Transvenous Embolization of a Direct Carotid Cavernous Fistula Through the Pterygoid Plexus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arteria Carotis Externa ACE External Carotid Artery
Common carotid artery CCA External Carotid artery ECA Internal carotid artery, ICA Subclavian artery SA and veins Ivo Klepáček ´tooth ache´ Salisbury cathedrale Three vascular systems are finally formed: Intraembryonic (cardinal); aortic sac (later gives rise aortic arches) Vitelline (aa. + vv.) Development of the vascular Placental system (umbilical Day 27 aa. + vv.) 1st – maxillary artery 2nd – hyoid, stapedial aa. 3rd – common carotid a. and first part of the internal carotid a., external carotid a. 4th – part of the subclavian aa. some of intersegmental arteries Common carotid artery Anterolaterally – skin, fascia, sternocleidomastoid muscle, sternohyoid, sternothyroid, superior belly of the omohyoid Posteriorly – transverse process of the C4 vertebrae, prevertebral muscles, sympathetic trunk Medially – wall of the pharynx and larynx, trachea, esophagus, the lobe of the thyroid gland Laterally – the internal jugular vein, vagus nerve (posterolaterally) Fascia pretrachealis a ACC Pretracheal fascia and ACC Sympathetic plexus surrounding arteries comes from sympathetic trunk External carotid artery ECA Anterolaterally – sternocleidomastoid muscle, XII. nerve, within parotid gland is crossed by VII. nerve, fascia, skin Medially – wall of the pharynx, internal carotid artery, stylopharyngeus, pharyngeal branch of the vagus For head without orbit, inner ear and brain Internal jugular Styloid vein lies septum dorsally and laterally from internal carotid artery behind m. m. stylohyoideus and styloglossus External carotid artery lies ventrally -

The Anatomy of Th-E Blood Vascular System of the Fox ,Squirrel
THE ANATOMY OF TH-E BLOOD VASCULAR SYSTEM OF THE FOX ,SQUIRREL. §CIURUS NlGER. .RUFIVENTEB (OEOEEROY) Thai: for the 009m of M. S. MICHIGAN STATE COLLEGE Thomas William Jenkins 1950 THulS' ifliillifllfllilllljllljIi\Ill\ljilllHliLlilHlLHl This is to certifg that the thesis entitled The Anatomy of the Blood Vascular System of the Fox Squirrel. Sciurus niger rufiventer (Geoffroy) presented by Thomas William Jenkins has been accepted towards fulfillment of the requirements for A degree in MEL Major professor Date May 23’ 19500 0-169 q/m Np” THE ANATOMY OF THE BLOOD VASCULAR SYSTEM OF THE FOX SQUIRREL, SCIURUS NIGER RUFIVENTER (GEOFFROY) By THOMAS WILLIAM JENKINS w L-Ooffi A THESIS Submitted to the School of Graduate Studies of Michigan State College of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Department of Zoology 1950 \ THESlSfi ACKNOWLEDGMENTS Grateful acknowledgment is made to the following persons of the Zoology Department: Dr. R. A. Fennell, under whose guidence this study was completed; Mr. P. A. Caraway, for his invaluable assistance in photography; Dr. D. W. Hayne and Mr. Poff, for their assistance in trapping; Dr. K. A. Stiles and Dr. R. H. Manville, for their helpful suggestions on various occasions; Mrs. Bernadette Henderson (Miss Mac), for her pleasant words of encouragement and advice; Dr. H. R. Hunt, head of the Zoology Department, for approval of the research problem; and Mr. N. J. Mizeres, for critically reading the manuscript. Special thanks is given to my wife for her assistance with the drawings and constant encouragement throughout the many months of work. -

Variant Position of the Facial Nerve in Parotid Gland
eISSN 1308-4038 International Journal of Anatomical Variations (2011) 4: 3–4 Case Report Variant position of the facial nerve in parotid gland Published online January 14th, 2011 © http://www.ijav.org Rajesh B. ASTIK ABSTRACT Urvi H. DAVE The division of the parotid gland into superficial and deep lobes by facial nerve has an important implication in parotid Krishna Swami GAJENDRA gland neoplasm. This plane is used in superficial or total parotidectomy to avoid damage to the facial nerve. During routine dissection in the Department of Anatomy, we found variably located facial nerve in the parotid gland of the left side. The main trunk of the facial nerve was located between maxillary vein and superficial temporal vein. It was divided into temporofacial and cervicofacial divisions. Both divisions crossed maxillary vein superficially instead Department of Anatomy, GSL Medical College, Rajahmundry, District- East Godavari, of retromandibular vein which was formed outside the parotid gland substance. Andhra Pradesh, INDIA. The operating surgeon should be familiar with this variation during parotidectomy to reduce the iatrogenic injury to the facial nerve. © IJAV. 2011; 4: 3–4. Dr. Rajesh B. Astik Associate Professor Department of Anatomy GSL Medical College NH-5, Rajahmundry District- East Godavari. Andhra Pradesh, 533296, INDIA. +91 883 2484999 [email protected] Received July 15th, 2010; accepted January 4th, 2011 Key words [facial nerve] [parotid gland] [retromandibular vein] [total parotidectomy] Introduction vein superficially instead of the retromandibular vein. The The retromandibular vein is formed by union of the maxillary retromandibular vein was formed by union of maxillary and and superficial temporal veins in the parotid gland [1]. -

Morphology and Fracture Effects of the Hamulus Pterygoid: a Literature Review of the Last 49 Years
Latin American Journal of Development, Curitiba, v. 3, n. 1, p. 475-487, jan./feb. 2021. ISSN 2674-9297 Morphology and fracture effects of the hamulus pterygoid: a literature review of the last 49 years Morfología y efectos de fractura del hamulus pterygoid: una revisión de la literatura de los últimos 49 años DOI: 10.46814/lajdv3n1-041 Recebimento dos originais: 30/10/2020 Aceitação para publicação: 23/12/2020 Polyanne Junqueira Silva Andresen Strini PhD, Federal University of Uberlândia - UFU, Uberlândia, MG, Brazil Address: Rio Preto Street, 178, Lídice, Uberlândia - MG Paulinne Junqueira Silva Andresen Strini PhD, Federal University of Uberlândia - UFU, Uberlândia, MG, Brazil Address: Rio Preto Street, 178, Lídice, Uberlândia - MG ABSTRACT The hamulus pterygoid consists in a relevant anatomical structure, important for fixation of several tendons and muscles, keeping the integrity of soft palate and pharynx. A literature review was conducted in order to investigate the morphology and effect of hamulus pterygoid fracture in clinical manifestation and its relationships with other orofacial components. A literature search was conducted, using Pubmed and Bireme data bases, and covering the time period 1970 to 2019. The Key words for the research were hamulus pterygoid, pterygoid fracture and hamulus pterygoid fracture, resulting in 440 articles, being 41 initials selected. Among them, just 31 were included in the analysis and 08 of the articles were not available through our library system or were in volumes before our holdings began. The remaining were excluded when they weren’t in English idiom, or when didn’t talk about morphological, functional or damages in the hamulus pterygoid. -

Vascular Supply to the Head and Neck
Vascular supply to the head and neck Sumamry This lesson covers the head and neck vascular supply. ReviseDental would like to thank @KIKISDENTALSERVICE for the wonderful drawings in this lesson. Arterial supply to the head Facial artery: Origin: External carotid Branches: submental a. superior and inferior labial a. lateral nasal a. angular a. Note: passes superiorly over the body of there mandible at the masseter Superficial temporal artery: Origin: External carotid Branches: It is a continuation of the ex carotid a. Note: terminal branch of the ex carotid a. and is in close relation to the auricular temporal nerve Transverse facial artery: Origin: Superficial temporal a. Note: exits the parotid gland Maxillary branch: supplies the areas missed from the above vasculature Origin: External carotid a. Branches: (to the face) infraorbital, buccal and inferior alveolar a.- mental a. Note: Terminal branch of the ex carotid a. The ophthalmic branches Origin: Internal carotid a. Branches: Supratrochlear, supraorbital, lacrimal, anterior ethmoid, dorsal nasal Note:ReviseDental.com enters orbit via the optic foramen Note: The face arterial supply anastomose freely. ReviseDental.com ReviseDental.com Venous drainage of the head Note: follow a similar pathway to the arteries Superficial vessels can communicate with deep structures e.g. cavernous sinus and the pterygoid plexus. (note: relevant for spread of infection) Head venous vessels don't have valves Supratrochlear vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supra-orbital v. Note: from the angular vein Supra-orbital vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supratrochlear v. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

Normal Flow Signal of the Pterygoid Plexus on 3T MRA in Patients Without DAVF of the Cavernous Sinus
ORIGINAL RESEARCH EXTRACRANIAL VASCULAR Normal Flow Signal of the Pterygoid Plexus on 3T MRA in Patients without DAVF of the Cavernous Sinus K. Watanabe, S. Kakeda, R. Watanabe, N. Ohnari, and Y. Korogi ABSTRACT BACKGROUND AND PURPOSE: Cavernous sinuses and draining dural sinuses or veins are often visualized on 3D TOF MRA images in patients with dural arteriovenous fistulas involving the CS. Flow signals may be seen in the jugular vein and dural sinuses at the skull base on MRA images in healthy participants, however, because of reverse flow. Our purpose was to investigate the prevalence of flow signals in the pterygoid plexus and CS on 3T MRA images in a cohort of participants without DAVFs. MATERIALS AND METHODS: Two radiologists evaluated the flow signals of the PP and CS on 3T MRA images obtained from 406 consecutive participants by using a 5-point scale. In addition, the findings on 3T MRA images were compared with those on digital subtraction angiography images in an additional 171 participants who underwent both examinations. RESULTS: The radiologists identified 110 participants (27.1%; 108 left, 10 right, 8 bilateral) with evidence of flow signals in the PP alone (n ϭ 67) or in both the PP and CS (n ϭ 43). Flow signals were significantly more common in the left PP than in the right PP. In 171 patients who underwent both MRA and DSA, the MRA images showed flow signals in the PP with or without CS in 60 patients; no DAVFs were identified on DSA in any of these patients. CONCLUSIONS: Flow signals are frequently seen in the left PP on 3T MRA images in healthy participants. -

Yagenich L.V., Kirillova I.I., Siritsa Ye.A. Latin and Main Principals Of
Yagenich L.V., Kirillova I.I., Siritsa Ye.A. Latin and main principals of anatomical, pharmaceutical and clinical terminology (Student's book) Simferopol, 2017 Contents No. Topics Page 1. UNIT I. Latin language history. Phonetics. Alphabet. Vowels and consonants classification. Diphthongs. Digraphs. Letter combinations. 4-13 Syllable shortness and longitude. Stress rules. 2. UNIT II. Grammatical noun categories, declension characteristics, noun 14-25 dictionary forms, determination of the noun stems, nominative and genitive cases and their significance in terms formation. I-st noun declension. 3. UNIT III. Adjectives and its grammatical categories. Classes of adjectives. Adjective entries in dictionaries. Adjectives of the I-st group. Gender 26-36 endings, stem-determining. 4. UNIT IV. Adjectives of the 2-nd group. Morphological characteristics of two- and multi-word anatomical terms. Syntax of two- and multi-word 37-49 anatomical terms. Nouns of the 2nd declension 5. UNIT V. General characteristic of the nouns of the 3rd declension. Parisyllabic and imparisyllabic nouns. Types of stems of the nouns of the 50-58 3rd declension and their peculiarities. 3rd declension nouns in combination with agreed and non-agreed attributes 6. UNIT VI. Peculiarities of 3rd declension nouns of masculine, feminine and neuter genders. Muscle names referring to their functions. Exceptions to the 59-71 gender rule of 3rd declension nouns for all three genders 7. UNIT VII. 1st, 2nd and 3rd declension nouns in combination with II class adjectives. Present Participle and its declension. Anatomical terms 72-81 consisting of nouns and participles 8. UNIT VIII. Nouns of the 4th and 5th declensions and their combination with 82-89 adjectives 9. -

The Development of Mammalian Dural Venous Sinuses with Especial Reference to the Post-Glenoid Vein
J. Anat. (1967), 102, 1, pp. 33-56 33 With 12 figures Printed in Great Britian The development of mammalian dural venous sinuses with especial reference to the post-glenoid vein H. BUTLER Department ofAnatomy, University of Saskatchewan, Saskatoon, Canada The intracranial venous outflow of mammals drains into both the internal and external jugular veins and the relative role of these two veins varies between different adult mammals as well as at different phases of embryonic and foetal life. In general, the primary head vein (consisting of venae capitis medialis and lateralis and their tributaries) gives rise to the dural venous sinuses which drain into the anterior cardinal vein (the future internal jugular vein). The external jugular veins appear as the face and jaws develop but, at all times, the two venous systems freely com- municate with each other. Morphologically, as shown by Sutton (1888), both the dural venous sinuses and the external jugular venous system are extracranial in so far as they are situated outside the dura mater. The chondrocranium and the dermocranium, however, develop in between the dural venous sinuses and the external jugular vein system (Butler, 1957). Thus, in the adult mammal, the bony skull wall separates the two venous systems, and therefore the dural venous sinuses are topographically intracranial whereas the external jugular venous system is extracranial. Furthermore the development of the skull localizes the connexions between the dural venous sinuses and the external jugular venous system to the various fontanelles and neuro-vascular foramina to form the emissary veins. The post-glenoid vein is one of the more important and controversial emissary veins since its presence or absence has been used in attempts to establish mammalian phylogenetic relationships (van Gelderen, 1925; Boyd, 1930). -

Spatial Aspect of the Mouse Orbital Venous Sinus Materials
Okajimas Folia Anat. Jpn., 56(6) : 329-336, March 1980 Spatial Aspect of the Mouse Orbital Venous Sinus By TOSHIO YAMASHITA, AKIRA TAKAHASHI and RYOHEI HONJIN Department of Anatomy, School of Medicine, Kanazawa University, Kanazawa 920, Japan (Director : Prof. Dr. Ryohei Honjin) -Received for Publication, July 24, 1979- Key Words: Mouse orbit, Orbital venous sinus, Orbital vein, Orbital muscle Summary. The spatial aspect of the mouse orbital venous sinus and its topogra- phical relation to the venous system of the head were studied in serial sections by light microscopy. The orbital venous sinus was found to extend between the orbital wall and the muscle cone and had a huge invaginated sac, which began from the antero-medial part of the sinus and enveloped most of Harder's gland. The orbital venous sinus received almost all the venous drainage from the eyeball, muscle cone, Harder's gland and conjunctiva, and communicated with the cavernous sinus, ptery- goid plexus, superficial temporal vein and facial vein. The mouse orbital venous sinus may correspond to the human superior and in- ferior ophthalmic veins. As well as draining blood from the orbital contents, it may play a significant role in producing exophthalmos when on the alert, in absorb- ing shock from the exterior to the orbital contents, and in promoting secretion from Harder's gland. Introduction Materials and Methods A large venous sinus occupying much The heads of 3 adult mice, pure strain of the retrobulbar space was reported KH-1 (Mus wagneri var. albula), were under the name of the "orbital venous removed, immersed in a mixture of 75 ml sinus" in the dog by Ulbrich (1909) and 70% ethanol, 20 ml 35% formalin and 5 in the rabbit by Davis (1929). -

Morphological Characteristics of Foramen of Vesalius and Its Relationship with Clinical Implications
Original article Morphological characteristics of foramen of Vesalius and its relationship with clinical implications Rossi, AC.1*, Freire, AR.1, Prado, FB.1, Caria, PHF.1 and Botacin, PR.2 1Department of Morphology, State University of Campinas – UNICAMP, Piracicaba, SP, Brazil 2Departament of Basic Sciences, Paulista State University – UNESP, Araçatuba, SP, Brazil *E-mail: [email protected] Abstract The aim of this study was to evaluate the incidence as well morphometry of the foramen of Vesalius in human skulls and analyzing their clinical importance. Dry human skulls (n = 80) and with gender distinction were used (40 male and 40 female). The results demonstrates an total incidence of 40%, 13.75% skulls with the bilateral presence of the foramen, 26.25% skulls with the unilateral presence of the foramen, 31.25% skulls with foramen only of the right side, 22.50% skulls with foramen only of the left side, 25% masculine skulls with at least 1 foramen and 52.25% skulls with at least 1 foramen. The morphometry showed an average diameter of 1.457 ± 1.043 mm on the right and 1592 ± 0938 mm to the left. The average distance to the foramen ovale was 1.853 ± 0.303 mm on the right side and 2.464 ± 0.311 mm on the left. It can be concluded that a deepened anatomical study of the foramen of Vesalius collaborates not only for anatomical knowledge of this structure, but also in clinical situations involving this foramen. Keywords: foramen of Vesalius, emissary vein, thrombophlebitis, neurosurgery. 1 Introduction The base of the skull has a lot of foramens, establishing rhizotomy (GUSMÃO, MAGALDI and ARANTES, 2003); communications between the extracranial and intracranial (SHINOHARA, MELO, SILVEIRA ET AL., 2010). -
27. Veins of the Head and Neck
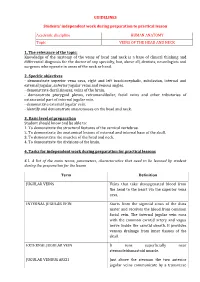
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath.