Assessment of Junior Doctors' Admission Notes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

New Patient Medical History Form
NEW PATIENT MEDICAL HISTORY FORM Full Name: Date: Birth Date: Age: ALLERGIES o NO ALLERGIES ALLERGY ALLERGIC REACTION MEDICATIONS MEDICATIONS DOSE TIMES PER DAY (Please list ALL) (Mg., pill, etc.) If you need more room to list medications, please write them on a blank sheet of paper with the required information HEALTH MAINTENANCE SCREENING TEST HISTORY CHolesterol Date: Facility/Provider: Abnormal Result? Y N Colonoscopy/SIGMOID Date: Facility/Provider: Abnormal Result? Y N Mammogram Date: Facility/Provider: Abnormal Result? Y N PAP SMEAR Date: Facility/Provider: Abnormal Result? Y N BONE density Date: Facility/Provider: Abnormal Result? Y N VACCINATION HISTORY Last Tetanus Booster or TdaP: Last Pnuemovax (Pneumonia): Last Flu Vaccine: Last Prevnar: Last Zoster Vaccine (Shingles): PERSONAL MEDICAL HISTORY DISEASE/CONDITION CURRENT PAST COMMENTS Alcoholism/Drug Abuse Asthma Cancer (type:_________________________________) Depression/Anxiety/Bipolar/Suicidal Diabetes (type:_______________________________) Emphysema (COPD) Heart Disease High Blood Pressure (hypertension) High Cholesterol Hypothyroidism/Thyroid Disease Renal (kidney) Disease Migraine Headaches Stroke Other: Other: SURGERIES TYPE (specify left/right) Date Location/Facility WOMEN’S HEALTH HISTORY Date of Last Menstrual Cycle: Age of First Menstruation: _____ Age of Menopause: _____ Total Number of Pregnancies: Number of Live Births: Pregnancy Complications: Patient Name: DOB: family MEDICAL HISTORY o NO Significant Family History IS KNOWN 4 CHECK ALL THat apply Stroke Cancer -
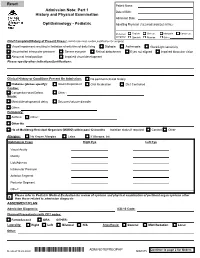
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Medical Staff Medical Record Policy
Number: MS -012 Effective Date: September 26, 2016 BO Revised:11/28/2016; 11/27/2017; 1/22/2018; 8/27/2018 CaroMont Regional Medical Center Author: Approved: Patrick Russo, MD, Chief-of-Staff Authorized: Todd Davis, MD, EVP, GMO MEDICAL STAFF MEDICAL RECORD POLICY 1. REQUIRED COMPONENTS OF THE MEDICAL RECORD The medical record shall include information to support the patient's diagnosis and condition, justify the patient's care, treatment and services, and document the course and result of the patient's care, and services to promote continuity of care among providers. The components may consist of the following: identification data, history and physical examination, consultations, clinical laboratory findings, radiology reports, procedure and anesthesia consents, medical or surgical treatment, operative report, pathological findings, progress notes, final diagnoses, condition on discharge, autopsy report when performed, other pertinent information and discharge summary. 2. ADMISSION HISTORY AND PHYSICAL EXAMINATION FOR HOSPITAL CARE Please refer to CaroMont Regional Medical Center Medical Staff Bylaws, Section 12.E. A. The history and physical examination (H&P), when required, shall be performed and recorded by a physician, dentist, podiatrist, or privileged practitioner who has an active NC license and has been granted privileges by the hospital. The H&P is the responsibility of the attending physician or designee. Oral surgeons, dentists, and podiatrists are responsible for the history and physical examination pertinent to their area of specialty. B. If a physician has delegated the responsibility of completing or updating an H&P to a privileged practitioner who has been granted privileges to do H&Ps, the H&P and/or update must be countersigned by the supervisor physician within 30 days after discharge to complete the medi_cal record. -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

Clinical Characteristics and Prognosis Of
Lyu et al. BMC Cardiovascular Disorders (2019) 19:209 https://doi.org/10.1186/s12872-019-1177-1 RESEARCH ARTICLE Open Access Clinical characteristics and prognosis of heart failure with mid-range ejection fraction: insights from a multi-centre registry study in China Lyu Siqi, Yu Litian* , Tan Huiqiong, Liu Shaoshuai, Liu Xiaoning, Guo Xiao and Zhu Jun Abstract Background: Heart failure (HF) with mid-range ejection fraction (EF) (HFmrEF) has attracted increasing attention in recent years. However, the understanding of HFmrEF remains limited, especially among Asian patients. Therefore, analysis of a Chinese HF registry was undertaken to explore the clinical characteristics and prognosis of HFmrEF. Methods: A total of 755 HF patients from a multi-centre registry were classified into three groups based on EF measured by echocardiogram at recruitment: HF with reduced EF (HFrEF) (n = 211), HFmrEF (n = 201), and HF with preserved EF (HFpEF) (n = 343). Clinical data were carefully collected and analyzed at baseline. The primary endpoint was all-cause mortality and cardiovascular mortality while the secondary endpoints included hospitalization due to HF and major adverse cardiac events (MACE) during 1-year follow-up. Cox regression and Logistic regression were performed to identify the association between the three EF strata and 1-year outcomes. Results: The prevalence of HFmrEF was 26.6% in the observed HF patients. Most of the clinical characteristics of HFmrEF were intermediate between HFrEF and HFpEF. But a significantly higher ratio of prior myocardial infarction (p = 0.002), ischemic heart disease etiology (p = 0.004), antiplatelet drug use (p = 0.009), angioplasty or stent implantation (p = 0.003) were observed in patients with HFmrEF patients than those with HFpEF and HFrEF. -

The Contribution of the Medical History for the Diagnosis of Simulated Cases by Medical Students
International Journal of Medical Education. 2012;3:78-82 ISSN: 2042-6372 DOI: 10.5116/ijme.4f8a.e48c The contribution of the medical history for the diagnosis of simulated cases by medical students Tomoko Tsukamoto, Yoshiyuki Ohira, Kazutaka Noda, Toshihiko Takada, Masatomi Ikusaka Department of General Medicine, Chiba University Hospital, Japan Correspondence: Tomoko Tsukamoto, Department of General Medicine, Chiba University Hospital, 1-8-1 Inohana, Chuo-ku, Chiba city, Chiba, 260-8677 Japan. Email: [email protected] Accepted: April 15, 2012 Abstract Objectives: The case history is an important part of diag- rates were compared using analysis of the χ2-test. nostic reasoning. The patient management problem method Results: Sixty students (63.8%) made a correct diagnosis, has been used in various studies, but may not reflect the which was based on the history in 43 students (71.7%), actual reasoning process because a list of choices is given to physical findings in 11 students (18.3%), and laboratory the subjects in advance. This study investigated the contri- data in 6 students (10.0%). Compared with students who bution of the history to making the correct diagnosis by considered the correct diagnosis in their differential diagno- using clinical case simulation, in which students obtained sis after taking a history, students who failed to do so were clinical information by themselves. 5.0 times (95%CI = 2.5-9.8) more likely to make a final Methods: A prospective study was conducted. Ninety-four misdiagnosis (χ2(1) = 30.73; p<0.001). fifth-year medical students from Chiba University who Conclusions: History taking is especially important for underwent supervised clinical clerkships in 2009 were making a correct diagnosis when students perform clinical surveyed. -

Junior Doctor Skill in the Art of Physical Examination: a Retrospective Study of the Medical Admission Note Over Four Decades
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002257 on 3 April 2013. Downloaded from Junior doctor skill in the art of physical examination: a retrospective study of the medical admission note over four decades Charlotte M Oliver,1 Selena A Hunter,2 Takayoshi Ikeda,3 Duncan C Galletly2 To cite: Oliver CM, ABSTRACT et al ARTICLE SUMMARY Hunter SA, Ikeda T, . Objectives: To investigate the hypothesis that junior Junior doctor skill in the art doctors’ examination skills are deteriorating by assessing of physical examination: a Article focus the medical admission note examination record. retrospective study ▪ There is well-documented international evidence of the medical admission Design: Retrospective study of the admission record. supporting a declining standard in junior note over four decades. BMJ Setting: Tertiary care hospital. doctors’ physical examination skills in recent Open 2013;3:e002257. Methods: The admission records of 266 patients years. doi:10.1136/bmjopen-2012- admitted to Wellington hospital between 1975 and 2011 ▪ This study was conducted to address the 002257 were analysed, according to the total number of physical research question that this deterioration has examination observations (PEOtot), examination of the occurred locally in Wellington, New Zealand. ▸ Prepublication history for relevant system pertaining to the presenting complaint this paper are available (RelSystem) and the number of body systems examined Key messages ▪ There has been a decline in the quantity and online. To view these files (Nsystems). Subgroup analysis proceeded according to quality of the medical admission note examin- please visit the journal online admission year, level of experience of the admitting (http://dx.doi.org/10.1136/ ation records in this tertiary care centre between doctor (registrar, house surgeon (HS) and trainee intern bmjopen-2012-002257). -

The History of Medicine a Beginner’S Guide
The History of Medicine A Beginner’s Guide Mark Jackson A Oneworld Paperback Published in North America, Great Britain & Australia by Oneworld Publications, 2014 Copyright © Mark Jackson 2014 The right of Mark Jackson to be identified as the Author of this work has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988 All rights reserved Copyright under Berne Convention A CIP record for this title is available from the British Library ISBN 978-1-78074-520-6 eISBN 978-1-78074-527-5 Typeset by Siliconchips Services Ltd, UK Printed and bound in Denmark by Nørhaven Oneworld Publications 10 Bloomsbury Street London WC1B 3SR England Stay up to date with the latest books, special offers, and exclusive content from Oneworld with our monthly newsletter Sign up on our website www.oneworld-publications.com For Ciara, Riordan and Conall ‘A heart is what a heart can do.’ Sir James Mackenzie, 1910 Contents List of illustrations viii Preface x Introduction xiii 1 Balance and flow: the ancient world 1 2 Regimen and religion: medieval medicine 25 3 Bodies and books: a medical Renaissance? 50 4 Hospitals and hope: the Enlightenment 84 5 Science and surgery: medicine in the nineteenth century 120 6 War and welfare: the modern world 159 Conclusion 197 Timeline 201 Further reading 214 Index 221 List of illustrations Figure 1 Chinese acupuncture chart Figure 2 Vessel for cupping (a form of blood-letting) discov- ered in Pompeii, dating from the first century CE Figure 3 Text and illustration on ‘urinomancy’ or urine analysis Figure 4 Mortuary crosses placed on the bodies of plague victims, c.