in the Enteric Nervous System That Generates Rhythmic Electrical Activity in Smooth Muscle
This Accepted Manuscript has not been copyedited and formatted. The final version may differ from this version. A link to any extended data will be provided when the final version is posted online. Research Articles: Systems/Circuits Identification of a rhythmic firing pattern in the enteric nervous system that generates rhythmic electrical activity in smooth muscle Nick J Spencer1, Timothy J Hibberd1, Lee Travis1, Lukasz Wiklendt1, Marcello Costa1, Hongzhen Hu2, Simon J Brookes1, David A Wattchow3, Phil G Dinning1,3, Damien J Keating1 and Julian Sorensen4 1College of Medicine and Public Health & Centre for Neuroscience, Flinders University, Adelaide, Australia 2Department of Anesthesiology, The Center for the Study of Itch, Washington University School of Medicine, St. Louis, MO, USA 3Discipline of Surgery and Gastroenterology, Flinders Medical Centre, South Australia. 4Cyber Sensing and Shaping, Cyber & Electronic Warfare Division, Defence, Science & Technology Group, Edinburgh, South Australia, Australia. DOI: 10.1523/JNEUROSCI.3489-17.2018 Received: 7 December 2017 Revised: 30 April 2018 Accepted: 9 May 2018 Published: 28 May 2018 Author contributions: N.J.S., M.C., and H.H. designed research; N.J.S. wrote the first draft of the paper; N.J.S., S.J.B., D.A.W., P.D., D.J.K., and J.S. edited the paper; N.J.S., T.H., M.C., H.H., and J.S. wrote the paper; T.H. and L.T. performed research; T.H. contributed unpublished reagents/analytic tools; T.H., L.T., L.W., and J.S. analyzed data. Conflict of Interest: The authors declare no competing financial interests. The experiments carried out in this study were funded by grants to NJS (grant # 1067317 & 1127140) from the National Health and Medical Research Council (NH & MRC) of Australia. -

The Autonomic Nervous System and Gastrointestinal Tract Disorders
NEUROMODULATION THE AUTONOMIC NERVOUS SYSTEM AND GASTROINTESTINALTRACT DISORDERS TERRY L. POWLEY, PH.D. PURDUE UNIVERSITY • MULTIPLE REFRACTORY GI DISORDERS EXIST. • VISCERAL ATLASES OF THE GI TRACT ARE AVAILABLE. • REMEDIATION WITH ELECTROMODULATION MAY BE PRACTICAL. TERRY l. POWLEY, PH.D. PURDUE NEUROMODUlATION: THE AUTONOMIC NERVOUS SYSTEM AND GASTP.OINTESTINAL TRACT DISORDERS UNIVERSITY 50 INTERNATIONAL I:"' NEUROMODULATION SOCIETY 0 40 ·IS 12TH WORLD CONGRESS -I: -• 30 !"' A. -..0 20 ..a• E 10 z::::t TERRY l. POWLEY, PH.D. PURDUE NEUROMODUlATION: THE AUTONOMIC NERVOUS SYSTEM AND GASTP.OINTESTINAL TRACT DISORDERS UNIVERSITY DISORDERS TO TREAT WITH NEUROMODULATION ACHALASIA DYSPHAGIA GASTROPARESIS GERD GUT DYSMOTILITY MEGA ESOPHAGUS DYSPEPSIA ,, VISCERAL PAIN l1 ' I NAUSEA, EMESIS OBESITY ,, ' 11 I PYLORIC STENOSIS ==..:.= --- "" .:.= --- .. _ _, DUMPING REFLUX COLITIS I:' . - IBS -·-- - CROHN'S DISEASE HIRSCHSPRUNG DISEASE CHAGAS DISUSE Gastrointestinal Tract Awodesk@ Ma;·a@ TERRY l. POWLEY, PH.D. PURDUE NEUROMODUlATION: THE AUTONOMIC NERVOUS SYSTEM AND GASTP.OINTESTINAL TRACT DISORDERS UNIVERSITY TIME The Obesity Epidemic in America ·. TERRY l. POWLEY, PH.D. PURDUE NEU ROMODUlATION : THE AUTO N OMIC NERVOUS SYSTEM A N D G A STP.OINTESTINAL TRACT DISORDERS UNI V E R SI TY ROUX-EN-Y BYPASS Bypassed portion of stomach Gastric -"'~ pouch Bypassed - Jejunum duodenum -1" food -___----_,,.,. digestivejuice TERRY l. POWLEY, PH.D. PURDUE NEU ROMODUlATION: THE AUTONOMIC NERVOUS SYSTEM A N D GASTP.OINTESTINAL TRACT DISORDERS UNIVERSITY 8y~s~ portionof i t()(l\3Ch • TERRYl. POWLEY, PH.D. PURDUE NEUROMOOUlATION: THE AUTONOMIC NERVOUS SYSTEM ANO 0.-STP.OINTESTINAL TRACT DISORDERS UHIVlflSITY • DESPERATE PATIENTS • ABSENCE OF SATISFACTORY PHARMACOLOGICAL TREATMENTS • POPULAR MEDIA HYPE • ABSENCE OF A SOLID MECHANISTIC UNDERSTANDING • UNCRITICAL ACCEPTANCE OF PROPONENT'S CLAIMS • MYOPIA REGARDING SIDE EFFECTS TERRY l. -

Heparin-Binding EGF-Like Growth Factor Promotes Neuronal Nitric Oxide Synthase Expression and Protects the Enteric Nervous System After Necrotizing Enterocolitis
Articles | Translational Investigation nature publishing group Heparin-binding EGF-like growth factor promotes neuronal nitric oxide synthase expression and protects the enteric nervous system after necrotizing enterocolitis Yu Zhou1, Yijie Wang1, Jacob Olson1, Jixin Yang1 and Gail E. Besner1 BACKGROUND: Neonatal necrotizing enterocolitis (NEC) is produced by myenteric neurons. Neuronal nitric oxide associated with alterations of the enteric nervous system synthase (nNOS)-producing neurons and choline acetyl (ENS), with loss of neuronal nitric oxide synthase (nNOS)- transferase (ChAT)-producing neurons are two major intest- expressing neurons in the intestine. The aim of this study was inal neuronal subpopulations involved in the regulation of to investigate the roles of heparin-binding EGF-like growth intestinal motility, and nNOS/ChAT misbalance has been factor (HB-EGF) in neural stem cell (NSC) differentiation, nNOS reported in certain inflammatory intestinal diseases and expression, and effects on ENS integrity during genetic intestinal motility disorders (2,3). We have shown experimental NEC. that neonatal NEC is associated with alterations of the ENS, METHODS: The effects of HB-EGF on NSC differentiation and with significant loss of nNOS-expressing neurons not only in nNOS production were determined using cultured enteric the acute stages of the disease but also months later at the NSCs. Myenteric neuronal subpopulations were examined in time of stoma closure (4). This decreased nNOS expression HB-EGF knockout mice. Rat pups were exposed to experi- may explain the intestinal dysmotility seen in NEC patients mental NEC, and the effects of HB-EGF treatment on nNOS even after recovery from the acute event. Current therapy for production and intestinal neuronal apoptosis were intestinal dysmotility is limited mainly to palliation, and new determined. -

Regional Complexity in Enteric Neuron Wiring Reflects Diversity of Motility
RESEARCH ARTICLE Regional complexity in enteric neuron wiring reflects diversity of motility patterns in the mouse large intestine Zhiling Li1, Marlene M Hao2, Chris Van den Haute3,4, Veerle Baekelandt3, Werend Boesmans1,5,6*, Pieter Vanden Berghe1* 1Laboratory for Enteric NeuroScience (LENS), Translational Research Center for Gastrointestinal Disorders (TARGID), University of Leuven, Leuven, Belgium; 2Department of Anatomy and Neuroscience, University of Melbourne, Melbourne, Australia; 3Laboratory for Neurobiology and Gene Therapy, Department of Neurosciences, KU Leuven, Leuven, Belgium; 4Leuven Viral Vector Core, KU Leuven, Leuven, Belgium; 5Department of Pathology, GROW-School for Oncology and Developmental Biology, Maastricht University Medical Center, Maastricht, The Netherlands; 6Biomedical Research Institute (BIOMED), Hasselt University, Hasselt, Belgium Abstract The enteric nervous system controls a variety of gastrointestinal functions including intestinal motility. The minimal neuronal circuit necessary to direct peristalsis is well-characterized but several intestinal regions display also other motility patterns for which the underlying circuits and connectivity schemes that coordinate the transition between those patterns are poorly understood. We investigated whether in regions with a richer palette of motility patterns, the underlying nerve circuits reflect this complexity. Using Ca2+ imaging, we determined the location *For correspondence: and response fingerprint of large populations of enteric neurons upon focal network -

Development of Enteric Neurons and Muscularis Macrophages Marina Avetisyan Washington University in St
Washington University in St. Louis Washington University Open Scholarship Arts & Sciences Electronic Theses and Dissertations Arts & Sciences Spring 5-15-2019 Development of Enteric Neurons and Muscularis Macrophages Marina Avetisyan Washington University in St. Louis Follow this and additional works at: https://openscholarship.wustl.edu/art_sci_etds Part of the Allergy and Immunology Commons, Immunology and Infectious Disease Commons, Medical Immunology Commons, and the Neuroscience and Neurobiology Commons Recommended Citation Avetisyan, Marina, "Development of Enteric Neurons and Muscularis Macrophages" (2019). Arts & Sciences Electronic Theses and Dissertations. 1781. https://openscholarship.wustl.edu/art_sci_etds/1781 This Dissertation is brought to you for free and open access by the Arts & Sciences at Washington University Open Scholarship. It has been accepted for inclusion in Arts & Sciences Electronic Theses and Dissertations by an authorized administrator of Washington University Open Scholarship. For more information, please contact [email protected]. WASHINGTON UNIVERSITY IN ST. LOUIS Division of Biology and Biomedical Sciences Neurosciences Dissertation Examination Committee: Robert O. Heuckeroth, Chair Aaron DiAntonio, Co-Chair Paul Bridgman Joseph Dougherty Kelly Monk Development of Enteric Neurons and Muscularis Macrophages. by Marina Avetisyan A dissertation presented to The Graduate School of Washington University in partial fulfillment of the requirements for the degree of Doctor of Philosophy May 2019 St. Louis, -

Building a Second Brain in the Bowel
Building a second brain in the bowel Marina Avetisyan, … , Ellen Merrick Schill, Robert O. Heuckeroth J Clin Invest. 2015;125(3):899-907. https://doi.org/10.1172/JCI76307. Review Series The enteric nervous system (ENS) is sometimes called the “second brain” because of the diversity of neuronal cell types and complex, integrated circuits that permit the ENS to autonomously regulate many processes in the bowel. Mechanisms supporting ENS development are intricate, with numerous proteins, small molecules, and nutrients that affect ENS morphogenesis and mature function. Damage to the ENS or developmental defects cause vomiting, abdominal pain, constipation, growth failure, and early death. Here, we review molecular mechanisms and cellular processes that govern ENS development, identify areas in which more investigation is needed, and discuss the clinical implications of new basic research. Find the latest version: https://jci.me/76307/pdf The Journal of Clinical Investigation REVIEW SERIES: ENTERIC NERVOUS SYSTEM Series Editor: Rodger Liddle Building a second brain in the bowel Marina Avetisyan,1 Ellen Merrick Schill,1 and Robert O. Heuckeroth2 1Washington University School of Medicine, St. Louis, Missouri, USA. 2Children’s Hospital of Philadelphia Research Institute and Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA. The enteric nervous system (ENS) is sometimes called the “second brain” because of the diversity of neuronal cell types and complex, integrated circuits that permit the ENS to autonomously regulate many processes in the bowel. Mechanisms supporting ENS development are intricate, with numerous proteins, small molecules, and nutrients that affect ENS morphogenesis and mature function. Damage to the ENS or developmental defects cause vomiting, abdominal pain, constipation, growth failure, and early death. -

Luminal Nutrients Activate Distinct Patterns in Submucosal and Myenteric Neurons in the Mouse Small Intestine
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.19.427232; this version posted January 20, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Luminal nutrients activate distinct patterns in submucosal and myenteric neurons in the mouse small intestine C. Fung1, M.M. Hao2, Y. Obata3, J. Tack1, V. Pachnis3, W. Boesmans4,5, P. Vanden Berghe1* 1Laboratory for Enteric NeuroScience (LENS), Translational Research Center for Gastrointestinal Disorders (TARGID), University of Leuven, Leuven, Belgium 2Department of Anatomy and Neuroscience, University of Melbourne, Parkville, Victoria, Australia 3The Francis Crick Institute, London, UK 4Department of Pathology, GROW-School for Oncology and Developmental Biology, Maastricht University Medical Center, Maastricht, The Netherlands. 5Biomedical Research Institute (BIOMED), Hasselt University, Hasselt, Belgium. *Correspondence: Pieter Vanden Berghe, [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.01.19.427232; this version posted January 20, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Nutrient signals sensed by enteroendocrine cells are conveyed to the enteric nervous system (ENS) to initiate intestinal reflexes. We addressed whether there are specific enteric pathways dedicated to detecting different luminal nutrients. Calcium imaging was performed on intact jejunal preparations from Wnt1-cre;R26R-GCaMP3 and Villin-cre;R26R-GCaMP3 mice which express a fluorescent calcium indicator in their ENS or intestinal epithelium, respectively. Glucose, acetate, and L-phenylalanine were perfused onto the mucosa whilst imaging underlying enteric neurons. -

The Parasympathetic System
DR MOUIN ABBOUD PR OF ANATOMY In faculity of medecin ( Damascus and Sham uneversities ) Specialist in respiratory diseases الدكتور معين عبود استاذ التشريح في كلية الطب البشري في جامعة دمشق وجامعة الشام الخاصة اختصاصي في أمراض جهاز التنفس DR MOUIN ABBOUD Abdominal viscera Innervation The Innervation Abdominal viscera are innervated by both : extrinsic ) visceral innervation ( involves : . receiving motor impulses from the central nervous system . and sending sensory information to, the central nervous system; and intrinsic components of the nervous system: involves the regulation of digestive tract activities by a generally self-sufficient network of sensory and motor neurons (the enteric nervous system). Visceral innervation The visceral innervation is transmited by Autonomic Plexuses )prevertebral plexus ). By which : these viscera send sensory information back to the central nervous system through visceral afferent fibers and receive motor impulses from the central nervous system through visceral efferent fibers. prevertebral plexus The abdominal prevertebral plexus receives: preganglionic parasympathetic and visceral afferent fibers from the vagus nerves [X]; preganglionic sympathetic and visceral afferent fibers from the thoracic and lumbar splanchnic nerves; preganglionic parasympathetic fibers from the pelvic splanchnic nerves. The Sympathetic Division The sympathetic division consists of the following: Preganglionic fibers in the lateral grey column of the thoracic and upper two lumbar segments of the spinal cord. Ganglionic neurons in : . Sympathetic chain ganglia, also called paravertebral, or lateral ganglia . Collateral ganglia, also known as prevertebral ganglia . Specialized neurons in the interior of the suprarenal gland Postganglionic fibers : to target organs Sectional Organization of the Spinal Cord The parasympathetic system The parasympathetic system is less neatly defined Preganglionic fibers . -
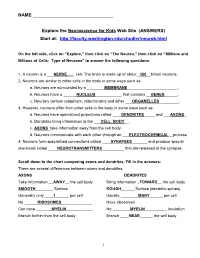
ANSWERS) Start At
NAME ________________________________ Explore the Neuroscience for Kids Web Site (ANSWERS) Start at: http://faculty.washington.edu/chudler/neurok.html On the left side, click on “Explore,” then click on “The Neuron,” then click on “Millions and Billions of Cells: Type of Neurons” to answer the following questions: 1. A neuron is a ___NERVE___ cell. The brain is made up of about _100__billion neurons. 2. Neurons are similar to other cells in the body in some ways such as: a. Neurons are surrounded by a ________MEMBRANE_______________________. b. Neurons have a ______NUCLEUS____________ that contains __GENES______. c. Neurons contain cytoplasm, mitochondria and other ___ORGANELLES_________. 3. However, neurons differ from other cells in the body in some ways such as: a. Neurons have specialized projections called ____DENDRITES_____ and ___AXONS_. b. Dendrites bring information to the ___CELL BODY__. c. AXONS_take information away from the cell body. d. Neurons communicate with each other through an ___ELECTROCHEMICAL__process. 4. Neurons form specialized connections called ____SYNAPSES_______ and produce special chemicals called ____NEUROTRANSMITTERS__________ that are released at the synapse. Scroll down to the chart comparing axons and dendrites. Fill in the answers: There are several differences between axons and dendrites: AXONS DENDRITES Take information __AWAY__ the cell body Bring information _TOWARD__ the cell body SMOOTH________ Surface ROUGH______ Surface (dendritic spines) Generally only ____1______ per cell Usually ________MANY______ per cell No ______RIBOSOMES______________ Have ribosomes Can have _______MYELIN____________ No ________MYELIN__________ insulation Branch further from the cell body Branch ____NEAR______ the cell body 1 Take the short neuron quiz at the bottom of the page, and correctly answer these questions: 1. Neuron part that releases neurotransmitters into the synaptic cleft.