EHR) Has Become an Important Component of Documentation of the Medical Record
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -
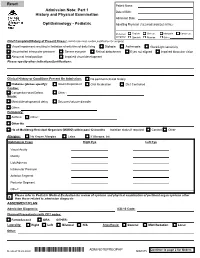
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019
Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019 Centers for Medicare & Medicaid Services PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is x. The time required to complete this information collection is estimated to average 0.3 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. This estimate does not include time for training. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. *****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Joan Proctor National Coordinator, Home Health Quality Reporting Program Centers for Medicare & Medicaid. OASIS-D Guidance Manual Table of Contents Page -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

Junior Doctor Skill in the Art of Physical Examination: a Retrospective Study of the Medical Admission Note Over Four Decades
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002257 on 3 April 2013. Downloaded from Junior doctor skill in the art of physical examination: a retrospective study of the medical admission note over four decades Charlotte M Oliver,1 Selena A Hunter,2 Takayoshi Ikeda,3 Duncan C Galletly2 To cite: Oliver CM, ABSTRACT et al ARTICLE SUMMARY Hunter SA, Ikeda T, . Objectives: To investigate the hypothesis that junior Junior doctor skill in the art doctors’ examination skills are deteriorating by assessing of physical examination: a Article focus the medical admission note examination record. retrospective study ▪ There is well-documented international evidence of the medical admission Design: Retrospective study of the admission record. supporting a declining standard in junior note over four decades. BMJ Setting: Tertiary care hospital. doctors’ physical examination skills in recent Open 2013;3:e002257. Methods: The admission records of 266 patients years. doi:10.1136/bmjopen-2012- admitted to Wellington hospital between 1975 and 2011 ▪ This study was conducted to address the 002257 were analysed, according to the total number of physical research question that this deterioration has examination observations (PEOtot), examination of the occurred locally in Wellington, New Zealand. ▸ Prepublication history for relevant system pertaining to the presenting complaint this paper are available (RelSystem) and the number of body systems examined Key messages ▪ There has been a decline in the quantity and online. To view these files (Nsystems). Subgroup analysis proceeded according to quality of the medical admission note examin- please visit the journal online admission year, level of experience of the admitting (http://dx.doi.org/10.1136/ ation records in this tertiary care centre between doctor (registrar, house surgeon (HS) and trainee intern bmjopen-2012-002257). -

Medical Record Rules and Regulations
New Hanover Regional Medical Center Rules and Regulations Medical Records Committee Review Function I. Preamble The medical record for each patient of this medical center should contain sufficient information as to identify the patient, support the diagnosis(es), justify the treatment, document the management and results as well as facilitate the continuity of care. Accordingly, the Medical Records Committee conducts quarterly analyses of medical records, or representative samples thereof, so as to assure the propriety and integrity of the medical records for the patients who seek treatment at this institution. This committee may initiate those action steps or recommendations in order to improve the timely completion, accuracy, and completeness of these records. II. Protection of the Medical Record All medical records are the property of the medical center (i.e. hospital) and are maintained for the benefit of each patient and for the healthcare providers. Records may be removed from the hospital’s jurisdiction only as pursuant to an appropriate court order, subpoena, or statute. In the case of re- admission of the patient, previous records may be available upon request for use of the attending physician. Except for current inpatients, all records which are removed from the Medical Records Department should be returned by 5 p.m. each day. III. General Medical Record Requirements All physician entries into the medical record (e.g. orders, notes, operative notes, history and physicals) shall be timed and dated. A legible identifier for services provided/ordered is requested. The method used shall be hand written or an electronic signature (stamp signatures are not acceptable) to sign an order or other medical record documentation. -

The Oral Presentation Nersi Nikakhtar, M.D
Guidelines for the Oral Presentation Nersi Nikakhtar, M.D. University of Minnesota Medical School !1 Table of Contents The Oral Presentation: An Introduction ..................................3 Why Worry About the Oral Presentation? ...............................4 Presenting the New Patient .....................................................5 The Opening Statement ......................................................5 History of Present Illness ....................................................5 Past Medical History ...........................................................6 Medications/Allergies ..........................................................7 Social and Family History ...................................................7 Review of Systems ..............................................................7 Vitals .....................................................................................8 Physical Exam .....................................................................8 Labs and Studies .................................................................8 Summary Statement ............................................................8 Assessment and Plan ..........................................................9 The Follow Up (or Daily) Presentation: What's Different? ...................................................................11 The Outpatient (Known Patient) Presentation: What's Different? ...................................................................12 !2 The Oral Presentation: An Introduction The -

The Value of the Physical Examination in Clinical Practice: an International Survey
ORIGINAL RESEARCH Clinical Medicine 2017 Vol 17, No 6: 490–8 T h e v a l u e o f t h e p h y s i c a l e x a m i n a t i o n i n c l i n i c a l p r a c t i c e : an international survey Authors: A n d r e w T E l d e r , A I C h r i s M c M a n u s ,B A l a n P a t r i c k , C K i c h u N a i r , D L o u e l l a V a u g h a n E a n d J a n e D a c r e F A structured online survey was used to establish the views of the act of physically examining a patient sits at the very heart 2,684 practising clinicians of all ages in multiple countries of the clinical encounter and is vital in establishing a healthy about the value of the physical examination in the contempo- therapeutic relationship with patients.7 Critics of the physical rary practice of internal medicine. 70% felt that physical exam- examination cite its variable reproducibility and the utility of ination was ‘almost always valuable’ in acute general medical more sensitive bedside tools, such as point of care ultrasound, ABSTRACT referrals. 66% of trainees felt that they were never observed by in place of traditional methods.2,8 a consultant when undertaking physical examination and 31% Amid this uncertainty, there is little published information that consultants never demonstrated their use of the physical describing clinicians’ opinions about the value of physical examination to them. -

The Patient Interview
CHAPTER 1 The Patient Interview Sneha Baxi Srivastava, PharmD, BCACP LEARNING OBJECTIVES • Explain the basic communication skills needed when performing a patient interview. • Describe the components of the patient interview. • Conduct a thorough medication history. • Compare and contrast the different patient interview approaches in various clinical settings. • Adapt the interview technique based on the needs of the patient. KEY TERMS • Active Listening • Pertinent Positive • Rapport • Pertinent Negative • Empathy • Past History • Open-Ended Questions • Medication History • Leading Questions • Family History • Probing Questions • Personal and Social History • Nonverbal Communication • Review of Systems • Chief Complaint • Physical Exam • History of Present Illness • QuEST/SCHOLAR-MAC INTRODUCTION The patient interview is the primary way of obtaining comprehensive information about the patient in order to provide effective patient-centered care, and the medica- tion history component is the pharmacist’s expertise. A methodological approach is used to obtain information from the patient, usually starting with determining the patient’s chief complaint, also known as the reason for the healthcare visit, and then 2 CHAPTER 1 / The Patient Interview delving further into an exploration of the patient’s specific complaint and problem. A comprehensive patient interview includes inquiring about the patient’s medical, medication, social, personal, and family history, as well as a thorough review of systems and possibly a physical examination. The medication history is the part of the patient interview that provides the pharmacist the opportunity to utilize his or her expertise by precisely collecting each component of the medication history (however, a medication history may also be collected independent of a comprehensive patient interview).