Is Sometimes Mushroom-Shaped, Due to a Neuroma-Like En- with the Nerve Loop, Or the Blood-Vesselaccompanying
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Morphometric Study of the Ciliary Ganglion and Its Pertinent Intraorbital Procedure L
Folia Morphol. Vol. 79, No. 3, pp. 438–444 DOI: 10.5603/FM.a2019.0112 O R I G I N A L A R T I C L E Copyright © 2020 Via Medica ISSN 0015–5659 journals.viamedica.pl Morphometric study of the ciliary ganglion and its pertinent intraorbital procedure L. Tesapirat1, S. Jariyakosol2, 3, V. Chentanez1 1Department of Anatomy, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand 2Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand 3Ophthalmology Department, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, Thailand [Received: 20 September 2019; Accepted: 12 October 2019] Background: Ciliary ganglion (CG) can be easily injured without notice in many intraorbital procedures. Surgical procedures approaching the lateral side of the orbit are at risk of CG injury which results in transient mydriasis and tonic pupil. This study aims to focus on the morphometric study of the CG which is pertinent to intraoperative procedure. Materials and methods: Forty embalmed cadaveric globes were dissected to ob- serve the location, shape and size of CG, characteristics and number of roots reaching CG, number of short ciliary nerve in the orbit. Distances from CG to posterior end of globe, optic nerve, lateral rectus muscle and its scleral insertion were measured. Results: Ciliary ganglion was located between optic nerve and lateral rectus in every case. Its shape could be oval, round and irregular. Mean width of CG was 2.24 mm and mean length was 3.50 mm. Concerning the roots, all 3 roots were present in 29 (72.5%) cases. Absence of motor root was found in 7 (17.5%) cases. -

Trigeminal Nerve Trigeminal Neuralgia
Trigeminal nerve trigeminal neuralgia Dr. Gábor GERBER EM II Trigeminal nerve Largest cranial nerve Sensory innervation: face, oral and nasal cavity, paranasal sinuses, orbit, dura mater, TMJ Motor innervation: muscles of first pharyngeal arch Nuclei of the trigeminal nerve diencephalon mesencephalic nucleus proprioceptive mesencephalon principal (pontine) sensory nucleus epicritic motor nucleus of V. nerve pons special visceromotor or branchialmotor medulla oblongata nucleus of spinal trigeminal tract protopathic Segments of trigeminal nereve brainstem, cisternal (pontocerebellar), Meckel´s cave, (Gasserian or semilunar ganglion) cavernous sinus, skull base peripheral branches Somatotopic organisation Sölder lines Trigeminal ganglion Mesencephalic nucleus: pseudounipolar neurons Kovách Motor root (Radix motoria) Sensory root (Radix sensoria) Ophthalmic nerve (V/1) General sensory innervation: skin of the scalp and frontal region, part of nasal cavity, and paranasal sinuses, eye, dura mater (anterior and tentorial region) lacrimal gland Branches of ophthalmic nerve (V/1) tentorial branch • frontal nerve (superior orbital fissure outside the tendinous ring) o supraorbital nerve (supraorbital notch) o supratrochlear nerve (supratrochlear notch) o lacrimal nerve (superior orbital fissure outside the tendinous ring) o Communicating branch to zygomatic nerve • nasociliary nerve (superior orbital fissure though the tendinous ring) o anterior ethmoidal nerve (anterior ethmoidal foramen then the cribriform plate) (ant. meningeal, ant. nasal, -
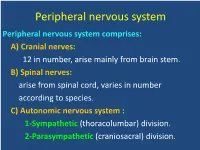
Peripheral Nervous System Peripheral Nervous System Comprises: A) Cranial Nerves: 12 in Number, Arise Mainly from Brain Stem
Peripheral nervous system Peripheral nervous system comprises: A) Cranial nerves: 12 in number, arise mainly from brain stem. B) Spinal nerves: arise from spinal cord, varies in number according to species. C) Autonomic nervous system : 1-Sympathetic (thoracolumbar) division. 2-Parasympathetic (craniosacral) division. Cranial nerves They are 12 pairs General features: – They are known by roman numbers from (rostral to caudal) . – Some nerves take their names according to: * Function as olfactory and abducent * Distribution as facial and hypoglossal * Shape as trigeminal. - All cranial nerves have superficial origins on ventral aspect of brain except trochlear nerve originates from dorsal aspect of brain. -All cranial nerves except first one originate from brain stem. - Each nerve emerges from cranial cavity through a foramen. - All cranial nerves except vagus distributed generally in head region. - 3,7,9,10 cranial nerves carry parasympathetic fibers. - Classification of cranial nerves: - They are classified according to the function into: 1-Sensory nerves: 1,2,8. 2-Motor nerves: 3,4,6,11,12. 3-Mixed nerves: 5,7,9,10. I- Olfactory nerves Type: • Sensory for smell. • Represented by bundles of nerve fibers, not form trunk. Origin: • Central processes of olfactory cells of olfactory region of nasal cavity. Course: • They pass though cribriform plate to join olfactory bulb. Vomeronasal nerve: • It arises from vomeronasal organ ,passes through medial border of cribriform plate to terminate in olfactory bulb. II- Optic nerve Type: • Sensory for vision. Origin: • Central processes of ganglion cells of retina. Course: • Fibers converge toward optic papilla forming optic nerve, emerges from eyeball. • Then passes through optic foramen and decussates with its fellow to form optic chiasma. -

1 Conjunctiva
Dr Parul Ichhpujani Assistant Professor Deptt. Of Ophthalmology, Government Medical College and Hospital, Sector 32, Chandigarh Subdivision of Lectures APPLIED ANATOMY INFLAMMATIONS OF Parts CONJUNCTIVA Structure Infective conjunctivitis Glands – Bacterial SYMPTOMATIC CONDITIONS – Chlamydial Hyperaemia –Viral Chemosis Allergic conjunctivitis Ecchymosis Xerosis Granulomatous conjunctivitis Discoloration DEGENERATIVE CONDITIONS CYSTS AND TUMOURS Pinguecula Pterygium Concretions Conjoin: to join….. has been given to this mucous membrane owing to the fact that it joins the eyeball to the lids. Palpebral conjunctiva Marginal conjunctiva extends from the lid margin to about 2 mm on the back of lid up to a shallow groove, the sulcus subtarsalis. Tarsal conjunctiva is firmly adherent to the whole tarsal plate in the upper lid. In the lower lid, it is adherent only to half width of the tarsus. Orbital part of palpebral conjunctiva lies loose between the tarsal plate and fornix. Bulbar conjunctiva Lies loose over the underlying structures and thus can be moved easily. It is separated from the anterior sclera by episcleral tissue and Tenon's capsule. A 3‐mm ridge of bulbar conjunctiva around the cornea is called limbal conjunctiva. In the area of limbus, the conjunctiva, Tenon's capsule and the episcleral tissue are fused into a dense tissue which is strongly adherent to the underlying corneoscleral junction. At the limbus, the epithelium of conjunctiva becomes continuous with that of cornea Forniceal Conjunctiva: Joins the -

The Anatomy of the Choroid – a Review
Revista Română de Anatomie funcţională şi clinică, macro- şi microscopică şi de Antropologie Vol. XV – Nr. 4 – 2016 UPDATES THE ANATOMY OF THE CHOROID – A REVIEW Şt. Oprea1*, C.M. Pantu1, F.M. Filipoiu1, Raluca Tulin1, Gabriela Diana Oprea2 1. University of Medicine and Pharmacy “Carol Davila” Bucharest Discipline of Anatomy 2. Universitary Emergency Central Military „Carol Davila“ Hospital, Bucharest THE ANATOMY OF THE CHOROID – A REVIEW (Abstract): The choroid is an important structure of the eye which can be involved in a lot of pathologies. Its great importance is given by functions like vascularization, thermoregulation and production of growth factors. A good knowl- edge of this element of the eye will help the ophthalmology specialists, especially the young ones, to understand better the pathological substrate of the diseases involving the choroid like diabetic retinopathy, age related macular degeneration wet form, choroid detachment etc. The choroid covers to the interior the fibrous tunic of the eye. It represents the posterior portion of the uvea, the anterior being represented by a thicker region, ciliary zone. Histological, choroid shows the 5 layers, from sclera to the retina: outer pigment layer, suprachoroid; two Vascular layers, one external (called Haller) and one internal, Sattler; choriocapillar layer and Bruch’s membrane. The choroid blood supply is ensured by posterior ciliary arteries (PCA), branches of the ophthalmic artery. Venous drainage is achieved through vorticity veins. Choroid’s Innervation is double, sym- pathetic and parasympathetic through dense perivascular plexus. Key words: THE CHOROID, DIABETIC RETINOPATHY, POSTERIOR CILIARY ARTERIES INTRODUCTION optical ditches appear in the cranial neural The choroid represents the main structure folds. -

And Domestic Duck (Anas Platyrhynchos F. Domestica)
Bull Vet Inst Pulawy 56, 649-653, 2012 DOI: 10.2478/v10213-012-0114-1 MORPHOMETRIC ANALYSIS OF THE CILIARY GANGLION IN THE DOMESTIC TURKEY (MELEAGRIS GALLOPAVO F. DOMESTICA) AND DOMESTIC DUCK (ANAS PLATYRHYNCHOS F. DOMESTICA) MAŁGORZATA RADZIMIRSKA Department of Nature Conservation, Institute of Biology, Jan Kochanowski University, 25-406 Kielce, Poland [email protected] Received: March 29, 2012 Accepted: December 3, 2012 Abstract The research was performed on 16 one-year-old domestic turkeys of Beltsville race and 16 domestic ducks of the Pekinese race, of both sexes. Standard histological technique was used and morphometric analysis was performed using histological samples. Ciliary ganglion morphometric analysis revealed the presence of two cell populations of ganglionic neurocytes: choroid and ciliary cells, clearly differing in diameter. Ciliary cells were predominant in turkeys, whereas choroid cells in ducks. The statistical analysis showed that the diameter and surface area of ganglionic neurocytes, the diameter and cross sectional area through the ciliary ganglion, as well as, the number of ganglionic cells on the cross-section through the ganglion were significantly larger (P<0.001) in turkeys than in ducks. The difference in the number of choroid and ciliary cells in domestic turkey and domestic duck is probably connected with eye accommodation, which seems to be greater in turkeys. Key words: domestic turkey, domestic duck, ciliary ganglion, morphometric analysis. Cephalic parasympathetic ganglia in birds, as of vision and the structures, which innervate this organ one of the main elements of the autonomic nervous in the animals. They can be used by clinicists and other system, constitute the subject of research for many biological disciplines representatives in the future. -

Anaesthesia for Ophthalmic Surgery
Update in Anaesthesia 23 ANAESTHESIA FOR OPHTHALMIC roof than the floor and nearer the lateral than the SURGERY - Part 1 : Regional Techniques medial wall. The sclera is the fibrous layer of the eyeball completely surrounding the globe except Dr. Andrei M. Varvinski, Anaesthetic Department, the cornea. It is relatively tough but can be pierced City Hospital, N 1 Arkhangelsk, Russia; Dr. Roger easily by needles. The optic nerve penetrates the Eltringham, Consultant Anaesthetist, Gloucestershire sclera posteriorly 1 or 2 mm medial to, and above, Royal Hospital. the posterior pole. The central retinal artery and vein accompany the optic nerve. The cone refers to Ophthalmic surgery can be performed under either the cone shaped structure formed by the extraocular regional or general anaesthesia. This article describes muscles of the eye. regional anaesthesia. In the next issue general Optic foramen anaesthesia will be discussed. Lateral wall of orbit Anatomy: Some basic knowledge of the anatomy of Medial wall the orbit and its contents is necessary for the succesful of orbit performance of regional anaesthesia for ophthalmic 90o surgery. If possible carefully examine the orbit in a 45o 45o skull whilst reading this article. This will make understanding the techniques described easier. Each orbit is in the shape of an irregular pyramid with its base at the front of the skull and its axis pointing posteromedially towards the apex. At the apex is the optic foramen, transmitting the optic Fig. 1. nerve and accompanying vessels and the superior and inferior orbital fissures transmitting the other Pupil nerves and the vessels. The depth of the orbit measured from the rear surface of the eyeball to the apex is about 25 mm (range 12- Iris 35 mm). -

Microtubule Polarity in the Peripheral Processes of Trigeminal Ganglion Cells: Relevance for the Retrograde Transport of Herpes Simplex Virus
The Journal of Neuroscience, January 1994, 14(l): 318325 Microtubule Polarity in the Peripheral Processes of Trigeminal Ganglion Cells: Relevance for the Retrograde Transport of Herpes Simplex Virus Kimberly S. Topp, Lauren B. Meade, and Jennifer H. LaVail Neuroscience Program and Department of Anatomy, University of California San Francisco, San Francisco, California 94143 The directional movement of many cellular organelles in neu- After disruption of the cornea1 epithelium, HSV can invade rons is dependent on polarized microtubules and direction- neuronal processesin the epithelium and stroma. The glyco- specific motor molecules. Microtubules are also thought to protein-rich envelope of the virion is thought to fuse with the mediate the retrograde transport of herpes simplex virus host cell membrane prior to entry of the virus into the cell (see (HSV) in sensory neurons. To define the cellular machinery Roizman and Sears, 1991, for review). The viral capsid and responsible for retrograde axonal transport of HSV, we have some of the associatedtegument proteins are then transported investigated the polarity of microtubules in the peripheral in a retrograde direction by trigeminal nerve axons to their cell axons of trigeminal ganglion neurons. The long ciliary nerves bodies in the ophthalmic division of the trigeminal ganglion. of rabbits were prepared for a standard “hook assay” of Here the HSV may enter a latent state or replicate and be pack- microtubule polarity. Axons in cross-sectioned nerves con- aged in a membrane-bound vesicle destined for transport in an tained microtubules with almost uniform orientation. The fast- anterogradedirection to both the CNS and the peripheral tissues growing, plus ends of these axonal microtubules are located (LaVail et al., 199 1). -

THE PUPILLARY REFLEXES and THEIR NEUROLOGICAL IMPORTANCE
( THE PUPILLARY REFLEXES and THEIR NEUROLOGICAL IMPORTANCE Suzanne R. Maystead /171 0 The pupil is a circular opening in the center of the iris, its shape and size controlled by the iris. Usually three to four milimeters in diameter in normal room light, it may reach eight to nine milimeters when maxirnimly dilated. The function of the pupil js mostly optical. It regulates the amount of light reaching the retina. It increases the depth of focus and decreases the chromatic and spherical aberration caused by the lens and cornea. The pupil is in constant motion which varies with the amount of light present. In bright light, these oscillations are small and regular, in dim light, they are larger and slower. ·rermed pupillary unrest, the bilatera l oscillations are caused by a dynamic equilibrum betwe~n the lr sympathetic and parasynpathetic systems and are considered non-patho loGical. Hippus is an extensive degree of bilateral unrest and its importance is not known. The pupillary size is controlled by both the sympathetic and parasympathetic systems. The iris muscl~s play a very important part, and any pathology or atrophy of the iris will affect the pupillary size and shape. For example, an iritis may cause unequal contractions in the sphincter. The iris, and hence the pupil, is controlled by two muscle masses, the dilator and the sphincter. The sphincter, located in the stromal layers, is composed of fully developed smooth muscle cells. It ]s about one milimeter wide and forms a ring around the pupillary border. Derived from ectoderm, it is inervated by the parasympathetic ( Oculomotor nerve via the Short Ciliary Nerve. -

The Autonomic Nervous System of the Chimaeroid Fish Hydrolagus Colliei by J
379 The Autonomic Nervous System of the Chimaeroid Fish Hydrolagus colliei By J. A. COLIN NICOL (From the Department of Zoology, University of British Columbia, Vancouver; present address, Marine Biological Laboratory, Plymouth) With two Plates SUMMARY The autonomic nervous system of the chimaeroid fish Hydrolagus colliei has been investigated by dissections and histological methods. It consists of a cranial para- sympathetic portion and a sympathetic portion confined to the trunk. The latter extends from the level of the heart to the anus and consists of segmentally arranged ganglia on each side of the dorsal aorta. These ganglia are closely associated with small accumulations of suprarenal tissue. Two axillary bodies are the largest of the sympathetic and suprarenal structures. They lie about the subclavian arteries and are made up of a gastric ganglion and a relatively large mass of chromaffin tissue. The sympathetic ganglia lie in an irregular plexus of longitudinal and crossing sympa- thetic strands but there is no regular sympathetic chain or commissure between ganglia. There are white rami communicantes which connect the sympathetic ganglia with spinal nerves. A small pregastric ganglion lies on the rami communicantes to the gastric ganglion. The visceral nerves arising from the sympathetic ganglia proceed to blood-vessels, genital ducts, chromaffin tissue, and gut. The latter is supplied by large splanchnic nerves which originate in the gastric ganglia and proceed along the coeliac axis to the intestine, pancreas, and liver. Prevertebral ganglia are absent. A mucosal and a submucosal plexus are present in the intestine. The cranial component of the autonomic system comprises a midbrain and a hindbrain outflow. -

The Orbital Apex the Orbital Apex • Review the Relationship Between the Orbital Apex and Adjacent Structures
Objectives • Understand the anatomy of the orbital apex The Orbital Apex • Review the relationship between the orbital apex and adjacent structures Barry Shpizner, MD • Discuss the imaging features of the orbital LIJ Medical Center apex in relation to adjacent anatomic Northwell Health structures New Hyde Park, NY Bony Anatomy Acknowledgments Orbit • Frontal • Richard Wiggins, MD • Zygomatic • Claudia Kirsch, MD • Maxillary • Lacrimal • Ethmoid • Palatine • Sphenoid Bony Anatomy Orbital Apex Bony Anatomy •OPTIC CANAL/OPTIC FORAMEN •SUPERIOR ORBITAL FISSURE •INFERIOR ORBITAL FISSURE •POSTEROR ETHMOID FORAMEN From Osseous Anatomy of the Orbital Apex David L. Daniels, et. al. AJNR 16:1929–1935, Oct 1995 0195-6108/95/1609–1929 Cavernous Sinus Optic Strut Superior Orbital Fissure Pterygopalatine Fossa Inferior Orbital Fissure Optic Canal Optic Strut Superior Orbital Fissure Inferior Orbital Fissure Annulus of Zinn Cranial Nerve II Annulus of Zinn Optic Nerve OCULOMOTOR FORAMEN- within annulus OPTIC TRACTS •OPTIC FORAMEN OPTIC CHIASM CN II SEGMENTS ) CN II Ophthalmic artery •Intracranial •Central Superior Orbital Fissure •Intracanalicular CN III •Intraorbital Nasociliary n. CN V1 •Intraocular- CN VI papilla SOF ABOVE ANNULUS CN V1 branches Acquires dural CN IV covering entering Superior ophth. vein optic canal SOF BELOW ANNULUS Inferior ophth. vein Optic Canal RICK Optic Nerve Cranial Nerve III Oculomotor Foramen Oculomotor Nerve NUCLEI- within ventral periaqueductal grey •Oculomotor n.- motor fibers to extraocular muscles except SO and LR -

Orbit and Contents
Orbit and Contents Mikel Snow, Ph.D. Professor Dept. Integrative Anatomical Sciences [email protected] July 15, 2019 Lecture Outline • Relationships of orbits to paranasal sinuses • Arrangement of orbital contents (fascial structures) • Structure of eyelids & lacrimal apparatus • Blood supply to the orbit and retina • Cranial nerves of the orbit (CN II, III, IV, V1, VI ) • Autonomics of the orbit (parasympathetic & sympathetic) • Extraocular muscles (actions & innervations) Relationships of the Orbit Frontal Ethmoid sinus air cells F ORBIT ORBIT E Maxillary N sinus M Nasal cavity Frontal Section Anteroposterior Radiograph through Orbit Lecture Outline • Relationships of the orbit • Arrangement of orbital contents (fascial structures) • Structure of eyelids & lacrimal apparatus • Blood supply to the orbit and retina • Cranial nerves of the orbit (CN II, III, IV, V1, VI ) • Autonomics of the orbit (parasympathetics & sympathetics • Extraocular muscles (actions & innervations) Dura mater lining the cranial cavity has two layers: Skull Periosteal Meningeal Dura Cranial Dura General Arrangement of Orbital Tarsal septum plates Orbital Fascia & Fat Periorbita (periosteum) Periosteum Orbital Dura Optic sheath: septum Fat Arachnoid Pia Superior tarsal plate Fat Bilaminar intracranial dura Inferior Fat Optic tarsal plate canal Orbital Fat septum Anatomy of the Eyelids (skeletal muscle innervated by CN III) Levator palpebrae superioris Orbital septum Superior tarsal muscle (smooth muscle innervated by sympathetics) Palpebral conjunctiva Orbicularis oculi Bulbar (skeletal) conjunctiva Conjunctival Tarsal vessels plate Skin Cilia Lacrimal Apparatus The lacrimal gland produces tears that wash across the eye from lateral to medial to moisten and aerate the cornea. A dry eye or reduced tears can lead to corneal edema. Lacrimal gland Lacrimal gland is innervated by parasympathetics from Lacrimal facial nerve.