Arteria Carotis Externa ACE External Carotid Artery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of Th-E Blood Vascular System of the Fox ,Squirrel
THE ANATOMY OF TH-E BLOOD VASCULAR SYSTEM OF THE FOX ,SQUIRREL. §CIURUS NlGER. .RUFIVENTEB (OEOEEROY) Thai: for the 009m of M. S. MICHIGAN STATE COLLEGE Thomas William Jenkins 1950 THulS' ifliillifllfllilllljllljIi\Ill\ljilllHliLlilHlLHl This is to certifg that the thesis entitled The Anatomy of the Blood Vascular System of the Fox Squirrel. Sciurus niger rufiventer (Geoffroy) presented by Thomas William Jenkins has been accepted towards fulfillment of the requirements for A degree in MEL Major professor Date May 23’ 19500 0-169 q/m Np” THE ANATOMY OF THE BLOOD VASCULAR SYSTEM OF THE FOX SQUIRREL, SCIURUS NIGER RUFIVENTER (GEOFFROY) By THOMAS WILLIAM JENKINS w L-Ooffi A THESIS Submitted to the School of Graduate Studies of Michigan State College of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Department of Zoology 1950 \ THESlSfi ACKNOWLEDGMENTS Grateful acknowledgment is made to the following persons of the Zoology Department: Dr. R. A. Fennell, under whose guidence this study was completed; Mr. P. A. Caraway, for his invaluable assistance in photography; Dr. D. W. Hayne and Mr. Poff, for their assistance in trapping; Dr. K. A. Stiles and Dr. R. H. Manville, for their helpful suggestions on various occasions; Mrs. Bernadette Henderson (Miss Mac), for her pleasant words of encouragement and advice; Dr. H. R. Hunt, head of the Zoology Department, for approval of the research problem; and Mr. N. J. Mizeres, for critically reading the manuscript. Special thanks is given to my wife for her assistance with the drawings and constant encouragement throughout the many months of work. -

Variant Position of the Facial Nerve in Parotid Gland
eISSN 1308-4038 International Journal of Anatomical Variations (2011) 4: 3–4 Case Report Variant position of the facial nerve in parotid gland Published online January 14th, 2011 © http://www.ijav.org Rajesh B. ASTIK ABSTRACT Urvi H. DAVE The division of the parotid gland into superficial and deep lobes by facial nerve has an important implication in parotid Krishna Swami GAJENDRA gland neoplasm. This plane is used in superficial or total parotidectomy to avoid damage to the facial nerve. During routine dissection in the Department of Anatomy, we found variably located facial nerve in the parotid gland of the left side. The main trunk of the facial nerve was located between maxillary vein and superficial temporal vein. It was divided into temporofacial and cervicofacial divisions. Both divisions crossed maxillary vein superficially instead Department of Anatomy, GSL Medical College, Rajahmundry, District- East Godavari, of retromandibular vein which was formed outside the parotid gland substance. Andhra Pradesh, INDIA. The operating surgeon should be familiar with this variation during parotidectomy to reduce the iatrogenic injury to the facial nerve. © IJAV. 2011; 4: 3–4. Dr. Rajesh B. Astik Associate Professor Department of Anatomy GSL Medical College NH-5, Rajahmundry District- East Godavari. Andhra Pradesh, 533296, INDIA. +91 883 2484999 [email protected] Received July 15th, 2010; accepted January 4th, 2011 Key words [facial nerve] [parotid gland] [retromandibular vein] [total parotidectomy] Introduction vein superficially instead of the retromandibular vein. The The retromandibular vein is formed by union of the maxillary retromandibular vein was formed by union of maxillary and and superficial temporal veins in the parotid gland [1]. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

The Development of Mammalian Dural Venous Sinuses with Especial Reference to the Post-Glenoid Vein
J. Anat. (1967), 102, 1, pp. 33-56 33 With 12 figures Printed in Great Britian The development of mammalian dural venous sinuses with especial reference to the post-glenoid vein H. BUTLER Department ofAnatomy, University of Saskatchewan, Saskatoon, Canada The intracranial venous outflow of mammals drains into both the internal and external jugular veins and the relative role of these two veins varies between different adult mammals as well as at different phases of embryonic and foetal life. In general, the primary head vein (consisting of venae capitis medialis and lateralis and their tributaries) gives rise to the dural venous sinuses which drain into the anterior cardinal vein (the future internal jugular vein). The external jugular veins appear as the face and jaws develop but, at all times, the two venous systems freely com- municate with each other. Morphologically, as shown by Sutton (1888), both the dural venous sinuses and the external jugular venous system are extracranial in so far as they are situated outside the dura mater. The chondrocranium and the dermocranium, however, develop in between the dural venous sinuses and the external jugular vein system (Butler, 1957). Thus, in the adult mammal, the bony skull wall separates the two venous systems, and therefore the dural venous sinuses are topographically intracranial whereas the external jugular venous system is extracranial. Furthermore the development of the skull localizes the connexions between the dural venous sinuses and the external jugular venous system to the various fontanelles and neuro-vascular foramina to form the emissary veins. The post-glenoid vein is one of the more important and controversial emissary veins since its presence or absence has been used in attempts to establish mammalian phylogenetic relationships (van Gelderen, 1925; Boyd, 1930). -
27. Veins of the Head and Neck
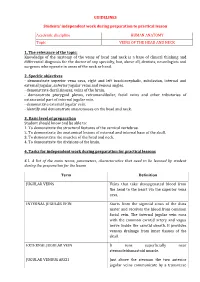
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

Atlas of Topographical and Pathotopographical Anatomy of The
Contents Cover Title page Copyright page About the Author Introduction Part 1: The Head Topographic Anatomy of the Head Cerebral Cranium Basis Cranii Interna The Brain Surgical Anatomy of Congenital Disorders Pathotopography of the Cerebral Part of the Head Facial Head Region The Lymphatic System of the Head Congenital Face Disorders Pathotopography of Facial Part of the Head Part 2: The Neck Topographic Anatomy of the Neck Fasciae, Superficial and Deep Cellular Spaces and their Relationship with Spaces Adjacent Regions (Fig. 37) Reflex Zones Triangles of the Neck Organs of the Neck (Fig. 50–51) Pathography of the Neck Topography of the neck Appendix A Appendix B End User License Agreement Guide 1. Cover 2. Copyright 3. Contents 4. Begin Reading List of Illustrations Chapter 1 Figure 1 Vessels and nerves of the head. Figure 2 Layers of the frontal-parietal-occipital area. Figure 3 Regio temporalis. Figure 4 Mastoid process with Shipo’s triangle. Figure 5 Inner cranium base. Figure 6 Medial section of head and neck Figure 7 Branches of trigeminal nerve Figure 8 Scheme of head skin innervation. Figure 9 Superficial head formations. Figure 10 Branches of the facial nerve Figure 11 Cerebral vessels. MRI. Figure 12 Cerebral vessels. Figure 13 Dural venous sinuses Figure 14 Dural venous sinuses. MRI. Figure 15 Dural venous sinuses Figure 16 Venous sinuses of the dura mater Figure 17 Bleeding in the brain due to rupture of the aneurism Figure 18 Types of intracranial hemorrhage Figure 19 Different types of brain hematomas Figure 20 Orbital muscles, vessels and nerves. Topdown view, Figure 21 Orbital muscles, vessels and nerves. -

Transvenous Embolization of a Direct Carotid Cavernous Fistula Through the Pterygoid Plexus
AJNR Am J Neuroradiol 23:1156–1159, August 2002 Case Report Transvenous Embolization of a Direct Carotid Cavernous Fistula through the Pterygoid Plexus Galen F.H. Chun and Thomas A. Tomsick Summary: Closure of a direct carotid cavernous fistula beyond a relatively acutely angulated posterior genu (Fig 1). with detachable coils by transpterygoid venous approach to No aneurysm was identified. Venous effluence was through the the cavernous sinus is an alternative technique that may be superior ophthalmic vein, attenuated anteromedially with small applied in cases in which other techniques offer increased connection to the left nasal vein, right nasal and right angular veins, and a single transforaminal channel to the pterygoid risk or in which other techniques have failed. In this case plexus. Venous-phase angiography over the face and neck report, we present the details of the management of a direct showed the pterygoid plexus, maxillary vein, and both the facial carotid cavernous fistula by this method. and retromandibular veins draining the fistula (Fig 2). An 80-cm 8F Bright Tip (Cordis Endovascular Systems, Miami Lakes, FL) guide catheter was passed coaxially with a 5F The efficacy and safety of detachable balloon oc- H1 catheter over a 0.035-inch Glidewire (Boston Scientific, clusion of direct carotid cavernous fistulas are well Natick, MA) into the left common carotid artery via the left established (1). However, detachable balloon tech- common femoral artery. A medium-detachment-pressure niques have required occlusion of the internal carotid 0.5-cc detachable silicone balloon (Target Therapeutics, Fre- artery (ICA) in a substantial percentage of patients mont, CA), attached to a heat-shaped Tracker-18 catheter (2–4). -

7. Internal Jugular Vein the Internal Jugular Vein Is a Large Vein That Receives Blood from the Brain, Face, and Neck
د.احمد فاضل Lecture 16 Anatomy The Root of the Neck The root of the neck can be defined as the area of the neck immediately above the inlet into the thorax. Muscles of the Root of the Neck Scalenus Anterior Muscle Scalenus Medius Muscle The Thoracic Duct The thoracic duct begins in the abdomen at the upper end of the cisterna chyli. It enters the thorax through the aortic opening in the diaphragm and ascends upward, inclining gradually to the left. On reaching the superior mediastinum, it is found passing upward along the left margin of the esophagus. At the root of the neck, it continues to ascend along the left margin of the esophagus until it reaches the level of the transverse process of the seventh cervical vertebra. Here, it bends laterally behind the carotid sheath. On reaching the medial border of the scalenus anterior, it turns 1 downward and drains into the beginning of the left brachiocephalic vein. It may, however, end in the terminal part of the subclavian or internal jugular veins. Main Nerves of the Neck Cervical Plexus Brachial Plexus The brachial plexus is formed in the posterior triangle of the neck by the union of the anterior rami of the 5th, 6th, 7th, and 8th cervical and the first thoracic spinal nerves. This plexus is divided into roots, trunks, divisions, and cords. The roots of C5 and 6 unite to form the upper trunk, the root of C7 continues as the middle trunk, and the roots of C8 and T1 unite to form the lower trunk. -

Vascularization of Air Sinuses and Fat Bodies in the Head of the Bottlenose Dolphin (Tursiops Truncatus): Morphological Implications on Physiology
ORIGINAL RESEARCH ARTICLE published: 04 July 2012 doi: 10.3389/fphys.2012.00243 Vascularization of air sinuses and fat bodies in the head of the Bottlenose dolphin (Tursiops truncatus): morphological implications on physiology Alex Costidis 1* and Sentiel A. Rommel 2 1 Aquatic Animal Health Program, Department of Physiological Sciences, College of Veterinary Medicine, University of Florida, Gainesville, FL, USA 2 Biology and Marine Biology, University of North Carolina Wilmington, Wilmington, NC, USA Edited by: Cetaceans have long been considered capable of limiting diving-induced nitrogen absorp- Andreas Fahlman, Texas A&M Corpus tion and subsequent decompression sickness through a series of behavioral, anatomical, Christi, USA and physiological adaptations. Recent studies however suggest that in some situations Reviewed by: Yara Bernaldo De Quiros, University of these adaptive mechanisms might be overcome, resulting in lethal and sublethal injuries. Las Palmas de Gran Canaria, Spain Perhaps most relevant to this discussion is the finding of intravascular gas and fat emboli James G. Mead, National Museum of in mass-stranded beaked whales. Although the source of the gas emboli has as yet to Natural History, Smithsonian been ascertained, preliminary findings suggest nitrogen is the primary component. Since Institution, USA nitrogen gas embolus formation in divers is linked to nitrogen saturation, it seems prema- *Correspondence: Alex Costidis, Department of ture to dismiss similar pathogenic mechanisms in breath-hold diving cetaceans. Due to the Physiological Sciences, College of various anatomical adaptations in cetacean lungs, the pulmonary system is thought of as Veterinary Medicine, University of an unlikely site of significant nitrogen absorption. The accessory sinus system on the ven- Florida, 1600 Southwest Archer Road, tral head of odontocete cetaceans contains a sizeable volume of air that is exposed to the Box 100144, Gainesville, FL 32610, USA. -

European Position Paper on the Anatomical Terminology of the Internal Nose and Paranasal Sinuses
ISSN: 03000729 INTERN AT IO N A L R H I N CONTENT O L O G I C Official Journal of the European and International Societies Position paper Lund VJ, Stammberger H, Fokkens WJ, Beale T, Bernal-Sprekelsen M, Eloy P, Georgalas C, Ger- S O C I E Y stenberger C, Hellings PW, Herman P, Hosemann WG, Jankowski R, Jones N, Jorissen M, Leunig T A, Onerci M, Rimmer J, Rombaux P, Simmen D, Tomazic PV, Tschabitscher M, Welge-Luessen A. European Position Paper on the Anatomical Terminology of the Internal Nose and Parana- VOLUME 50 | SUPPLEMENT 24 | MARCH 2014 sal Sinuses. Rhinology. 2014 Suppl. 24: 1-34. European Position Paper on the Anatomical Terminology of the Internal Nose and Paranasal Sinuses Lund VJ, Stammberger H, Fokkens WJ et al. 2014 Anatomical terminology cover JS.indd 1 27-02-14 23:03 European Position Paper on the Anatomical Terminology of the INTERN AT Internal Nose and Paranasal Sinuses IO N A L R H I N O L O G I C Official Journal of the European and International Rhinologic Societies S O C I E Y T Editor-in-Chief Address Prof V.J. Lund Journal Rhinology, c/o AMC, Mrs. J. Kosman / A2-234, PO Box 22 660, Prof W.J. Fokkens 1100 DD Amsterdam, the Netherlands. Tel: +31-20-566 4534 Associate Editor Fax: +31-20-566 9662 Prof P.W. Hellings E-mail: [email protected] Website: www.rhinologyjournal.com Managing Editor Dr. W.T.V. Germeraad Assistant Editor Dr. Ch. Georgalas Editorial Assistant (contact for manuscripts) Mrs J. -

Tikrit University – Collage of Dentistry Dr.Ban IS Head & Neck Anatomy 2
Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. The Face/part 2: Lec [2] Sensory nerve supply of the face: The trigeminal nerve has three divisions : ophthalmic, maxillary and mandibular. The skin of the face is supplied by the branches of the three divisions of the trigeminal nerve except the skin over the parotid gland and part of the auricle of the ear [lower part medial and lateral surfaces] which supplied by the great auricular nerve. Ophthalmic nerve.. Five cutaneous branches: 1-The lacrimal nerve supplies a small area of skin over the lateral part of the upper lid. 2-The supraorbital nerve indents the bone into a notch or a foramen. The nerve passes up, breaking into several branches which radiate out and supply the forehead and scalp up to the vertex. 1 cden.tu.edu.iq Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. 3-The smaller supratrochlear nerve passes up on the medial side of the supraorbital nerve to supply the middle of the forehead up to the hairline. 4-The infratrochlear nerve supplies skin on the medial part of the upper lid and, passing above the medial palpebral ligament, descends along the side of the external nose, supplying skin over the bridge of the nose. These four branches of the ophthalmic nerve also supply upper lid conjunctiva. 5-The external nasal nerve supplies the middle of the external nose down to the tip. It emerges between the nasal bone and the upper nasal cartilage. -

Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula
brain sciences Review Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula Justin Dye 1,*, Gary Duckwiler 2, Nestor Gonzalez 3, Naoki Kaneko 2, Robert Goldberg 4, Daniel Rootman 4, Reza Jahan 2, Satoshi Tateshima 2 and Viktor Szeder 2 1 Department of Neurosurgery, Loma Linda University, Loma Linda, CA 92354, USA 2 Division of Interventional Neuroradiology, Department of Radiological Sciences, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (G.D.); [email protected] (N.K.); [email protected] (R.J.); [email protected] (S.T.); [email protected] (V.S.) 3 Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA; [email protected] 4 Department of Ophthalmology, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (R.G.); [email protected] (D.R.) * Correspondence: [email protected]; Tel.: +1-909-558-6338 Received: 16 July 2020; Accepted: 12 August 2020; Published: 14 August 2020 Abstract: Dural arteriovenous fistulas involving the cavernous sinus can lead to orbital pain, vision loss and, in the setting of associated cortical venous reflux, intracranial hemorrhage. The treatment of dural arteriovenous fistulas has primarily become the role of the endovascular surgeon. The venous anatomy surrounding the cavernous sinus and venous sinus thrombosis that is often associated with these fistulas contributes to the complexity of these interventions. The current report gives a detailed description of the alternate endovascular routes to the cavernous sinus based on a single center’s experience as well as a literature review supporting each approach.