Dissecting the Heterogeneity in T-Cell Mediated Inflammation In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
UNITEL PROUDLY REPRESENTS the INTERNATIONAL TV DISTRIBUTION of Browse Through the Complete Unitel Catalogue of More Than 2,000 Titles At
UNITEL PROUDLY REPRESENTS THE INTERNATIONAL TV DISTRIBUTION OF Browse through the complete Unitel catalogue of more than 2,000 titles at www.unitel.de Date: March 2018 FOR CO-PRODUCTION & PRESALES INQUIRIES PLEASE CONTACT: Unitel GmbH & Co. KG Gruenwalder Weg 28D · 82041 Oberhaching/Munich, Germany Tel: +49.89.673469-613 · Fax: +49.89.673469-610 · [email protected] Ernst Buchrucker Dr. Thomas Hieber Dr. Magdalena Herbst Managing Director Head of Business and Legal Affairs Head of Production [email protected] [email protected] [email protected] Tel: +49.89.673469-19 Tel: +49.89.673469-611 Tel: +49.89.673469-862 WORLD SALES C Major Entertainment GmbH Meerscheidtstr. 8 · 14057 Berlin, Germany Tel.: +49.30.303064-64 · [email protected] Elmar Kruse Niklas Arens Nishrin Schacherbauer Managing Director Sales Manager, Director Sales Sales Manager [email protected] & Marketing [email protected] [email protected] Nadja Joost Ira Rost Sales Manager, Director Live Events Sales Manager, Assistant to & Popular Music Managing Director [email protected] [email protected] CONTENT BRITTEN: GLORIANA Susan Bullock/Toby Spence/Kate Royal/Peter Coleman-Wright Conducted by: Paul Daniel OPERAS 3 Staged by: Richard Jones BALLETS 8 Cat. No. A02050015 | Length: 164' | Year: 2016 DONIZETTI: LA FILLE DU RÉGIMENT Natalie Dessay/Juan Diego Flórez/Felicity Palmer Conducted by: Bruno Campanella Staged by: Laurent Pelly Cat. No. A02050065 | Length: 131' | Year: 2016 OPERAS BELLINI: NORMA Sonya Yoncheva/Joseph Calleja/Sonia Ganassi/ Brindley Sherratt/La Fura dels Baus Conducted by: Antonio Pappano Staged by: Àlex Ollé Cat. -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

2017 American College of Rheumatology/American Association
Arthritis Care & Research Vol. 69, No. 8, August 2017, pp 1111–1124 DOI 10.1002/acr.23274 VC 2017, American College of Rheumatology SPECIAL ARTICLE 2017 American College of Rheumatology/ American Association of Hip and Knee Surgeons Guideline for the Perioperative Management of Antirheumatic Medication in Patients With Rheumatic Diseases Undergoing Elective Total Hip or Total Knee Arthroplasty SUSAN M. GOODMAN,1 BRYAN SPRINGER,2 GORDON GUYATT,3 MATTHEW P. ABDEL,4 VINOD DASA,5 MICHAEL GEORGE,6 ORA GEWURZ-SINGER,7 JON T. GILES,8 BEVERLY JOHNSON,9 STEVE LEE,10 LISA A. MANDL,1 MICHAEL A. MONT,11 PETER SCULCO,1 SCOTT SPORER,12 LOUIS STRYKER,13 MARAT TURGUNBAEV,14 BARRY BRAUSE,1 ANTONIA F. CHEN,15 JEREMY GILILLAND,16 MARK GOODMAN,17 ARLENE HURLEY-ROSENBLATT,18 KYRIAKOS KIROU,1 ELENA LOSINA,19 RONALD MacKENZIE,1 KALEB MICHAUD,20 TED MIKULS,21 LINDA RUSSELL,1 22 14 23 17 ALEXANDER SAH, AMY S. MILLER, JASVINDER A. SINGH, AND ADOLPH YATES Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The ACR considers adherence to the recommendations within this guideline to be volun- tary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote benefi- cial or desirable outcomes but cannot guarantee any specific outcome. Guidelines and recommendations developed and endorsed by the ACR are subject to periodic revision as warranted by the evolution of medi- cal knowledge, technology, and practice. -

Curriculum Vitae: Daniel J
CURRICULUM VITAE: DANIEL J. WALLACE, M.D., F.A.C.P., M.A.C.R. Up to date as of January 1, 2019 Personal: Address: 8750 Wilshire Blvd, Suite 350 Beverly Hills, CA 90211 Phone: (310) 652-0010 FAX: (310) 360-6219 E mail: [email protected] Education: University of Southern California, 2/67-6/70, BA Medicine, 1971. University of Southern California, 9/70-6/74, M.D, 1974. Postgraduate Training: 7/74-6/75 Medical Intern, Rhode Island (Brown University) Hospital, Providence, RI. 7/75-6/77 Medical Resident, Cedars-Sinai Medical Center, Los Angeles, CA. 7/77-6/79 Rheumatology Fellow, UCLA School of Medicine, Los Angeles, CA. Medical Boards and Licensure: Diplomate, National Board of Medical Examiners, 1975. Board Certified, American Board of Internal Medicine, 1978. Board Certified, Rheumatology subspecialty, 1982. California License: #G-30533. Present Appointments: Medical Director, Wallace Rheumatic Study Center Attune Health Affiliate, Beverly Hills, CA 90211 Attending Physician, Cedars-Sinai Medical Center, Los Angeles, 1979- Clinical Professor of Medicine, David Geffen School of Medicine at UCLA, 1995- Professor of Medicine, Cedars-Sinai Medical Center, 2012- Expert Reviewer, Medical Board of California, 2007- Associate Director, Rheumatology Fellowship Program, Cedars-Sinai Medical Center, 2010- Board of Governors, Cedars-Sinai Medical Center, 2016- Member, Medical Policy Committee, United Rheumatology, 2017- Honorary Appointments: Fellow, American College of Physicians (FACP) Fellow, American College of Rheumatology (FACR) -

Fontolizumab, a Humanised Anti-Interferon C Antibody
1131 INFLAMMATORY BOWEL DISEASE Gut: first published as 10.1136/gut.2005.079392 on 28 February 2006. Downloaded from Fontolizumab, a humanised anti-interferon c antibody, demonstrates safety and clinical activity in patients with moderate to severe Crohn’s disease D W Hommes, T L Mikhajlova, S Stoinov, D Sˇtimac, B Vucelic, J Lonovics, M Za´kuciova´, G D’Haens, G Van Assche, S Ba, S Lee, T Pearce ............................................................................................................................... Gut 2006;55:1131–1137. doi: 10.1136/gut.2005.079392 See end of article for Introduction: Interferon c is a potent proinflammatory cytokine implicated in the inflammation of Crohn’s authors’ affiliations ....................... disease (CD). We evaluated the safety and efficacy of fontolizumab, a humanised anti-interferon c antibody, in patients with moderate to severe CD. Correspondence to: Methods: A total of 133 patients with Crohn’s disease activity index (CDAI) scores between 250 and 450, Dr D W Hommes, Department inclusive, were randomised to receive placebo or fontolizumab 4 or 10 mg/kg. Forty two patients Gastroenterology and received one dose and 91 patients received two doses on days 0 and 28. Investigators and patients were Hepatology, Academic unaware of assignment. Study end points were safety, clinical response (decrease in CDAI of 100 points or Medical Centre, C2-111, ( Meibergdreef 9 1105 AZ, more), and remission (CDAI 150). Amsterdam, the Results: There was no statistically significant difference in the primary end point of the study (clinical Netherlands; response) between the fontolizumab and placebo groups after a single dose at day 28. However, patients d.w.hommes@ receiving two doses of fontolizumab demonstrated doubling in response rate at day 56 compared with amc.uva.nl placebo: 32% (9/28) versus 69% (22/32, p = 0.02) and 67% (21/31, p = 0.03) for the placebo, and 4 Revised version received and 10 mg/kg fontolizumab groups, respectively. -

[Product Monograph Template
PRODUCT MONOGRAPH PrXELJANZ® tofacitinib, tablets, oral 5 mg tofacitinib (as tofacitinib citrate) 10 mg tofacitinib (as tofacitinib citrate) PrXELJANZ® XR tofacitinib extended-release, tablets, oral 11 mg tofacitinib (as tofacitinib citrate) ATC Code: L04AA29 Selective Immunosuppressant Pfizer Canada ULC Date of Preparation: 17,300 Trans-Canada Highway October 24, 2019 Kirkland, Quebec H9J 2M5 TMPF PRISM C.V. c/o Pfizer Manufacturing Holdings LLC Pfizer Canada ULC, Licensee © Pfizer Canada ULC 2019 Submission Control No: 230976 XELJANZ/XELJANZ XR Page 1 of 80 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION.........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS ...................................................................................................4 ADVERSE REACTIONS..................................................................................................15 DRUG INTERACTIONS ..................................................................................................29 DOSAGE AND ADMINISTRATION..............................................................................34 OVERDOSAGE ................................................................................................................38 ACTION AND CLINICAL PHARMACOLOGY ............................................................38 -

New Biological Therapies: Introduction to the Basis of the Risk of Infection
New biological therapies: introduction to the basis of the risk of infection Mario FERNÁNDEZ RUIZ, MD, PhD Unit of Infectious Diseases Hospital Universitario “12 de Octubre”, Madrid ESCMIDInstituto de Investigación eLibraryHospital “12 de Octubre” (i+12) © by author Transparency Declaration Over the last 24 months I have received honoraria for talks on behalf of • Astellas Pharma • Gillead Sciences • Roche • Sanofi • Qiagen Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author Paul Ehrlich (1854-1915) • “side-chain” theory (1897) • receptor-ligand concept (1900) • “magic bullet” theory • foundation for specific chemotherapy (1906) • Nobel Prize in Physiology and Medicine (1908) (together with Metchnikoff) Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author 1981: B-1 antibody (tositumomab) anti-CD20 monoclonal antibody 1997: FDA approval of rituximab for the treatment of relapsed or refractory CD20-positive NHL 2001: FDA approval of imatinib for the treatment of chronic myelogenous leukemia Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author Functional classification of targeted (biological) agents • Agents targeting soluble immune effector molecules • Agents targeting cell surface receptors -

Verdi Otello
VERDI OTELLO RICCARDO MUTI CHICAGO SYMPHONY ORCHESTRA ALEKSANDRS ANTONENKO KRASSIMIRA STOYANOVA CARLO GUELFI CHICAGO SYMPHONY CHORUS / DUAIN WOLFE Giuseppe Verdi (1813-1901) OTELLO CHICAGO SYMPHONY ORCHESTRA RICCARDO MUTI 3 verdi OTELLO Riccardo Muti, conductor Chicago Symphony Orchestra Otello (1887) Opera in four acts Music BY Giuseppe Verdi LIBretto Based on Shakespeare’S tragedy Othello, BY Arrigo Boito Othello, a Moor, general of the Venetian forces .........................Aleksandrs Antonenko Tenor Iago, his ensign .........................................................................Carlo Guelfi Baritone Cassio, a captain .......................................................................Juan Francisco Gatell Tenor Roderigo, a Venetian gentleman ................................................Michael Spyres Tenor Lodovico, ambassador of the Venetian Republic .......................Eric Owens Bass-baritone Montano, Otello’s predecessor as governor of Cyprus ..............Paolo Battaglia Bass A Herald ....................................................................................David Govertsen Bass Desdemona, wife of Otello ........................................................Krassimira Stoyanova Soprano Emilia, wife of Iago ....................................................................BarBara DI Castri Mezzo-soprano Soldiers and sailors of the Venetian Republic; Venetian ladies and gentlemen; Cypriot men, women, and children; men of the Greek, Dalmatian, and Albanian armies; an innkeeper and his four servers; -

Cairo Alexandria 16-Jul 03:00.37 1 2 AMR MOHAMED
2017 UIPM LASER RUN CITY TOUR (LRCT) WORLD RANKING - ELITE DIVISON Updated 16/11/2017 after LRCT: Tbilisi (GEO), 01/04/2017 Sausset Les Pins (FRA), 08/04/2017 Karnal (IND), 09/04/2017 Rostov on Don (RUS), 01/05/2017 Rustavi (GEO), 06/05/2017 Lagos (NGR), 06/05/2017 Kiev (UKR), 14/05/2017 Perpignan (FRA), 14/05/2017 Pretoria (RSA), 20/05/2017 Cairo (EGY), 26/05/2017 Covilha (POR), 03/06/2017 Bath (GBR), 04/06/2017 Alexandria (EGY), 16/06/2017 Pune (IND), 17/06/2017 London (GBR), 18/06/2017 Madiwela Kotte (SRI), 25/06/2017 Alenquer (POR), 25/06/2017 Hull (GBR), 02/07/2017 Singapore (SIN), 30/07/2017 Delhi (IND), 27/08/2017 Mossel Bay (RSA), 02/09/2017 Geelong (AUS), 02/09/2017 Thessaloníki (GRE), 16/09/2017 Amadora (POR), 24/09/2017 Colombo (SRI), 30/09/2017 Division ELITE Age Group U11 Running Sequence 2x400m Gender Female Shooting Distance 5m (2 hands opt) Athlete Best Natio LRCT # UIPM ID School/ Club Name LRCT City Finishing WR Surname First Name n Date Time 1 WALED MOHAMED OSMAN MOHAMED ELGENDY GANA EGY Ahly bank - cairo Alexandria 16-Jul 03:00.37 1 2 AMR MOHAMED ABDELFATTAH MOHAMED SARA EGY Shams club Alexandria 16-Jul 03:01.20 2 3 HAZEM AHMED SAMIR MOHAMED AHMED SAMAHA SHAHD EGY Shams club Alexandria 16-Jul 03:07.50 3 4 MOHAMED SALAH HUSSIEN ELSAYED BASMALA EGY Shams club Alexandria 16-Jul 03:10.39 4 5 ALAA KAMAL ELSAYED GHONEM LAILA EGY Shams club Alexandria 16-Jul 03:11.08 5 6 ABDALLAH MOHAMED ABDALLAH SALAMAH ZINA EGY Shams club Alexandria 16-Jul 03:12.33 6 7 HISHAM ALI MAHMOUD YOUMNA EGY Sherouk Alexandria 16-Jul 03:16.12 7 8 -
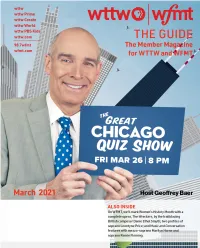
Geoffrey Baer, Who Each Friday Night Will Welcome Local Contestants Whose Knowledge of Trivia About Our City Will Be Put to the Test
From the President & CEO The Guide The Member Magazine Dear Member, for WTTW and WFMT This month, WTTW is excited to premiere a new series for Chicago trivia buffs and Renée Crown Public Media Center curious explorers alike. On March 26, join us for The Great Chicago Quiz Show hosted by 5400 North Saint Louis Avenue Chicago, Illinois 60625 WTTW’s Geoffrey Baer, who each Friday night will welcome local contestants whose knowledge of trivia about our city will be put to the test. And on premiere night and after, visit Main Switchboard (773) 583-5000 wttw.com/quiz where you can play along at home. Turn to Member and Viewer Services page 4 for a behind-the-scenes interview with Geoffrey and (773) 509-1111 x 6 producer Eddie Griffin. We’ll also mark Women’s History Month with American Websites wttw.com Masters profiles of novelist Flannery O’Connor and wfmt.com choreographer Twyla Tharp; a POV documentary, And She Could Be Next, that explores a defiant movement of women of Publisher color transforming politics; and Not Done: Women Remaking Anne Gleason America, tracing the last five years of women’s fight for Art Director Tom Peth equality. On wttw.com, other Women’s History Month subjects include Emily Taft Douglas, WTTW Contributors a pioneering female Illinois politician, actress, and wife of Senator Paul Douglas who served Julia Maish in the U.S. House of Representatives; the past and present of Chicago’s Women’s Park and Lisa Tipton WFMT Contributors Gardens, designed by a team of female architects and featuring a statue by Louise Bourgeois; Andrea Lamoreaux and restaurateur Niquenya Collins and her newly launched Afro-Caribbean restaurant and catering business, Cocoa Chili. -

Looking for Therapeutic Antibodies in Next Generation Sequencing Repositories
bioRxiv preprint doi: https://doi.org/10.1101/572958; this version posted March 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Title: Looking for Therapeutic Antibodies in Next Generation Sequencing Repositories. Authors: Konrad Krawczyk1*, Matthew Raybould2, Aleksandr Kovaltsuk2, Charlotte M. Deane2 1 NaturalAntibody, Hamburg, Germany 2 Oxford University Department of Statistics, Oxford, UK *Correspondence to [email protected] Abstract: Recently it has become possible to query the great diversity of natural antibody repertoires using Next Generation Sequencing (NGS). These methods are capable of producing millions of sequences in a single experiment. Here we compare Clinical Stage Therapeutic antibodies to the ~1b sequences from 60 independent sequencing studies in the Observed Antibody Space Database. Of the 242 post Phase I antibodies, we find 16 with sequence identity matches of 95% or better for both heavy and light chains. There are also 54 perfect matches to therapeutic CDR-H3 regions in the NGS outputs, suggesting a nontrivial amount of convergence between naturally observed sequences and those developed artificially. This has potential implications for both the discovery of antibody therapeutics and the legal protection of commercial antibodies. Introduction Antibodies are proteins in jawed vertebrates that recognize noxious molecules (antigens) for elimination. An organism expresses millions of diverse antibodies to increase the chances that some of them will be able to bind the foreign antigen, initiating the adaptive immune response.