Primary Healthcare Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Jordan Project Pipeline
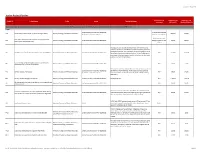
Last update: 14 February 2019 Jordan Project Pipeline USAID readiness Investment size Investment size Project ID Project name Entity Source Description/notes assessment (Million JD) Median (Million JD) This list only marks the initial effort at compiling and evaluating projects; the process will be continued by the Project Facility Unit at the PPDF with close collaboration with governmental entities and Ministries. Energy Jordan Economic Growth Plan 2018-2022 In market but contracts PP1 Generation of electric power by direct burning of waste Ministry of Energy and Mineral Resources 120-130 125.00 /Cabinet list of current projects have not been awarded Round 3 Renewable Expand the development of renewable energy projects for PP2 Ministry of Energy and Mineral Resources Jordan Economic Growth Plan 2018-2022 Energy Projects is in the 300.00 300.00 power generation (wind & solar) market The objective is to expand the Jordan Petroleum Refinery, since current production is not sufficient to meet the growing demand in the Jordanian market. The opportunity of converting the low value PP3 4th Expansion of Jordan Petroleum Refinery Company (JPRC) Ministry of Energy and Mineral Resources Jordan Economic Growth Plan 2018-2022 N/A 1,140.00 1,140.00 heavy fuel oil to more valuable products will allow the Refinery to cover most of the local demand, and this is the basis for the fourth expansion project of the Refinery. Use of 'energy storage through batteries' to reinforce the PP4 Ministry of Energy and Mineral Resources Jordan Economic Growth Plan 2018-2022 N/A 50.00 50.00 electrical grid and maintain its suitability. -

Amman, Jordan
MINISTRY OF WATER AND IRRIGATION WATER YEAR BOOK “Our Water situation forms a strategic challenge that cannot be ignored.” His Majesty Abdullah II bin Al-Hussein “I assure you that the young people of my generation do not lack the will to take action. On the contrary, they are the most aware of the challenges facing their homelands.” His Royal Highness Hussein bin Abdullah Imprint Water Yearbook Hydrological year 2016-2017 Amman, June 2018 Publisher Ministry of Water and Irrigation Water Authority of Jordan P.O. Box 2412-5012 Laboratories & Quality Affairs Amman 1118 Jordan P.O. Box 2412 T: +962 6 5652265 / +962 6 5652267 Amman 11183 Jordan F: +962 6 5652287 T: +962 6 5864361/2 I: www.mwi.gov.jo F: +962 6 5825275 I: www.waj.gov.jo Photos © Water Authority of Jordan – Labs & Quality Affairs © Federal Institute for Geosciences and Natural Resources Authors Thair Almomani, Safa’a Al Shraydeh, Hilda Shakhatreh, Razan Alroud, Ali Brezat, Adel Obayat, Ala’a Atyeh, Mohammad Almasri, Amani Alta’ani, Hiyam Sa’aydeh, Rania Shaaban, Refaat Bani Khalaf, Lama Saleh, Feda Massadeh, Samah Al-Salhi, Rebecca Bahls, Mohammed Alhyari, Mathias Toll, Klaus Holzner The Water Yearbook is available online through the web portal of the Ministry of Water and Irrigation. http://www.mwi.gov.jo Imprint This publication was developed within the German – Jordanian technical cooperation project “Groundwater Resources Management” funded by the German Federal Ministry for Economic Cooperation and Development (BMZ) Implemented by: Foreword It is highly evident and well known that water resources in Jordan are very scarce. -

World Bank Document
THE HASHEMITEKINGDOM OF JORDAN 664 M MINISTRYOF PUBLICWORKS AND HOUSING Public Disclosure Authorized E-233 VOL. 2 FEASIBILITYSTUDY FOR THE Public Disclosure Authorized 'AMMAN RING ROAD Public Disclosure Authorized Volume 2 Environmental Impact Assessment Public Disclosure Authorized DAR AL-HAN DASAhI DAR AL-HANDASAH insmadaNm.i w_na Cairo London. Skut An Jurn 1996 w1ss HASHEMITEKINGDOM OFJORDAN ~THE ,;vet M ~MINISTRYOF PUBLIC WORKS AND HOUSING ) FEASIBILITYSTU DY FOR THE M4rr L\. LI - Volume 2 Environmental Impact Assessment DAR AL-HANDASAH DAR AL-HANDASAH - - iinassociation with Manama Cairo London Beirut Amman J9760 June1998 Amman Rtn2 Road Phase I Table ol Contents TABLE OF CONTENTS 1. INTRODUCTION PAGE 1.1 Project Background 1.1 1.2 Study Components 1.1 1.3 Report Scope 1.2 1.4 Report Structure 1.2 2. PROJECT BACKGROUND AND PROJECT DESCRIPTION 2.1 Introduction 2.1 2.2 Project Status 2.1 2.3 Project Location 2.4 2.4 Project Proponent 2.7 2.5 Project Description 2.7 2.6 Design Standards and Guidelines 2.17 3. POLICY AND LEGAL FRAMEWORK 3.1 Introduction 3.1 3.2 Legislative Framework 3.1 3.3 Institutional Framework 3.4 3.4 Project Environmental Appraisal Framework 3.11 3.5 Project Planning Framework 3.14 4. BIOPHYSICAL ENVIRONMENT 4.1 Introduction 4.1 4.2 Climate 4.1 4.3 Geology and Seismology 4.6 4.4 Topography, Landform, Soils and Land Suitability 4.12 4.5 Flora and Fauna 4.25 4.6 Surface Water Resources 4.30 4.7 Groundwater Resources 4.34 4.8 Air Quality 4.39 4.9 Noise 4.41 4.10 Archaeology 4.45 4.11 Data Weaknesses 4.48 5. -

Impact of Syrian Refugees on the Jordanian Labour Market
Impact of Syrian refugees on the Jordanian labour market By Svein Erik Stave and Solveig Hillesund International Labour Organization Regional Office for the Arab States Aresco Center, Justinien Street, Kantari P.O.Box 11-4088 Riad El Solh 1107-2150 Beirut – Lebanon Tel: +961-1-752400 Fax: +961-1-752405 Email: [email protected] Website: www.ilo.org/arabstates Follow ILO in Arab States on Twitter: @iloarabic ISBN 9789221295839 ISBN 9789221295846 (web pdf) Fafo Borggata 2B/P.O.Box 2947 Tøyen NO-0608 Oslo www.fafo.no Fafo-report 2015:16 ISBN 978-82-324-0198-7 ISSN 0801-6143 20421-cover.indd 1 24.04.2015 09:21:47 Impact of Syrian refugees on the Jordanian labour market Findings from the governorates of Amman, Irbid and Mafraq By Svein Erik Stave and Solveig Hillesund International Labour Organization Regional Office for the Arab States and Fafo Copyright © International Labour Organization 2015 / Fafo 2015 First published 2015 Publications of the International Labour Office enjoy copyright under Protocol 2 of the Universal Copyright Convention. Nevertheless, short excerpts from them may be reproduced without authorization, on condition that the source is indicated. For rights of reproduction or transla- tion, application should be made to ILO Publications (Rights and Permissions), International Labour Office, CH-1211 Geneva 22, Switzerland, or by email: [email protected]. The International Labour Office welcomes such applications. Libraries, institutions and other users registered with reproduction rights organizations may make copies in accordance with the licen- ces issued to them for this purpose. Visit www.ifrro.org to find the reproduction rights organization in your country. -

Draft Outline
USAID Jordan Cities Implementing Transparent, Innovative, and Effective Solutions (USAID CITIES) Quarterly Progress Report Second Quarter FY 2018 – January 1 to March 31, 2018. Submission Date: April 15, 2018 Contract No.: AID-OAA-I-14-00062 Activity Start Date and End Date: September 25, 2016 to September 24, 2021 COR: George Kara’a Submitted by: Mark Grubb, Chief of Party Chemonics International Inc. This document was produced for review and approval by the United States Agency for International Development / Jordan (USAID/Jordan). July 2008 1 CONTENTS Contents ....................................................................................................................... 3 1. Activity Overview ............................................................................................. 7 a. Activity Details ............................................................................................................... 7 b. Executive Summary ....................................................................................................... 8 2. Sub-Purpose 1: Improved Service Delivery .............................................. 11 a. Key Accomplishments in Q2 ..................................................................................... 11 b. Upcoming Activities in Year 2 .................................................................................. 13 3. Sub-Purpose 2: Increased Sustainability of Local Government Operations ........................................................................................................................... -

Spatial Analysis of Health Centers in the Governorate of Amman, Jordan
Spatial Analysis of Health Centers in the Governorate of Amman, Jordan Mahmoud Abdullah Al-Habees*1 Abstract Objective: This study aimed at shedding light on the health centers in the Health Directorate of Amman, Jordan. That is, it explained the spatial analysis of the primary health centers in order to show the quantitative and qualitative spatial distribution of the existing health centers in the study area, analyze the spatial variation of the characteristics of the health centers, and introduce some recommendations allowing decision makers to make the optimal use of these health centers. Methods: This study adopted the inductive approach for the special and statistical properties of health services. The community consisted of all official health centers in the Health Directorate of Amman. There are 58 health centers that are comprehensive, primary, or secondary. The study used the appropriate statistical equations and methods appropriate to answer its specific questions. Results: The study concluded that there is a lack of medically qualified and specialized staff in the majority of health centers, and there is a considerable variation in the pattern of distribution of health centers in general. That is, the spatial distribution is concentrated to some urban areas. Besides that, the concentration ratio of health services indicates that the concentration ratio of the recipients of health services is not balanced with the concentration ratio of doctors. Keywords: Spatial analysis of health centers, the capital city. (J Med J 2013; Vol. 47 (1):44- 56) Received Accepted August 8, 2010 October 2, 2011 Introduction communities. Thus, the process of providing developed health services for those in need Investigating health services is of importance becomes a primary responsibility of in civilized societies and developed countries governments, which should provide them to since it assesses the government programs to their citizens.1 achieve the social and economic goals. -

“Ever-Growing Amman”, Jordan: Urban Expansion, Social
Habitat International 33 (2009) 81–92 Contents lists available at ScienceDirect Habitat International journal homepage: www.elsevier.com/locate/habitatint ‘‘Ever-growing Amman’’, Jordan: Urban expansion, social polarisation and contemporary urban planning issues Robert B. Potter a,*, Khadija Darmame a, Nasim Barham b, Stephen Nortcliff c a Department of Geography, School of Human and Environmental Sciences, University of Reading, Whiteknights, P.O. Box 227, Reading RG6 6NS, UK b Department of Geography, University of Jordan, Amman, Jordan c Department of Soil Science, School of Human and Environmental Sciences, University of Reading, Reading, UK abstract Keywords: Amman the primate capital city of the Hashemite Kingdom of Jordan currently has a population in excess Amman of 2 million, but in 1924 it consisted of little more than a collection of dwellings and some 2000–3000 Jordan inhabitants. The present paper sets out to document and explain the phenomenal expansion of ‘‘ever- Arab city growing Amman’’. The physical geography of the urban region and the early growth of the city are Urban growth considered at the outset and this leads directly to consideration of the highly polarised social structuring Urban social structure Urban transport that characterises contemporary Amman. In doing this, original data derived from the recent Greater Urban water supply Amman Municipality’s Geographical Information System are presented. In this respect, the essential Urban and regional planning modernity of the city is exemplified. The employment and industrial bases of the city and a range of Geopolitics pressing contemporary issues are then considered, including transport and congestion, the provision of urban water under conditions of water stress and privatisation, and urban and regional development planning for the city. -

TRANSPORT SECTOR Green Growth National Action Plan 2021-2025
TRANSPORT SECTOR Green Growth National Action Plan 2021-2025 Agriculture Energy WasteWater Tourism Transport ii Green Growth National Action Plan 2021-2025 Copyright © July 2020 This report should be referenced as follows: MoEnv. “Transport Sector Green Growth National Action Plan 2021-2025,” 2020. Amman, The Hashemite Kingdom of Jordan. Text from this report can be quoted provided the source is acknowledged. His Majesty King Abdullah II Ibn Al Hussein Economic leadership is by definition forward-looking. And forward-looking engagement will send a powerful message, a message of hope for my people and for yours. TRANSPORT SECTOR Green Growth National Action Plan 2021-2025 Agriculture Energy Waste Water Touris Transport v Transport Sector Foreword by the Minister of Environment Foreword by the Minister of Environment The Ministry of Environment has been taking While infrastructure investments and donor support solid action to support Jordan’s green growth will be critical to stabilize this risk, private sector Green Growth National transformation. In 2017, the Cabinet approved the investment in the green growth vision is equally National Green Growth Plan, which established important. In many ways, the world is already green growth as a top national priority. Jordan’s moving toward a greener future. The spread green growth vision – economic growth which is of renewable energy, electric transportation, Action Plan 2021-2025 environmentally sustainable and socially inclusive – technology that saves water and energy resources, puts a strong emphasis on the importance of building and innovations that promote the circular economy resilience. This is needed for our economy to be are taking off globally. -

Jordan Response Plan 2016-2018
HASHEMITE KINGDOM OF JORDAN MINISTRY OF PLANNING AND INTERNATIONAL COOPERATION JORDAN RESPONSE PLAN for the Syria Crisis 2016-2018 Table of Contents Acronyms ............................................................................................................................. 4 Executive Summary ............................................................................................................. 8 CHAPTER 1. Overview and Methodology ......................................................................... 14 1.1. Overview of Vulnerabilities and Needs ..................................................................... 14 1.2. International Assistance to Jordan ............................................................................. 19 1.3. JRP 2016 – 2018 Preparation Process ....................................................................... 20 1.4. Scope and Structure of the Plan ................................................................................. 23 1.5. Overview of JRP 2016-18 Sector Response Strategies ............................................. 29 CHAPTER 2. Sector Response Plans ................................................................................. 46 2.1 Introduction .................................................................................................................... 46 2.2. Response Plans by Sector ............................................................................................. 47 Chapter 3. Overall Impact of the Syria Crisis and Direct Budget Support -

Economic, Social, Political and Psychological Implications on Jordanian Women Married to Non-Jordanians and Their Families
FIELD STUDY Economic, Social, Political and Psychological Implications on Jordanian Women Married to Non-Jordanians and their Families Arab Women Organization of Jordan June 2010 Amman - Jordan Study Researcher Lamis Nasser ACKNOWLEGEMENTS The Arab Women Organization of Jordan thankfully acknowledges the assistance rendered by women organizations, development centres and municipal councils in various Governorates, for facilitating the implementation of this field study, specifically the ‘Musawa Network’ coordinators affiliated to the Arab Women Organization of Jordan, and the ‘United for Legal Equality’ Coalition members affiliated to the Human Forum for Women’s Rights. Special gratitude is extended to the following parties: Arab Women Society, Mafraq; Family Awareness and Counseling Centre, Zarka; Kufur Khil Municipality, Jerash; White Beds Society, Irbed; Jordanian Hashemite Fund for Human Development, Irbed; Khawla Bint Al-Azwar Society, Zarka; Women Programmes Centre, Zarka; Sharaka Centre for Democracy, Madaba; Princess Basma Community Centre, Jabal Al-Nuzha, Amman; Al-Naseem Municipality, Jerash; Rural Women Development and Rehabilitation Society, Amman; Women Society for Literacy, Amman; Women Cooperative Society, Salt. The Arab Women Organization of Jordan would also like to thank Researcher Lamis Nasser in appreciation of her efforts during all the stages of the field study. 2 FOREWORD This study is a qualitative and analytical field survey aimed at exploring the human experiences of Jordanian women married to non-Jordanian men, based on focus group discussions and face-to-face interviews with women groups at a number of Governorates, using a research tool specifically designed for this purpose. The study primarily aimed at providing decision-makers and politicians with realistic first-hand data from the field on the size and forms of suffering experienced by women and their families, to act as a research-informed tool for NGOs, experts and researchers in the field. -

Intention to Use Contraceptives in Jordan
Intention to Use Contraceptives in Jordan: Further Analysis of the Jordan Population and Family Health Survey 2017-18 DHS Further Analysis Reports No. 141 December 2020 This publication was produced for review by the United States Agency for International Development. It was prepared by Sara Riese. Further Analysis Reports No. 141 Intention to Use Contraceptives in Jordan: Further Analysis of the Jordan Population and Family Health Survey 2017-18 Sara Riese1,2 ICF Rockville, Maryland, USA December 2020 1 ICF 2 The DHS Program Corresponding author: Sara Riese, International Health and Development, ICF, 530 Gaither Road, Suite 500, Rockville, MD 20850, USA; phone: +1 301-572-0546; fax: +1 301-407-6501; email: [email protected] Acknowledgments: This study was supported by the USAID/Jordan. The USAID Mission in Jordan provided support and funding under the DHS-8 contract. Many thanks to my colleague, Christina Juan, for brainstorming and discussions during the Jordan Further Analysis report development process. Gratitude is extended to Shireen Assaf and Yodit Bekele for their thoughtful review and comments, as well as to our external reviewers, Hana Banat, John Callanta, and Samah Al-Quran. Editor: Diane Stoy Document Production: Natalie Shattuck This report presents findings from a further analysis of the 2017-18 Jordan Population and Family Health Survey (JPFHS). This report is a publication of The DHS Program which collects, analyzes, and disseminates data on fertility, family planning, maternal and child health, nutrition, and HIV/AIDS. Funding was provided by the U.S. Agency for International Development (USAID) through the DHS Program (#720-0AA-18C-00083). -

橡 Cover-Contents
2.5.5.2 Description of Selected System ( Activated Sludge Process)---------- MB2-51 2.5.5.3 Site of Treatment Plant------------------------------------------------------MB2-54 2.5.6 Effluent Disposal-----------------------------------------------------------------MB2-55 2.6 Operation and Maintenance Procedures----------------------------------------MB2-57 2.6.1 General----------------------------------------------------------------------------MB2-57 2.6.2 Sewerage System-----------------------------------------------------------------MB2-58 2.6.3 Treatment Facilities--------------------------------------------------------------MB2-59 2.7 Preliminary Cost Estimation-----------------------------------------------------MB2-60 2.7.1 Basic Assumptions and Unit Costs--------------------------------------------MB2-60 2.7.2 Investment Costs-----------------------------------------------------------------MB2-61 2.7.3 Operation and Maintenance Costs---------------------------------------------MB2-63 2.8 Economic and Financial Analysis-----------------------------------------------MB2-64 2.8.1 Socio-Economic Conditions----------------------------------------------------MB2-64 2.8.2 Economic and Financial Analysis---------------------------------------------MB2-65 2.8.3 Preparation of Projected Financial Statements-------------------------------MB2-68 2.9 Preliminary Implementation Plan-----------------------------------------------MB2-71 2.10 IEE for the Wadi Zarqa Wastewater Treatment Plant----------------------- MB2-71 2.10.1 Project Components