NASAL ANATOMY Elena Rizzo Riera R1 ORL HUSE NASAL ANATOMY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Septoplasty, Rhinoplasty, Septorhinoplasty, Turbinoplasty Or
Septoplasty, Rhinoplasty, Septorhinoplasty, 4 Turbinoplasty or Turbinectomy CPAP • If you have obstructive sleep apnea and use CPAP, please speak with your surgeon about how to use it after surgery. Follow-up • Your follow-up visit with the surgeon is about 1 to 2 weeks after Septoplasty, Rhinoplasty, Septorhinoplasty, surgery. You will need to call for an appointment. Turbinoplasty or Turbinectomy • During this visit any nasal packing or stents will be removed. Who can I call if I have questions? For a healthy recovery after surgery, please follow these instructions. • If you have any questions, please contact your surgeon’s office. Septoplasty is a repair of the nasal septum. You may have • For urgent questions after hours, please call the Otolaryngologist some packing up your nose or splints which stay in for – Head & Neck (ENT) surgeon on call at 905-521-5030. 7 to 14 days. They will be removed at your follow up visit. When do I need medical help? Rhinoplasty is a repair of the nasal bones. You will have a small splint or plaster on your nose. • If you have a fever 38.5°C (101.3°F) or higher. • If you have pain not relieved by medication. Septorhinoplasty is a repair of the nasal septum and the nasal bone. You will have a small splint or plaster cast on • If you have a hot or inflamed nose, or pus draining from your nose, your nose. or an odour from your nose. • If you have an increase in bleeding from your nose or on Turbinoplasty surgery reduces the size of the turbinates in your dressing. -
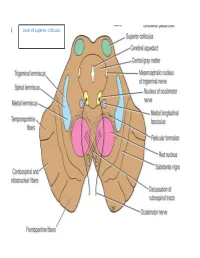
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Rhinoplasty and Septorhinoplasty These Services May Or May Not Be Covered by Your Healthpartners Plan
Rhinoplasty and septorhinoplasty These services may or may not be covered by your HealthPartners plan. Please see your plan documents for your specific coverage information. If there is a difference between this general information and your plan documents, your plan documents will be used to determine your coverage. Administrative Process Prior authorization is not required for: • Septoplasty • Surgical repair of vestibular stenosis • Rhinoplasty, when it is done to repair a nasal deformity caused by cleft lip/ cleft palate Prior authorization is required for: • Rhinoplasty for any indication other than cleft lip/ cleft palate • Septorhinoplasty Coverage Rhinoplasty is not covered for cosmetic reasons to improve the appearance of the member, but may be covered subject to the criteria listed below and per your plan documents. The service and all related charges for cosmetic services are member responsibility. Indications that are covered 1. Primary rhinoplasty (30400, 30410) may be considered medically necessary when all of the following are met: A. There is anatomical displacement of the nasal bone(s), septum, or other structural abnormality resulting in mechanical nasal airway obstruction, and B. Documentation shows that the obstructive symptoms have not responded to at least 3 months of conservative medical management, including but not limited to nasal steroids or immunotherapy, and C. Photos clearly document the structural abnormality as the primary cause of the nasal airway obstruction, and D. Documentation includes a physician statement regarding why a septoplasty would not resolve the airway obstruction. 2. Secondary rhinoplasty (30430, 30435, 30450) may be considered medically necessary when: A. The secondary rhinoplasty is needed to treat a complication/defect that was caused by a previous surgery (when the previous surgery was not cosmetic), and B. -

Nerves of the Orbit Optic Nerve the Optic Nerve Enters the Orbit from the Middle Cranial Fossa by Passing Through the Optic Canal
human anatomy 2016 lecture fourteen Dr meethak ali ahmed neurosurgeon Nerves of the Orbit Optic Nerve The optic nerve enters the orbit from the middle cranial fossa by passing through the optic canal . It is accompanied by the ophthalmic artery, which lies on its lower lateral side. The nerve is surrounded by sheath of pia mater, arachnoid mater, and dura mater. It runs forward and laterally within the cone of the recti muscles and pierces the sclera at a point medial to the posterior pole of the eyeball. Here, the meninges fuse with the sclera so that the subarachnoid space with its contained cerebrospinal fluid extends forward from the middle cranial fossa, around the optic nerve, and through the optic canal, as far as the eyeball. A rise in pressure of the cerebrospinal fluid within the cranial cavity therefore is transmitted to theback of the eyeball. Lacrimal Nerve The lacrimal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward along the upper border of the lateral rectus muscle . It is joined by a branch of the zygomaticotemporal nerve, whi(parasympathetic secretomotor fibers). The lacrimal nerve ends by supplying the skin of the lateral part of the upper lid. Frontal Nerve The frontal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward on the upper surface of the levator palpebrae superioris beneath the roof of the orbit . -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

Rhinoplasty and Septoplasty
Rhinoplasty and Septoplasty Surgically altering the nose is a common plastic surgery procedure that often has a profound impact on a patient’s life. In some cases this procedure is required to alter the internal anatomy of the nose in order to address functional breathing problems. In others a patient may desire to change the appearance of their nose. Rhinoplasty alters the external appearance of the nose, improving its shape and balance with the face. Frequently a combination of internal and external alterations are performed simultaneously. Functional Problems Airway obstruction is the most common functional nasal problem. It may be caused by either congenital or post- traumatic deformity of the nasal septum. Enlargement of the turbinates may also occur, creating an airway obstruction. All of these changes can exacerbate existing sinus problems. Cosmetic Deformity Some cosmetic deformities of the nose are post traumatic, while others are congenital. Both can be addressed similarly by surgically altering the underlying bony and cartilaginous framework of the nose. The Procedure Septoplasty and rhinoplasty are generally done on an outpatient basis and require either general anesthesia or sedation with a local. Airway problems are treated by removing or reshaping the septal cartilage. Some cases require a reduction in the size of the turbinates. Changes to the shape of the nose are accomplished by reshaping the bone and cartilage framework of the nose. In most cases the incisions can be located inside the nose resulting in no visible scars. Frequently used post-operative measures include splinting, taping and nasal packing. The Results Rhinoplasty can have a substantial effect on a person’s appearance and, ultimately, their general sense of well-being. -

Rhinoplasty ARTICLE by PHILIP WILKES, CST/CFA
Rhinoplasty ARTICLE BY PHILIP WILKES, CST/CFA hinoplasty is plastic become lodged in children's noses.3 glabella, laterally with the maxilla, surgery of the nose Fortunately, the art and science of inferiorly with the upper lateral car- for reconstructive, rhinoplasty in the hands of a skilled tilages, and posteriorly with the eth- restorative, or cos- surgical team offers positive alter- moid bone? metic purposes. The natives. The nasal septum is formed by procedure of rhmo- Three general types of rhino- the ethmoid (perpendicular plate) plasty had its beginnings in India plasty will be discussed in this arti- and vomer bones (see Figure 5). The around 800 B.c.,as an ancient art cle. They include partial, complete, cartilaginous part is formed by sep- performed by Koomas Potters.' and finesse rhinoplasties. tal and vomeronasal cartilages. The Crimes were often punished by the anterior portion consists of the amputation of the offender's nose, Anatomy and Physiology of the medial crus of the greater alar carti- creating a market for prosthetic sub- Nose lages, called the columella nasi? stitutes. The skill of the Koomas The nose is the olfactory organ that The vestibule is the cave-like area enabled them to supply this need. In projects from the center of the face modem times, rhinoplasty has and warms, filters, and moistens air developed into a high-technology on the way to the respiratory tract. procedure that combines art with Someone breathing only through the latest scientific advancements.' the mouth delivers a bolus of air During rhinoplastic procedures, with each breath. The components surgeons can change the shape and of the nose allow a thin flow of air size of the nose to improve physical to reach the lungs, which is a more appearance or breathing. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

Correlation of CT Cerebral Vascular Territories with Function: 3. Middle Cerebral Artery
161 Correlation of CT Cerebral Vascular Territories with Function: 3. Middle Cerebral Artery Stephen A. Berman 1 Schematic displays are presented of the cerebral territories supplied by branches of L. Anne Hayman2 the middle cerebral artery as they would appear on axial and coronal computed Vincent C. Hinck 1 tomographic (CT) scan sections. Companion diagrams of regional cortical function and a discussion of the fiber tracts are provided to simplify correlation of clinical deficits with coronal and axial CT abnormalities. This report is the third in a series designed to correlate cerebral vascular territories and functional anatomy in a form directly applicable to computed tomog raphy (CT). The illustrations are intended to simplify analysis of CT images in terms of clinical signs and symptoms and vascular territories in everyday practice. The anterior and posterior cerebral arteries have been described [1 , 2] . This report deals with the middle cerebral arterial territory. Knowledge of cerebral vascular territories can help in differentiating between infarction and other pathologic processes. For example, if the position and extent of a lesion and the usual position and extent of a vascular territory are incongruous, infarction should receive relatively low diagnostic priority and vice versa. Knowledge of vascular territories can also facilitate correct interpretation of cerebral angio grams by pinpointing specific vessels for particularly close attention. Knowledge of functional neuroanatomy applied to a patient's clinical findings can improve detection of subtle lesions by pinpointing specific areas for special attention on CT and specific vessels for attention on angiograms. Discussion The largest area of the brain that is normally supplied by the vessel(s) of the middle cerebral territory is indicated in figures 1 and 2. -

Vascular Supply to the Head and Neck
Vascular supply to the head and neck Sumamry This lesson covers the head and neck vascular supply. ReviseDental would like to thank @KIKISDENTALSERVICE for the wonderful drawings in this lesson. Arterial supply to the head Facial artery: Origin: External carotid Branches: submental a. superior and inferior labial a. lateral nasal a. angular a. Note: passes superiorly over the body of there mandible at the masseter Superficial temporal artery: Origin: External carotid Branches: It is a continuation of the ex carotid a. Note: terminal branch of the ex carotid a. and is in close relation to the auricular temporal nerve Transverse facial artery: Origin: Superficial temporal a. Note: exits the parotid gland Maxillary branch: supplies the areas missed from the above vasculature Origin: External carotid a. Branches: (to the face) infraorbital, buccal and inferior alveolar a.- mental a. Note: Terminal branch of the ex carotid a. The ophthalmic branches Origin: Internal carotid a. Branches: Supratrochlear, supraorbital, lacrimal, anterior ethmoid, dorsal nasal Note:ReviseDental.com enters orbit via the optic foramen Note: The face arterial supply anastomose freely. ReviseDental.com ReviseDental.com Venous drainage of the head Note: follow a similar pathway to the arteries Superficial vessels can communicate with deep structures e.g. cavernous sinus and the pterygoid plexus. (note: relevant for spread of infection) Head venous vessels don't have valves Supratrochlear vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supra-orbital v. Note: from the angular vein Supra-orbital vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supratrochlear v. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular.