The Nose Embryology the Nose Developed from the Frontonasal Process
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
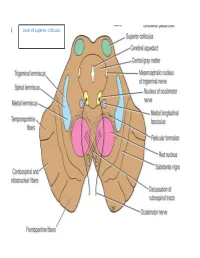
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -
Extracranial Course of Cranial Nerves
Extracranial course of cranial nerves Oculomotor, Trochlear, Abducent, Trigeminal, Facial and Accessory nerves Dr. Heba Kalbouneh Associate Professor of Anatomy and Histology Dr. Heba Kalbouneh Brainstem Mid brain Pons Medulla Pons Inferior view Facial nerve Anatomically, the course of the facial nerve can be divided into two parts: Motor: Innervates the muscles of facial Intracranial – the course of the nerve through expression, the posterior belly of the the cranial cavity, and the cranium itself. digastric, the stylohyoid and the stapedius Extracranial – the course of the nerve outside muscles. the cranium, through the face and neck. General Sensory: A small area around the concha of the auricle, EAM Special Sensory: Provides special taste sensation to the anterior 2/3 of the tongue. Parasympathetic: Supplies many of the glands of the head and neck, including: 1- Submandibular and sublingual salivary glands (via the submandibular ganglion/ chorda tympani) 2- Nasal, palatine and pharyngeal mucous glands (via the pterygopalatine ganglion/ greater petrosal) 3- Lacrimal glands (via the pterygopalatine ganglion/ greater petrosal) Dr. Heba Kalbouneh Intracranial course The nerve arises in the pons. It begins as two roots; a large motor root, and a small sensory root The two roots travel through the internal acoustic meatus. Pons Here, they are in very close proximity to the inner ear. 7th (motor) 8th Note: The part of the facial nerve that runs between the motor root of facial and vestibulocochlear nerve is sometimes Kalbouneh known as the nervus intermedius It contains the sensory and parasympathetic Heba fibers of the facial nerve Dr. Dr. Still within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -
![September 2008 [KT 1572] Sub](https://docslib.b-cdn.net/cover/8868/september-2008-kt-1572-sub-1478868.webp)
September 2008 [KT 1572] Sub
September 2008 [KT 1572] Sub. Code: 3115 DIPLOMA IN OTO-RHINO-LARYNGOLOGY EXAMINATION. Paper II – OTO-RHINO-LARYNGOLOGY INCLUDING AUDIOLOGY AND NEURO OTOLOGY (Candidates admitted upto 2003-2004 and Candidates admitted from 2004-2005 onwards) Q.P. Code : 353115 Time : Three hours Maximum : 100 marks Draw suitable diagram wherever necessary. Answer ALL questions. I. Essay questions : (2 X 20 = 40) 1. Discuss the etiology, clinical features and management epistaxis 2. Discuss the aetiopathogenesis, clinical features and managent of Post cricoid malignancy II. Write short notes on : (10 X 6 = 60) 1. Subglottic stenosis. 2. Otitic hydrocephalus. 3. Oroantral fistula. 4. Ennumerate ENT manifestations of AIDS. 5. Penetrating neck injuries. 6. Neoglottis. 7. Congenital cholesteatoma. 8. Prognostic tests for facial nerve palsy. 9. Puberphonia. 10. Cryosurgery in ENT diseases. ____________ MARCH -2009 [KU 1572] Sub. Code: 3115 DIPLOMA IN OTO-RHINO-LARYNGOLOGY EXAMINATION. Paper II – OTO-RHINO-LARYNGOLOGY INCLUDING AUDIOLOGY AND NEURO OTOLOGY (Common to all Regulations) Q.P. Code : 353115 Time : Three hours Maximum : 100 marks Draw suitable diagram wherever necessary. Answer ALL questions. I. Essay questions : (2 X 20 = 40) 1. Discuss the etiopathogenesis, clinical features and management of acoustic neuroma. 2. Describe the aetiology, clinical features and management of fungal sinusitis. II. Write short notes on : (10 X 6 = 60) 1. Stapedotomy. 2. Electronystagmography. 3. Vidian neurectomy. 4. CSF rhinorrhoea. 5. Blow out fracture. 6. Septal perforation. 7. Rhinophyma. 8. Perilymph fistula. 9. Tinnitus. 10. Tuberculous otitis media. ***** September - 2009 [KV 1572] Sub. Code: 3115 DIPLOMA IN OTO-RHINO-LARYNGOLOGY EXAMINATION. Paper II – OTO-RHINO-LARYNGOLOGY INCLUDING AUDIOLOGY AND NEURO OTOLOGY (Common to all Regulations) Q.P. -

NEUROANATOMY of the VISUAL PATHWAYS Magrane Basic Science Course June 2018
NEUROANATOMY OF THE VISUAL PATHWAYS Magrane Basic Science Course June 2018 **It is important for me to acknowledge the extensive input from Dr. Lola Hudson and Dr. Karen Munana to both these notes and the Power Point presentation.** CENTRAL NERVOUS SYSTEM All 5 divisions of the brain are involved with ocular function and/or adnexa in either conscious pathways or reflex pathways. The 5 divisions are the telencephalon (cerebral hemispheres), diencephalon (thalamus, hypothalamus), mesencephalon (midbrain), metencephalon (cerebellum and pons) and myelencephalon (medulla oblongata). The telencephalon and diencephalon together can be referred to as the prosencephalon (forebrain), and the metencephalon and myelencephalon can be referred to as the rhombencephalon (hindbrain). These 3 larger divisions (prosencephalon, mesencephalon and rhombencephalon) relate to the embryology of the brain from three original neural tube vesicles. The more cranial spinal cord is also involved with ocular function through sensory innervation into the cervical spinal cord and through sympathetic autonomic function particularly in the cranial thoracic spinal cord. PERIPHERAL NERVOUS SYSTEM The majority of the 12 pairs of cranial nerves (CN) have some involvement with ocular function: CNs II, III, IV, V (ophthalmic and maxillary branches), VI, VII and VIII including appropriate sensory and autonomic ganglia of these CNs. TELENCEPHALON (cerebrum=cerebral hemispheres=cerebral cortex) Telencephalon is the site of awareness, initiation of voluntary movements and perception of stimuli. The cerebrum functions in perception and integration of vision as well as voluntary control of eye/eyelid movements. The occipital lobes and the motor cortex of the frontal/parietal lobes are the primary regions involved in ocular and eyelid function. -

Clinical Anatomy of Greater Petrosal Nerve and Its Surgical Importance
[Downloaded free from http://www.indianjotol.org on Monday, August 18, 2014, IP: 218.241.189.21] || Click here to download free Android application for this journal ORIGINAL ARTICLE Clinical anatomy of greater petrosal nerve and its surgical importance Prashant E Natekar, Fatima M De Souza Department of Anatomy, Goa Medical College, Bambolim, Goa, India Background: Surgical approach towards greater petrosal nerve has to be done with caution as many surgeons ABSTRACT are unfamiliar with the anatomy of the facial nerve. The anatomical landmarks selected must be reliable and above all easy to identify for identification of the greater petrosal nerve so as to avoid injury to the structures in the middle cranial fossa. Observation and Results: The present study is carried out on 100 temporal bones by examining the following measurements of the right and the left sides a) length of the hiatus for grater petrosal superficial nerve b) distance from superior petrosal sinus c) distance from lateral margin of middle cranial fossa d) arcuate eminence and e) distance from exit to the foramen ovale. Conclusion: The anatomical landmarks selected must be reliable and above all easy to identify. Bony structures are more suitable than soft tissue or cartilaginous landmarks because of their rigid and reliable location. These anatomical landmarks will definitely help the surgeon while performing vidian nerve neurectomy and also the anatomical relationship of the facial nerve in temporal bone. The middle fossa approach involves a temporal craniotomy in cases of perineural spread of adenoid cystic carcinomas hence these anatomical landmarks will serve as useful guide for the surgeons and radiologists. -

Parasympathetic Nucleus of Facial Nerve
Neurology of Lacrimation Michael Davidson Professor, Ophthalmology Diplomate, American College of Veterinary Ophthalmologists Department of Clinical Sciences College of Veterinary Medicine North Carolina State University Raleigh, North Carolina, USA Trigeminal Nerve and Lacrimation Sensory afferent from lacrimal gland, adnexa, eye – through ophthalmic division and first branch of maxillary division (zygomatic n.) maxillary branch To trigeminal ganglion ophthalmic branch – adjacent to petrous temporal bone lateral to mandibular branch cavernous sinus near middle ear trigeminal ganglion Terminal branches of trigeminal n. trigeminal nerve distributes sympathetic and parasympathetic efferent to lacrimal gland and face Trigeminal-Lacrimal Reflex Afferent arm = CN V, ophthalmic division ⇒trigeminal ganglion ⇒ principle CN V nuclei Efferent arm = parasympathetic efferent to lacrimal gland(s) Elicits reflex tearing Parasympathetic efferent also supplies basal stimuli for lacrimation www.slideplayer.com Parasympathetic Efferent to Lacrimal Gland CN VII parasympathetic nuclei ⇒ greater petrosal nerve (petrous temporal bone) ⇒ nerve of pterygoid canal (with post ganglionic sympathetics) ⇒ synapse in pterygopalatine ganglion (ventral periorbital region, near apex of orbit) ⇒ zygomatic nerve (CN V, maxillary division)* ⇒ zygomaticotemporal nerve ⇒ acinar cells of lacrimal gland** *some texts state postganglionic parasympathetic fibers also in lacrimal nerve (ophthalmic division CNV) **postganglionic parasympathetic innervation to nictitans -

NASAL ANATOMY Elena Rizzo Riera R1 ORL HUSE NASAL ANATOMY
NASAL ANATOMY Elena Rizzo Riera R1 ORL HUSE NASAL ANATOMY The nose is a highly contoured pyramidal structure situated centrally in the face and it is composed by: ü Skin ü Mucosa ü Bone ü Cartilage ü Supporting tissue Topographic analysis 1. EXTERNAL NASAL ANATOMY § Skin § Soft tissue § Muscles § Blood vessels § Nerves ² Understanding variations in skin thickness is an essential aspect of reconstructive nasal surgery. ² Familiarity with blood supplyà local flaps. Individuality SKIN Aesthetic regions Thinner Thicker Ø Dorsum Ø Radix Ø Nostril margins Ø Nasal tip Ø Columella Ø Alae Surgical implications Surgical elevation of the nasal skin should be done in the plane just superficial to the underlying bony and cartilaginous nasal skeleton to prevent injury to the blood supply and to the nasal muscles. Excessive damage to the nasal muscles causes unwanted immobility of the nose during facial expression, so called mummified nose. SUBCUTANEOUS LAYER § Superficial fatty panniculus Adipose tissue and vertical fibres between deep dermis and fibromuscular layer. § Fibromuscular layer Nasal musculature and nasal SMAS § Deep fatty layer Contains the major superficial blood vessels and nerves. No fibrous fibres. § Periosteum/ perichondrium Provide nutrient blood flow to the nasal bones and cartilage MUSCLES § Greatest concentration of musclesàjunction of upper lateral and alar cartilages (muscular dilation and stenting of nasal valve). § Innervation: zygomaticotemporal branch of the facial nerve § Elevator muscles § Depressor muscles § Compressor -

Lecture 7 Anatomy the PTERYGOPALATINE FOSSA
د.احمد فاضل القيسي Lecture 7 Anatomy THE PTERYGOPALATINE FOSSA The pterygopalatine fossa lies beneath the posterior surface of the maxilla and the pterygoid process of the sphenoid bone. The pterygopalatine fossa contains the maxillary nerve, the maxillary artery (third part) and the pterygopalatine parasympathetic ganglion. Boundaries Anteriorly: posterior surface of maxilla. Posteriorly: anterior margin of pterygoid process below and greater wing of sphenoid above. Medially: perpendicular plate of palatine bone. Superiorly: greater wing of sphenoid. Laterally: communicates with infratemporal fossa through pterygomaxillary fissure Communications and openings: 1. The pterygomaxillary fissure: transmits the maxillary artery from the infratemporal fossa, the posterior superior alveolar branches of the maxillary division of the trigeminal nerve and the sphenopalatine veins. 2. The inferior orbital fissure: transmits the infraorbital and zygomatic branches of the maxillary nerve, the orbital branches of the pterygopalatine ganglion and the infraorbital vessels. 3. The foramen rotundum from the middle cranial fossa, occupying the greater wing of the sphenoid bone and transmit the maxillary division of the trigeminal nerve 4. The pterygoid canal from the region of the foramen lacerum at the base of the skull. The pterygoid canal transmits the greater petrosal and deep petrosal nerves (which combine to form the nerve of the pterygoid canal) and an accompanying artery derived from the maxillary artery. 5. The sphenopalatine foramen lying high up on the medial wall of the fossa.This foramen communicates with the lateral wall of the nasal cavity. It transmits the nasopalatine and posterior superior nasal nerves (from the pterygopalatine ganglion) and the sphenopalatine vessels. 6. The opening of a palatine canal found at the base of the fossa. -
Orbital Fractures
Vadim P. Nikolaenko Yury S. Astakhov Editors Orbital Fractures A Physician’s Manual 123 Orbital Fractures Vadim P. Nikolaenko • Yury S. Astakhov Editors Orbital Fractures A Physician's Manual Editors Vadim P. Nikolaenko, MD, PhD, DSc Yury S. Astakhov, MD, PhD, DSc Ophthalmology Ophthalmology Saint-Petersburg State Hospital No. 2 I.P. Pavlov First Saint Petersburg State Saint-Petersburg Medical University Russia Saint-Petersburg Russia Authorized translation of the 1st Russian language edition Orbital Fractures – A Physician’s Manual by Vadim P. Nikolaenko and Yury S. Astakhov © LLC Eco-Vektor, Saint-Petersburg, Russia, 2012, www.eco-vector.com All Rights Reserved ISBN 978-3-662-46207-2 ISBN 978-3-662-46208-9 (eBook) DOI 10.1007/978-3-662-46208-9 Library of Congress Control Number: 2015934822 Springer Heidelberg New York Dordrecht London © Springer-Verlag Berlin Heidelberg 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recita- tion, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or infor- mation storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publica- tion does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication.