European Position Paper on the Anatomical Terminology of the Internal Nose and Paranasal Sinuses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -
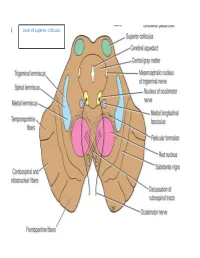
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Gross Anatomy Assignment Name: Olorunfemi Peace Toluwalase Matric No: 17/Mhs01/257 Dept: Mbbs Course: Gross Anatomy of Head and Neck
GROSS ANATOMY ASSIGNMENT NAME: OLORUNFEMI PEACE TOLUWALASE MATRIC NO: 17/MHS01/257 DEPT: MBBS COURSE: GROSS ANATOMY OF HEAD AND NECK QUESTION 1 Write an essay on the carvernous sinus. The cavernous sinuses are one of several drainage pathways for the brain that sits in the middle. In addition to receiving venous drainage from the brain, it also receives tributaries from parts of the face. STRUCTURE ➢ The cavernous sinuses are 1 cm wide cavities that extend a distance of 2 cm from the most posterior aspect of the orbit to the petrous part of the temporal bone. ➢ They are bilaterally paired collections of venous plexuses that sit on either side of the sphenoid bone. ➢ Although they are not truly trabeculated cavities like the corpora cavernosa of the penis, the numerous plexuses, however, give the cavities their characteristic sponge-like appearance. ➢ The cavernous sinus is roofed by an inner layer of dura matter that continues with the diaphragma sellae that covers the superior part of the pituitary gland. The roof of the sinus also has several other attachments. ➢ Anteriorly, it attaches to the anterior and middle clinoid processes, posteriorly it attaches to the tentorium (at its attachment to the posterior clinoid process). Part of the periosteum of the greater wing of the sphenoid bone forms the floor of the sinus. ➢ The body of the sphenoid acts as the medial wall of the sinus while the lateral wall is formed from the visceral part of the dura mater. CONTENTS The cavernous sinus contains the internal carotid artery and several cranial nerves. Abducens nerve (CN VI) traverses the sinus lateral to the internal carotid artery. -

Arteria Carotis Externa ACE External Carotid Artery
Common carotid artery CCA External Carotid artery ECA Internal carotid artery, ICA Subclavian artery SA and veins Ivo Klepáček ´tooth ache´ Salisbury cathedrale Three vascular systems are finally formed: Intraembryonic (cardinal); aortic sac (later gives rise aortic arches) Vitelline (aa. + vv.) Development of the vascular Placental system (umbilical Day 27 aa. + vv.) 1st – maxillary artery 2nd – hyoid, stapedial aa. 3rd – common carotid a. and first part of the internal carotid a., external carotid a. 4th – part of the subclavian aa. some of intersegmental arteries Common carotid artery Anterolaterally – skin, fascia, sternocleidomastoid muscle, sternohyoid, sternothyroid, superior belly of the omohyoid Posteriorly – transverse process of the C4 vertebrae, prevertebral muscles, sympathetic trunk Medially – wall of the pharynx and larynx, trachea, esophagus, the lobe of the thyroid gland Laterally – the internal jugular vein, vagus nerve (posterolaterally) Fascia pretrachealis a ACC Pretracheal fascia and ACC Sympathetic plexus surrounding arteries comes from sympathetic trunk External carotid artery ECA Anterolaterally – sternocleidomastoid muscle, XII. nerve, within parotid gland is crossed by VII. nerve, fascia, skin Medially – wall of the pharynx, internal carotid artery, stylopharyngeus, pharyngeal branch of the vagus For head without orbit, inner ear and brain Internal jugular Styloid vein lies septum dorsally and laterally from internal carotid artery behind m. m. stylohyoideus and styloglossus External carotid artery lies ventrally -

The Anatomy of Th-E Blood Vascular System of the Fox ,Squirrel
THE ANATOMY OF TH-E BLOOD VASCULAR SYSTEM OF THE FOX ,SQUIRREL. §CIURUS NlGER. .RUFIVENTEB (OEOEEROY) Thai: for the 009m of M. S. MICHIGAN STATE COLLEGE Thomas William Jenkins 1950 THulS' ifliillifllfllilllljllljIi\Ill\ljilllHliLlilHlLHl This is to certifg that the thesis entitled The Anatomy of the Blood Vascular System of the Fox Squirrel. Sciurus niger rufiventer (Geoffroy) presented by Thomas William Jenkins has been accepted towards fulfillment of the requirements for A degree in MEL Major professor Date May 23’ 19500 0-169 q/m Np” THE ANATOMY OF THE BLOOD VASCULAR SYSTEM OF THE FOX SQUIRREL, SCIURUS NIGER RUFIVENTER (GEOFFROY) By THOMAS WILLIAM JENKINS w L-Ooffi A THESIS Submitted to the School of Graduate Studies of Michigan State College of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Department of Zoology 1950 \ THESlSfi ACKNOWLEDGMENTS Grateful acknowledgment is made to the following persons of the Zoology Department: Dr. R. A. Fennell, under whose guidence this study was completed; Mr. P. A. Caraway, for his invaluable assistance in photography; Dr. D. W. Hayne and Mr. Poff, for their assistance in trapping; Dr. K. A. Stiles and Dr. R. H. Manville, for their helpful suggestions on various occasions; Mrs. Bernadette Henderson (Miss Mac), for her pleasant words of encouragement and advice; Dr. H. R. Hunt, head of the Zoology Department, for approval of the research problem; and Mr. N. J. Mizeres, for critically reading the manuscript. Special thanks is given to my wife for her assistance with the drawings and constant encouragement throughout the many months of work. -

Entrapment Neuropathy of the Central Nervous System. Part II. Cranial
Entrapment neuropathy of the Cranial nerves central nervous system. Part II. Cranial nerves 1-IV, VI-VIII, XII HAROLD I. MAGOUN, D.O., F.A.A.O. Denver, Colorado This article, the second in a series, significance because of possible embarrassment considers specific examples of by adjacent structures in that area. The same entrapment neuropathy. It discusses entrapment can occur en route to their desti- nation. sources of malfunction of the olfactory nerves ranging from the The first cranial nerve relatively rare anosmia to the common The olfactory nerves (I) arise from the nasal chronic nasal drip. The frequency of mucosa and send about twenty central proces- ocular defects in the population today ses through the cribriform plate of the ethmoid bone to the inferior surface of the olfactory attests to the vulnerability of the optic bulb. They are concerned only with the sense nerves. Certain areas traversed by of smell. Many normal people have difficulty in each oculomotor nerve are pointed out identifying definite odors although they can as potential trouble spots. It is seen perceive them. This is not of real concern. The how the trochlear nerves are subject total loss of smell, or anosmia, is the significant to tension, pressure, or stress from abnormality. It may be due to a considerable variety of causes from arteriosclerosis to tu- trauma to various bony components morous growths but there is another cause of the skull. Finally, structural which is not usually considered. influences on the abducens, facial, The cribriform plate fits within the ethmoid acoustic, and hypoglossal nerves notch between the orbital plates of the frontal are explored. -

Annual Meeting in Tulsa (Hosted by Elmus Beale) on June 11-15, 2019, We Were All Energized
37th ANNUAL Virtual Meeting 2020 June 15-19 President’s Report June 15-19, 2020 Virtual Meeting #AACA Strong Due to the unprecedented COVID-19 pandemic, our 2020 annual AACA meeting in June 15-19 at Weill Cornell in New York City has been canceled. While this is disappointing on many levels, it was an obvious decision (a no brainer for this neurosurgeon) given the current situation and the need to be safe. These past few weeks have been stressful and uncertain for our society, but for all of us personally, professionally and collectively. Through adversity comes opportunity: how we choose to react to this challenge will determine our future. Coming away from the 36th Annual meeting in Tulsa (hosted by Elmus Beale) on June 11-15, 2019, we were all energized. An informative inaugural newsletter edited by Mohammed Khalil was launched in the summer. In the fall, Christina Lewis hosted a successful regional meeting (Augmented Approaches for Incorporating Clinical Anatomy into Education, Research, and Informed Therapeutic Management) with an excellent faculty and nearly 50 attendees at Samuel Merritt University in Oakland, CA. The midyear council meeting was coordinated to overlap with that regional meeting to show solidarity. During the following months, plans for the 2020 New York meeting were well in motion. COVID-19 then surfaced: first with its ripple effect and then its storm. Other societies’ meetings - including AAA and EB – were canceled and outreach to them was extended for them to attend our meeting later in the year. Unfortunately, we subsequently had to cancel the plans for NY. -

An Endoscopic Study on the Prevalence of the Accessory Maxillary Ostium in Chronic Sinusitis Patients
International Journal of Otorhinolaryngology and Head and Neck Surgery Varadharajan R et al. Int J Otorhinolaryngol Head Neck Surg. 2020 Jan;6(1):40-44 http://www.ijorl.com pISSN 2454-5929 | eISSN 2454-5937 DOI: http://dx.doi.org/10.18203/issn.2454-5929.ijohns20195211 Original Research Article An endoscopic study on the prevalence of the accessory maxillary ostium in chronic sinusitis patients Ramesh Varadharajan*, Swara Sahithya, Ranjitha Venkatesan, Agaman Gunasekaran, Sneha Suresh Department of Otorhinolaryngology and Head and Neck Surgery , Aarupadai Veedu Medical College and Hospital, Kirumampakkam, Puducherry, India Received: 21 October 2019 Revised: 07 November 2019 Accepted: 08 November 2019 *Correspondence: Dr. Ramesh Varadharajan, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Chronic maxillary sinusitis is one of the common ENT problems. Accessory maxillary ostium (AMO) has been postulated in many publications to play a role in the development of chronic maxillary sinusitis. AMO is found in the medial wall of maxillary sinus and located in the lateral wall of the nose. It’s been frequently identified in the routine nasal endoscopy. The variations in the location of AMO have been evaluated by nasal endoscopy in live subjects or through cadaver dissections by many authors. This live study is conducted to identify the prevalence of AMO during nasal endoscopic evaluation of chronic sinusitis patients. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

A New Radiological Classification for the Risk Assessment of Anterior Skull
www.nature.com/scientificreports OPEN A new radiological classifcation for the risk assessment of anterior skull base injury in endoscopic sinus surgery Baharudin Abdullah 1*, Shiun Chuen Chew1, Mohd Ezane Aziz2, Norasnieda Md Shukri1, Salina Husain3, Sng Weirong Joshua4, De Yun Wang4 & Kornkiat Snidvongs5 Keros and Gera classifcations are widely used to assess the risk of skull base injury during endoscopic sinus surgery. Although, both classifcations are useful preoperatively to stratify risk of patients going for surgery, it is not practical to measure the respective lengths during surgery. In this study, we aimed to propose a new radiological classifcation (Thailand-Malaysia-Singapore (TMS)) to assess the anatomical risk of anterior skull base injury using the orbital foor (OF) as a reference. A total of 150 computed tomography images of paranasal sinuses (300 sides) were reviewed. The TMS classifcation was categorized into 3 types by measuring OF to cribriform plate and OF to ethmoid roof. Most patients were classifed as TMS type 1, Keros type 2 and Gera class II, followed by patients classifed as TMS type 3, Keros type 1 and Gera class 1. TMS has signifcant correlation with Keros classifcation (p < 0.05). There was no signifcant correlation between Keros and Gera classifcations (p = 0.33) and between TMS and Gera classifcations (p = 0.80). The TMS classifcation has potential to be used for risk assessment of skull base injury among patients undergoing ESS. It serves as an additional assessment besides the Keros and Gera classifcations. Endoscopic sinus surgery (ESS) has an overall complication rate of 0.5% with the specifc complications of cere- brospinal fuid leak, orbital injury, haemorrhage requiring surgery, blood transfusion and toxic shock syndrome at 0.09%, 0.09%, 0.10%, 0.18%, and 0.02%, respectively1. -

Chapter 2 Implants and Oral Anatomy
Chapter 2 Implants and oral anatomy Associate Professor of Maxillofacial Anatomy Section, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University Tatsuo Terashima In recent years, the development of new materials and improvements in the operative methods used for implants have led to remarkable progress in the field of dental surgery. These methods have been applied widely in clinical practice. The development of computerized medical imaging technologies such as X-ray computed tomography have allowed detailed 3D-analysis of medical conditions, resulting in a dramatic improvement in the success rates of operative intervention. For treatment with a dental implant to be successful, it is however critical to have full knowledge and understanding of the fundamental anatomical structures of the oral and maxillofacial regions. In addition, it is necessary to understand variations in the topographic and anatomical structures among individuals, with age, and with pathological conditions. This chapter will discuss the basic structure of the oral cavity in relation to implant treatment. I. Osteology of the oral area The oral cavity is composed of the maxilla that is in contact with the cranial bone, palatine bone, the mobile mandible, and the hyoid bone. The maxilla and the palatine bones articulate with the cranial bone. The mandible articulates with the temporal bone through the temporomandibular joint (TMJ). The hyoid bone is suspended from the cranium and the mandible by the suprahyoid and infrahyoid muscles. The formation of the basis of the oral cavity by these bones and the associated muscles makes it possible for the oral cavity to perform its various functions. -

Appendix-A-Osteology-V-2.0.Pdf
EXPLORATIONS: AN OPEN INVITATION TO BIOLOGICAL ANTHROPOLOGY Editors: Beth Shook, Katie Nelson, Kelsie Aguilera and Lara Braff American Anthropological Association Arlington, VA 2019 Explorations: An Open Invitation to Biological Anthropology is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, except where otherwise noted. ISBN – 978-1-931303-63-7 www.explorations.americananthro.org Appendix A. Osteology Jason M. Organ, Ph.D., Indiana University School of Medicine Jessica N. Byram, Ph.D., Indiana University School of Medicine Learning Objectives • Identify anatomical position and anatomical planes, and use directional terms to describe relative positions of bones • Describe the gross structure and microstructure of bone as it relates to bone function • Describe types of bone formation and remodeling, and identify (by name) all of the bones of the human skeleton • Distinguish major bony features of the human skeleton like muscle attachment sites and passages for nerves and/or arteries and veins • Identify the bony features relevant to estimating age, sex, and ancestry in forensic and bioarchaeological contexts • Compare human and chimpanzee skeletal anatomy Anthropology is the study of people, and the skeleton is the framework of the person. So while all subdisciplines of anthropology study human behavior (culture, language, etc.) either presently or in the past, biological anthropology is the only subdiscipline that studies the human body specifically. And the fundamental core of the human (or any vertebrate) body is the skeleton. Osteology, or the study of bones, is central to biological anthropology because a solid foundation in osteology makes it possible to understand all sorts of aspects of how people have lived and evolved.