Peripheral Nervous System Peripheral Nervous System Comprises: A) Cranial Nerves: 12 in Number, Arise Mainly from Brain Stem
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
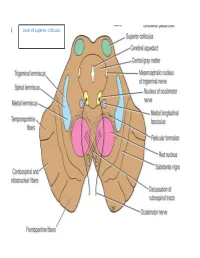
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Palatal Injection Does Not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth
Open Access Review Article DOI: 10.7759/cureus.2120 Palatal Injection does not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth Joe Iwanaga 1 , R. Shane Tubbs 2 1. Seattle Science Foundation 2. Neurosurgery, Seattle Science Foundation Corresponding author: Joe Iwanaga, [email protected] Abstract The superior alveolar nerves course lateral to the maxillary sinus and the greater palatine nerve travels through the hard palate. This difficult three-dimensional anatomy has led some dentists and oral surgeons to a critical misunderstanding in developing the anterior and middle superior alveolar (AMSA) nerve block and the palatal approach anterior superior alveolar (P-ASA) nerve block. In this review, the anatomy of the posterior, middle and anterior superior alveolar nerves, greater palatine nerve, and nasopalatine nerve are revisited in order to clarify the anatomy of these blocks so that the perpetuated anatomical misunderstanding is rectified. We conclude that the AMSA and P-ASA nerve blockades, as currently described, are not based on accurate anatomy. Categories: Anesthesiology, Medical Education, Other Keywords: anatomy, innervation, local anesthesia, maxillary nerve, nerve block, tooth Introduction And Background Anesthetic blockade of the posterior superior alveolar (PSA) branch of the maxillary nerve has played an important role in the endodontic treatment of irreversible acute pulpitis of the upper molar teeth except for the mesiobuccal root of the first molar tooth [1, 2]. This procedure requires precise anatomical knowledge of the pterygopalatine fossa and related structures in order to avoid unnecessary complications and to make the blockade most effective. The infraorbital nerve gives rise to middle superior alveolar (MSA) and anterior superior alveolar (ASA) branches. -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

The Incisive Canal: a Comprehensive Review. Cureus 10(7): E3069
Providence St. Joseph Health Providence St. Joseph Health Digital Commons Journal Articles and Abstracts 7-30-2018 The ncI isive Canal: A Comprehensive Review. Sasha Lake Joe Iwanaga Shogo Kikuta Rod J Oskouian Neurosurgery, Swedish Neuroscience Institute, Seattle, USA. Marios Loukas See next page for additional authors Follow this and additional works at: https://digitalcommons.psjhealth.org/publications Part of the Neurology Commons, and the Pathology Commons Recommended Citation Lake, Sasha; Iwanaga, Joe; Kikuta, Shogo; Oskouian, Rod J; Loukas, Marios; and Tubbs, R Shane, "The ncI isive Canal: A Comprehensive Review." (2018). Journal Articles and Abstracts. 813. https://digitalcommons.psjhealth.org/publications/813 This Article is brought to you for free and open access by Providence St. Joseph Health Digital Commons. It has been accepted for inclusion in Journal Articles and Abstracts by an authorized administrator of Providence St. Joseph Health Digital Commons. For more information, please contact [email protected]. Authors Sasha Lake, Joe Iwanaga, Shogo Kikuta, Rod J Oskouian, Marios Loukas, and R Shane Tubbs This article is available at Providence St. Joseph Health Digital Commons: https://digitalcommons.psjhealth.org/publications/813 Open Access Review Article DOI: 10.7759/cureus.3069 The Incisive Canal: A Comprehensive Review Sasha Lake 1 , Joe Iwanaga 2 , Shogo Kikuta 3 , Rod J. Oskouian 4 , Marios Loukas 5 , R. Shane Tubbs 6 1. Anatomical Studies, St. George's, St. George, GRD 2. Medical Education and Simulation, Seattle Science Foundation, Seattle, WA, USA 3. Seattle Science Foundation, Seattle, USA 4. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 5. Anatomical Sciences, St. George's University, St. -

Anatomy of Maxillary and Mandibular Local Anesthesia
Anatomy of Mandibular and Maxillary Local Anesthesia Patricia L. Blanton, Ph.D., D.D.S. Professor Emeritus, Department of Anatomy, Baylor College of Dentistry – TAMUS and Private Practice in Periodontics Dallas, Texas Anatomy of Mandibular and Maxillary Local Anesthesia I. Introduction A. The anatomical basis of local anesthesia 1. Infiltration anesthesia 2. Block or trunk anesthesia II. Review of the Trigeminal Nerve (Cranial n. V) – the major sensory nerve of the head A. Ophthalmic Division 1. Course a. Superior orbital fissure – root of orbit – supraorbital foramen 2. Branches – sensory B. Maxillary Division 1. Course a. Foramen rotundum – pterygopalatine fossa – inferior orbital fissure – floor of orbit – infraorbital 2. Branches - sensory a. Zygomatic nerve b. Pterygopalatine nerves [nasal (nasopalatine), orbital, palatal (greater and lesser palatine), pharyngeal] c. Posterior superior alveolar nerves d. Infraorbital nerve (middle superior alveolar nerve, anterior superior nerve) C. Mandibular Division 1. Course a. Foramen ovale – infratemporal fossa – mandibular foramen, Canal -> mental foramen 2. Branches a. Sensory (1) Long buccal nerve (2) Lingual nerve (3) Inferior alveolar nerve -> mental nerve (4) Auriculotemporal nerve b. Motor (1) Pterygoid nerves (2) Temporal nerves (3) Masseteric nerves (4) Nerve to tensor tympani (5) Nerve to tensor veli palatine (6) Nerve to mylohyoid (7) Nerve to anterior belly of digastric c. Both motor and sensory (1) Mylohyoid nerve III. Usual Routes of innervation A. Maxilla 1. Teeth a. Molars – Posterior superior alveolar nerve b. Premolars – Middle superior alveolar nerve c. Incisors and cuspids – Anterior superior alveolar nerve 2. Gingiva a. Facial/buccal – Superior alveolar nerves b. Palatal – Anterior – Nasopalatine nerve; Posterior – Greater palatine nerves B. -

Entrapment Neuropathy of the Central Nervous System. Part II. Cranial
Entrapment neuropathy of the Cranial nerves central nervous system. Part II. Cranial nerves 1-IV, VI-VIII, XII HAROLD I. MAGOUN, D.O., F.A.A.O. Denver, Colorado This article, the second in a series, significance because of possible embarrassment considers specific examples of by adjacent structures in that area. The same entrapment neuropathy. It discusses entrapment can occur en route to their desti- nation. sources of malfunction of the olfactory nerves ranging from the The first cranial nerve relatively rare anosmia to the common The olfactory nerves (I) arise from the nasal chronic nasal drip. The frequency of mucosa and send about twenty central proces- ocular defects in the population today ses through the cribriform plate of the ethmoid bone to the inferior surface of the olfactory attests to the vulnerability of the optic bulb. They are concerned only with the sense nerves. Certain areas traversed by of smell. Many normal people have difficulty in each oculomotor nerve are pointed out identifying definite odors although they can as potential trouble spots. It is seen perceive them. This is not of real concern. The how the trochlear nerves are subject total loss of smell, or anosmia, is the significant to tension, pressure, or stress from abnormality. It may be due to a considerable variety of causes from arteriosclerosis to tu- trauma to various bony components morous growths but there is another cause of the skull. Finally, structural which is not usually considered. influences on the abducens, facial, The cribriform plate fits within the ethmoid acoustic, and hypoglossal nerves notch between the orbital plates of the frontal are explored. -

Communication Between the Mylohyoid and Lingual Nerves: Clinical Implications
Int. J. Morphol., Case Report 25(3):561-564, 2007. Communication Between the Mylohyoid and Lingual Nerves: Clinical Implications Comunicación entre los Nervios Milohioideo y Lingual: Implicancias Clínicas *Valéria Paula Sassoli Fazan; **Omar Andrade Rodrigues Filho & ***Fernando Matamala FAZAN, V. P. S.; RODRIGUES FILHO, O. A. & MATAMALA, F. Communication between the mylohyoid and lingual nerves: Clinical implications. Int. J. Morphol., 25(3):561-564, 2007. SUMMARY: The mylohyoid muscle plays an important role in chewing, swallowing, respiration and phonation, being the mylohyoid nerve also closely related to these important functions. It has been postulated that the mylohyoid nerve might have a role in the sensory innervation of the chin and the lower incisor teeth while the role of the mylohyoid nerve in the mandibular posterior tooth sensation is still a controversial issue. Although variations in the course of the mylohyoid nerve in relation to the mandible are frequently found on the dissecting room, they have not been satisfactorily described in the anatomical or surgical literature. It is well known that variations on the branching pattern of the mandibular nerve frequently account for the failure to obtain adequate local anesthesia in routine oral and dental procedures and also for the unexpected injury to branches of the nerves during surgery. Also, anatomical variations might be responsible for unexpected and unexplained symptoms after a certain surgical procedure. We describe the presence of a communicating branch between the mylohyoid and lingual nerves in an adult male cadaver, and discuss its clinical/surgical implications as well as its possible role on the sensory innervation of the tongue. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Innervation of the Temporomandibular Joint Can Be Discussed It Is Necessary First to Describe Its Embryology, Gfoss Anatomy and Microscopic Appe¿Ìrance
à8.ì 'R? INNERVATION OF THE TEMPOROMAI\DIBULAR J AN EXPERIMENTAL AMMAL MODEL USING AUSTRALIAN MERINO STIEEP ABDOLGHAFAR TAHMASEBI-SARVESTANI' B. Sc, M. Sc Thesis submitted for the degree of DOCTOR OF PHILOSOPHY In The Department of Anatomical Sciences The University of Adelaide (Faculty of Medicine)' Adelaide, South Australia, 5005 April, L997 tfüs tñesisis [elicatelø nl wtfe Aggñleñ ø¡tlour g4.arzi"e tfr.re e c friûfren Ía fiera ñ, fo zic ñ atú fi l-1 ACKNOWLEDGMENTS I am greatly indebted to my supervisors Dr. Ray Tedman and Professor Alastair Goss who first inrroduced me to this freld of study and providing me with the opportunity to carry out this work. I wish to thank them for their constant interest and guidance throughout the course of this study. I am also indebted to the scholarship committee of the Shiraz Medical Science University and Ministry of Health and Medical Education, Iran for gânting me a 4 year scholarship to study at the Universiry of Adelaide. I thank professor Goss and the Japanese Surgical Research team for their expertise in surgical animal models, and Professor July Polak and Dr Mika Hukkanen, Royal postgraduate Medical School London University for their expertise in immunohistochemistry and for providing some of the antisera used in the neuropeptide studies. I would also like to thank Professor Ian Gibbins, Department of Anatomy and Histology of the Flinders Medical Centre for, without the use of his laboratories, materials, and expertise, the double and triple labelling parts of the immunocytochemical work would not have occurred. I also orwe many thanks to Susan Matthew, a senior laboratory officer for her skilful technical assistance in double and triple immunocytochemistry. -

Extracranial Course of Cranial Nerves
Extracranial course of cranial nerves Oculomotor, Trochlear, Abducent, Trigeminal, Facial and Accessory nerves Dr. Heba Kalbouneh Associate Professor of Anatomy and Histology Dr. Heba Kalbouneh Brainstem Mid brain Pons Medulla Pons Inferior view Facial nerve Anatomically, the course of the facial nerve can be divided into two parts: Motor: Innervates the muscles of facial Intracranial – the course of the nerve through expression, the posterior belly of the the cranial cavity, and the cranium itself. digastric, the stylohyoid and the stapedius Extracranial – the course of the nerve outside muscles. the cranium, through the face and neck. General Sensory: A small area around the concha of the auricle, EAM Special Sensory: Provides special taste sensation to the anterior 2/3 of the tongue. Parasympathetic: Supplies many of the glands of the head and neck, including: 1- Submandibular and sublingual salivary glands (via the submandibular ganglion/ chorda tympani) 2- Nasal, palatine and pharyngeal mucous glands (via the pterygopalatine ganglion/ greater petrosal) 3- Lacrimal glands (via the pterygopalatine ganglion/ greater petrosal) Dr. Heba Kalbouneh Intracranial course The nerve arises in the pons. It begins as two roots; a large motor root, and a small sensory root The two roots travel through the internal acoustic meatus. Pons Here, they are in very close proximity to the inner ear. 7th (motor) 8th Note: The part of the facial nerve that runs between the motor root of facial and vestibulocochlear nerve is sometimes Kalbouneh known as the nervus intermedius It contains the sensory and parasympathetic Heba fibers of the facial nerve Dr. Dr. Still within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal. -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

Is Sometimes Mushroom-Shaped, Due to a Neuroma-Like En- with the Nerve Loop, Or the Blood-Vesselaccompanying
INTRASCLERAL NERVE LOOPS ALGERNON B. REESE, M.D. New York The long ciliary nerves accompany the long posterior ciliary arteries through their emissaries in the posterior part of the sclera, each nerve dividing into two branches before emerging into the suprachoroidal space. These four nerves course forward in a meridional direction between the sclera and the choroid. In some instances the ciliary nerve enters the sclera near the junction of the orbiculus ciliaris and the corona ciliaris, or 2.5 to 3 mm. from the angle of the an- terior chamber, then turns abruptly back again, to resume its forward course into the ciliary body. Occasionally the nerve loop thus formed extends through the entire thickness of the sclera, with its cupola projecting above the external surface, covered only by conjunctiva. This nerve loop may enter into the sclera perpendicular to or at an angle with the surface, or it may be retroverted or be anteflexed. Its apex is sometimes mushroom-shaped, due to a neuroma-like en- largement. At times chromatophores from the supracho- roidea appear, extending up into the interspace of the loop, and occasionally similar pigment cells, as well as smooth muscle from the ciliary body, are seen along the wall of the scleral foramen through which the loop passes. On rare oc- casions a cyst is seen accompanying a loop. The anterior ciliary artery, in its inward course, may share the emissary with the nerve loop, or the blood-vessel accompanying the loop may be an anastomotic branch between the episcleral and the ciliary vessels. Either the cupola or the stem of the loop may send off nerve branches which extend forward into the cornea.