Immunology 101
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
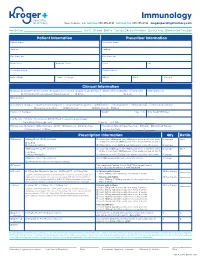
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

M.Tech. BT ( R14 Regulations)
M.Tech. BT ( R14 Regulations) CMR COLLEGE OF ENGINEERING & TECHNOLOGY (An Autonomous Institution) ACADEMIC REGULATIONS FOR M. TECH. (REGULAR) DEGREE COURSE Applicable for the students of M. Tech. (Regular) Course from the Academic Year 2014-15 and onwards The M. Tech. degree shall be conferred on candidates who are admitted to the program and who fulfil all the requirements for the award of the degree. 1.0 Eligibility for Admissions Admission to the above program shall be made subject to eligibility, qualification and specialization as prescribed by the State Government from time to time. 2.0 Award of M. Tech. degree 2.1 A student shall be declared eligible for the award of the M. Tech. Degree, if he pursues a course of study in not less than two and not more than four academic years. 2.2 A student, who fails to fulfill all the academic requirements for the award of the degree within four academic years from the year of his admission, shall forfeit his seat in M. Tech. course. 2.3 The student shall register for all 88 credits and secure all the 88 credits. 2.4 The minimum instruction days in each semester are 90. 2.5 The medium of instruction and examination shall be English. 3.0 A. Courses of Study The following specializations are offered at present for the M. Tech. course of study. 1. Bio-Technology 2. Embedded Systems 3. Power Electronics 4. Structural Engineering 5. Computer Science & Engineering 6. Machine Design and any other course as approved by the College/ University/AICTE from time to time. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Adaptive Tdetect Fact Sheet for Recipient
FACT SHEET FOR RECIPIENTS Coronavirus Adaptive Biotechnologies Corporation September 2, 2021 Disease 2019 T-Detect COVID Test (COVID-19) You are being given this Fact Sheet because your coughing, difficulty breathing, etc.). A full list of sample is being tested or was tested for an adaptive T- symptoms of COVID-19 can be found at the following cell immune response to the virus that causes link: https://www.cdc.gov/coronavirus/2019- Coronavirus Disease 2019 (COVID-19) using the T- ncov/symptoms-testing/symptoms.html. Detect COVID Test. How are people tested for COVID-19? Two main kinds of tests are currently available for You should not interpret the results of this COVID-19: diagnostic tests and adaptive immune response tests. test to indicate the presence or absence of immunity or protection from COVID-19 • A diagnostic test tells you if you have a current infection. infection. • An adaptive immune response test tells you if you may have had a previous infection This Fact Sheet contains information to help you understand the risks and benefits of using this test to What is the T-Detect COVID Test? evaluate your adaptive immune response to SARS-CoV- This test is similar to an antibody test in that it measures 2, the virus that causes COVID-19. After reading this your adaptive immune response to SARS-CoV-2, the Fact Sheet, if you have questions or would like to virus that causes COVID-19. However in this case it discuss the information provided, please talk to your specifically measures your adaptive T-cell immune healthcare provider. -

Gut Microbiome, Antibiotic Use, and Immunotherapy Responsiveness in Cancer
309 Editorial Commentary Page 1 of 4 Gut microbiome, antibiotic use, and immunotherapy responsiveness in cancer Jarred P. Reed, Suzanne Devkota, Robert A. Figlin Cedars-Sinai Medical Center, Los Angeles, CA, USA Correspondence to: Robert A. Figlin. Samuel Oschin Comprehensive Cancer Institute, Cedars-Sinai Medical Center, 8700 Beverly Blvd, Saperstein Critical Care Tower, C 2003, Los Angeles, CA 90048, USA. Email: [email protected]. Provenance: This is an invited article commissioned by the Section Editor Dr. Xiao Li (Department of Urology, Jiangsu Cancer Hospital, Jiangsu Institute of Cancer Research, Nanjing Medical University Affiliated Cancer Hospital, Nanjing, China). Comment on: Tinsley N, Zhou C, Tan G, et al. Cumulative Antibiotic Use Significantly Decreases Efficacy of Checkpoint Inhibitors in Patients with Advanced Cancer. Oncologist 2019. [Epub ahead of print]. Submitted Sep 27, 2019. Accepted for publication Oct 10, 2019. doi: 10.21037/atm.2019.10.27 View this article at: http://dx.doi.org/10.21037/atm.2019.10.27 Immune checkpoint inhibitors (ICIs) have transformed undergoing ICI treatment were reviewed for antibiotic the treatment of solid malignancies, but responses are exposure occurring within the time period two weeks heterogeneous with benefit generally limited to only before and six weeks after initiation of ICI therapy. Ninety- a fraction of patients. A number of factors have been two patients (32%) in the study received antibiotics. hypothesized to contribute to variability in ICI efficacy. Univariate analyses were performed to assess for significant Among these, a growing body of evidence points to a associations between patient characteristics and outcomes. critical role for the commensal gut microbiome, the Progression-free survival (PFS) was found to correlate with complex ecosystem of microorganisms living together antibiotic exposure, performance status, and comorbidity. -

Innate Immunity in the Lung: How Epithelial Cells Fight Against
Copyright #ERSJournals Ltd 2004 EurRespir J 2004;23: 327– 333 EuropeanRespiratory Journal DOI: 10.1183/09031936.03.00098803 ISSN0903-1936 Printedin UK –allrights reserved REVIEW Innateimmunity in the lung: how epithelialcells ght against respiratorypathogens R. Bals*,P.S. Hiemstra # Innateimmunity in the lung: how epithelial cells ® ghtagainst respiratory pathogens *Deptof Internal Medicine, Division of R Bals, P S Hiemstra #ERS JournalsLtd 2004 PulmonaryMedicine, Hospital of the Uni- versityof Marburg, Philipps-University, ABSTRACT: Thehuman lung is exposed to a largenumber of airborne pathogens as a # resultof the daily inhalation of 10,000 litres of air Theobservation that respiratory Marburg,Germany; Deptof Pulmonology, LeidenUniversity Medical Center, Leiden, infectionsare nevertheless rare is testimony to the presence of anef®cient host defence TheNetherlands systemat the mucosal surface of the lung Theairway epithelium is strategically positioned at the interface with the Correspondence:P S Hiemstra,Dept of environment,and thus plays a keyrole in this host defence system Recognition Pulmonology,Leiden University Medical systemsemployed by airwayepithelial cells to respond to microbialexposure include the Center, P O Box9600, 2300 RC Leiden, The actionof the toll-like receptors Netherlands Theairway epithelium responds to such exposure by increasing its production of Fax:31 715266927 mediatorssuch as cytokines, chemokines and antimicrobial peptides Recent® ndings E-mail: p s hiemstra@lumc nl indicatethe importance of these peptides -

The TNF-Family Cytokine TL1A Drives IL-13-Dependent Small Intestinal Inflammation
ARTICLES nature publishing group See ARTICLE page 186 The TNF-family cytokine TL1A drives IL-13-dependent small intestinal inflammation F M e y l a n 1 , 6 , Y - J S o n g 1 , 6 , I F u s s 2 , S V i l l a r r e a l 1 , E K a h l e 1 , I - J M a l m 1 , K A c h a r y a 1 , H L R a m o s 3 , L L o 4 , M M M e n t i n k - K a n e 5 , T A W y n n 5 , T - S M i g o n e 4 , W S t r o b e r 2 a n d R M S i e g e l 1 The tumor necrosis factor (TNF)-family cytokine TL1A (TNFSF15) costimulates T cells through its receptor DR3 (TNFRSF25) and is required for autoimmune pathology driven by diverse T-cell subsets. TL1A has been linked to human inflammatory bowel disease (IBD), but its pathogenic role is not known. We generated transgenic mice that constitutively express TL1A in T cells or dendritic cells. These mice spontaneously develop IL-13-dependent inflammatory small bowel pathology that strikingly resembles the intestinal response to nematode infections. These changes were dependent on the presence of a polyclonal T-cell receptor (TCR) repertoire, suggesting that they are driven by components in the intestinal flora. Forkhead box P3 (FoxP3)-positive regulatory T cells (Tregs) were present in increased numbers despite the fact that TL1A suppresses the generation of inducible Tregs. -

The Distribution of Immune Cells in the Uveal Tract of the Normal Eye
THE DISTRIBUTION OF IMMUNE CELLS IN THE UVEAL TRACT OF THE NORMAL EYE PAUL G. McMENAMIN Perth, Western Australia SUMMARY function of these cells in the normal iris, ciliary body Inflammatory and immune-mediated diseases of the and choroid. The role of such cell types in ocular eye are not purely the consequence of infiltrating inflammation, which will be discussed by other inflammatory cells but may be initiated or propagated authors in this issue, is not the major focus of this by immune cells which are resident or trafficking review; however, a few issues will be briefly through the normal eye. The uveal tract in particular considered where appropriate. is the major site of many such cells, including resident tissue macro phages, dendritic cells and mast cells. This MACRO PHAGES review considers the distribution and location of these and other cells in the iris, ciliary body and choroid in Mononuclear phagocytes arise from bone marrow the normal eye. The uveal tract contains rich networks precursors and after a brief journey in the blood as of both resident macrophages and MHe class 11+ monocytes immigrate into tissues to become macro dendritic cells. The latter appear strategically located to phages. In their mature form they are widely act as sentinels for capturing and sampling blood-borne distributed throughout the body. Macrophages are and intraocular antigens. Large numbers of mast cells professional phagocytes and play a pivotal role as are present in the choroid of most species but are effector cells in cell-mediated immunity and inflam virtually absent from the anterior uvea in many mation.1 In addition, due to their active secretion of a laboratory animals; however, the human iris does range of important biologically active molecules such contain mast cells. -

Development of Plasmacytoid and Conventional Dendritic Cell Subtypes from Single Precursor Cells Derived in Vitro and in Vivo
ARTICLES Development of plasmacytoid and conventional dendritic cell subtypes from single precursor cells derived in vitro and in vivo Shalin H Naik1,2, Priyanka Sathe1,3, Hae-Young Park1,4, Donald Metcalf1, Anna I Proietto1,3, Aleksander Dakic1, Sebastian Carotta1, Meredith O’Keeffe1,4, Melanie Bahlo1, Anthony Papenfuss1, Jong-Young Kwak1,4,LiWu1 & Ken Shortman1 The development of functionally specialized subtypes of dendritic cells (DCs) can be modeled through the culture of bone marrow with the ligand for the cytokine receptor Flt3. Such cultures produce DCs resembling spleen plasmacytoid DCs (pDCs), http://www.nature.com/natureimmunology CD8+ conventional DCs (cDCs) and CD8– cDCs. Here we isolated two sequential DC-committed precursor cells from such cultures: dividing ‘pro-DCs’, which gave rise to transitional ‘pre-DCs’ en route to differentiating into the three distinct DC subtypes (pDCs, CD8+ cDCs and CD8– cDCs). We also isolated an in vivo equivalent of the DC-committed pro-DC precursor cell, which also gave rise to the three DC subtypes. Clonal analysis of the progeny of individual pro-DC precursors demonstrated that some pro-DC precursors gave rise to all three DC subtypes, some produced cDCs but not pDCs, and some were fully committed to a single DC subtype. Thus, commitment to particular DC subtypes begins mainly at this pro-DC stage. Dendritic cells (DCs) are antigen-presenting cells crucial for the innate macrophages12. Further ‘downstream’, ‘immediate’ precursors have and adaptive response to infection as well as for maintaining immune been identified for several DC types, including Ly6Chi monocytes as 3,4,6 13 Nature Publishing Group Group Nature Publishing tolerance to self tissue. -

Natural Killer Cells Associated with SARS-Cov-2 Viral RNA Shedding
Bao et al. Exp Hematol Oncol (2021) 10:5 https://doi.org/10.1186/s40164-021-00199-1 Experimental Hematology & Oncology LETTER TO THE EDITOR Open Access Natural killer cells associated with SARS-CoV-2 viral RNA shedding, antibody response and mortality in COVID-19 patients Changqian Bao1†, Xiandong Tao2,3†, Wei Cui4†, Yuanyuan Hao1, Shuaike Zheng5, Bin Yi2,3, Tiewen Pan2, Ken H. Young6* and Wenbin Qian1,7* Abstract Coronavirus disease 2019 (COVID-19) is a novel infectious viral disease caused by the severe acute respiratory syn- drome coronavirus 2 (SARS-CoV-2). Two consecutively negative SARS-CoV-2 viral RNA test ( interval 24 hours), improved respiratory symptoms and obvious absorption of infammation in pulmonary imaging are≥ the discharge criteria for COVID-19 patients. The clearance profle of viral RNA in the upper respiratory tract specimens, including nasopharyngeal swab and/or oropharyngeal swabs, is related to innate immune cells such as Natural Killer cells. A total of 168 patients were included for the study. In this cohort, non-severe and severe groups showed signifcant dif- ferences in white blood cells, neutrophils, lymphocytes, basophils and platelets counts, as well as in infection related parameters such as CRP and serum cytokine IL-6. For lymphocyte subsets tests at admission, the severe group dis- played signifcantly lower cell counts than the non-severe group. Higher counts of total T cells, CD4 T cells, CD8 T cells, and NK cells in peripheral blood showed a signifcant correlation with the shorter time taken to+ obtain the frst+ negative viral RNA test and frst positive IgM/ IgG antibody test. -

Targeting Dendritic Cells with Antigen-Delivering Antibodies for Amelioration of Autoimmunity in Animal Models of Multiple Sclerosis and Other Autoimmune Diseases
antibodies Review Targeting Dendritic Cells with Antigen-Delivering Antibodies for Amelioration of Autoimmunity in Animal Models of Multiple Sclerosis and Other Autoimmune Diseases Courtney A. Iberg and Daniel Hawiger * Department of Molecular Microbiology and Immunology, Saint Louis University School of Medicine, Doisy Research Center, 1205 Carr Lane, St. Louis, MO 63104, USA; [email protected] * Correspondence: [email protected] Received: 31 March 2020; Accepted: 30 April 2020; Published: 15 June 2020 Abstract: The specific targeting of dendritic cells (DCs) using antigen-delivering antibodies has been established to be a highly efficient protocol for the induction of tolerance and protection from autoimmune processes in experimental autoimmune encephalomyelitis (EAE), a model of multiple sclerosis (MS), as well as in some other animal disease models. As the specific mechanisms of such induced tolerance are being investigated, the newly gained insights may also possibly help to design effective treatments for patients. Here we review approaches applied for the amelioration of autoimmunity in animal models based on antibody-mediated targeting of self-antigens to DCs. Further, we discuss relevant mechanisms of immunological tolerance that underlie such approaches, and we also offer some future perspectives for the application of similar methods in certain related disease settings such as transplantation. Keywords: dendritic cells; tolerance; antigen targeting; chimeric antibodies; autoimmunity; multiple sclerosis; diabetes 1. Introduction Over one hundred years ago, Paul Ehrlich coined the term “horror autotoxicus” to define an immune attack against an organism’s healthy tissues [1]. Since then, our knowledge of the complex mechanisms of the immune system as well as our understanding of the pathogenesis of specific autoimmune diseases have grown tremendously.