PREVNAR 13 Safely and Effectively
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

362.Full.Pdf
AMERICAN ACADEMY OF PEDIATRICS Committee on Infectious Diseases Policy Statement: Recommendations for the Prevention of Pneumococcal Infections, Including the Use of Pneumococcal Conjugate Vaccine (Prevnar), Pneumococcal Polysaccharide Vaccine, and Antibiotic Prophylaxis ABSTRACT. Heptavalent pneumococcal conjugate vac- lular pertussis; HbOC, Haemophilus influenzae type b conjugate cine (PCV7) is recommended for universal use in chil- vaccine; HIV, human immunodeficiency virus; AOM, acute otitis dren 23 months and younger, to be given concurrently media. with other recommended childhood vaccines at 2, 4, 6, and 12 to 15 months of age. For children 7 to 23 months he purpose of this report is to provide recom- old who have not received previous doses of PCV7, ad- ministration of a reduced number of doses is recom- mendations for use of the heptavalent pneumo- mended. Two doses of PCV7 are recommended for chil- Tcoccal conjugate vaccine (PCV7), Prevnar (Led- dren 24 to 59 months old at high risk of invasive erle Laboratories, Pearl River, NY; Wyeth-Ayerst pneumococcal infection—including children with func- Pharmaceuticals, Marietta, PA), and 23-valent pneumo- tional, anatomic, or congenital asplenia; infection with coccal polysaccharide (23PS) vaccines. In addition, rec- human immunodeficiency virus; and other predisposing ommendations for the continuing use of antibiotic pro- conditions—who have not been immunized previously phylaxis in children with sickle cell disease (SCD) and with PCV7. Recommendations have been made for use of asplenia will be given, and the use of antibiotics and 23-valent pneumococcal polysaccharide (23PS) vaccine in vaccines in children who attend out-of-home care will high-risk children to expand serotype coverage. -

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -
Pneumococcal Vaccine
Vaccines for Primary Care Pneumococcal, Shingles, Pertussis Devang Patel, M.D. Assistant Professor Chief of Service, MICU ID Service University of Maryland School of Medicine Pneumococcal Vaccine Pneumococcal Disease • 2nd most common cause of vaccine preventable death in the US • Major Syndromes – Pneumonia – Bacteremia – Meningitis Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network Streptococcus pneumoniae, 2010 (ORIG) Vaccine Target • Polysaccharide capsule allows bacteria to resist phagocytosis • Antibodies to capsule facilitate phagocytosis • >90 different pneumococcal capsular serotypes • Vaccines contain most common serotypes causing disease Pneumococcal Vaccines Pneumococcal Vaccines • Pneumococcal polysaccharide vaccine (PPSV23; Pneumovax) – Contains capsular polysaccharides – 23 most commonly infecting serotypes • Cause 60% of all pneumococcal infections in adults – Not recommended for children <2 due to poor immunogenicity of polysaccharides Pneumococcal Vaccines • Pneumococcal conjugate vaccine (PCV13, Prevnar) – Polysaccharides linked to nontoxic protein • higher antigenicity – Stimulates mucosal antibody • Eliminates nasal carriage in young children • Herd effect in adults – Reduction in PCV7 serotype disease >90% Prevnar 13 • 2000 - PCV7 approved for infants toddlers • 2010 - PCV13 recommended for infants and toddlers • 2012 – ACIP recommended PCV13 for high- risk adults • 2014 – recommended for adults >65 • 2018 – ACIP will revisit PCV13 use in adults – Childhood vaccines may eliminate -

The Hepatitis B Vaccine Is the Most Widely Used Vaccine in the World, with Over 1 Billion Doses Given
Hepatitis B Vaccine Protect Yourself and Those You Love What is Hepatitis B? Hepatitis B is the most common serious liver infection in the world. It is caused by the hepatitis B virus (HBV), which attacks liver cells and can lead to liver failure, cirrhosis (scarring), or liver cancer later in life. The virus is transmitted through direct contact with infected blood and bodily fluids, and from an infected woman to her newborn at birth. Is there a safe vaccine for hepatitis B? YES! The good news is that there is a safe and effective vaccine for hepatitis B. The vaccine is a series, typically given as three shots over a six-month period that will provide a lifetime of protection. You cannot get hepatitis B from the vaccine – there is no human blood or live virus in the vaccine. The hepatitis B vaccine is the most widely used vaccine in the world, with over 1 billion doses given. The hepatitis B vaccine is the first "anti-cancer" vaccine because it can help prevent liver cancer! Who should be vaccinated against hepatitis B? The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) recommend the hepatitis B vaccine for all newborns and children up to 18 years of age, and all high-risk adults. All infants should receive the first dose of the vaccine in the delivery room or in the first 24 hours of life, preferably within 12 hours. (CDC recommends the first dose within 12 hours vs. the WHO recommendation of 24 hours.) The HBV vaccine is recommended to anyone who is at high risk of infection. -

Engerix-B Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME ENGERIX-B 20 micrograms/mL, suspension for injection. ENGERIX-B paediatric 10 micrograms/0.5 mL, suspension for injection. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION ENGERIX-B paediatric dose: 10 microgram (µg) dose vaccine 1 dose (0.5 mL) contains: Hepatitis B surface antigen 1, 2 10 micrograms 1Adsorbed on aluminium hydroxide, hydrated Total: 0.25 milligrams Al3+ 2Produced in yeast cells (Saccharomyces cerevisiae) by recombinant DNA technology ENGERIX-B: 20 microgram (µg) dose vaccine 1 dose (1 mL) contains: Hepatitis B surface antigen1, 2 20 micrograms 1Adsorbed on aluminium hydroxide, hydrated Total: 0.50 milligrams Al3+ 2Produced in yeast cells (Saccharomyces cerevisiae) by recombinant DNA technology The vaccine is highly purified, and meets the WHO requirements for recombinant hepatitis B vaccines. No substances of human origin are used in its manufacture. For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Suspension for injection. ENGERIX-B is a turbid white suspension. Upon storage, a fine white deposit with a clear colourless supernatant may be observed. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications ENGERIX-B is indicated for active immunisation against hepatitis B virus infection. As part of the national immunisation schedule, the New Zealand Ministry of Health* recommend all infants, unvaccinated children up to the age of 16 years, and household and sexual contacts of known hepatitis B carriers receive a primary course of vaccination against hepatitis B. 1 Immunisation is also recommended for seronegative persons who are at substantial risk and have been demonstrated or judged to be susceptible to the hepatitis B virus (HBV). -
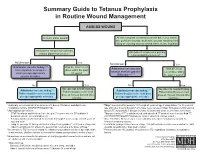
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

YF-VAX® Rx Only AHFS Category
YF-VAX® Rx Only Laboratory Personnel AHFS Category: 80:12 Laboratory personnel who handle virulent yellow fever virus or concentrated preparations Rx only of the yellow fever vaccine virus strains may be at risk of exposure by direct or indirect Yellow Fever Vaccine contact or by aerosols. (14) DESCRIPTION CONTRAINDICATIONS ® Hypersensitivity YF-VAX , Yellow Fever Vaccine, for subcutaneous use, is prepared by culturing the YF-VAX is contraindicated in anyone with a history of acute hypersensitivity reaction to any 17D-204 strain of yellow fever virus in living avian leukosis virus-free (ALV-free) chicken component of the vaccine. (See DESCRIPTION section.) Because the yellow fever virus embryos. The vaccine contains sorbitol and gelatin as a stabilizer, is lyophilized, and is used in the production of this vaccine is propagated in chicken embryos, do not administer hermetically sealed under nitrogen. No preservative is added. Each vial of vaccine is YF-VAX to anyone with a history of acute hypersensitivity to eggs or egg products due to supplied with a separate vial of sterile diluent, which contains Sodium Chloride Injection a risk of anaphylaxis. Less severe or localized manifestations of allergy to eggs or to USP – without a preservative. YF-VAX is formulated to contain not less than 4.74 log10 feathers are not contraindications to vaccine administration and do not usually warrant plaque forming units (PFU) per 0.5 mL dose throughout the life of the product. Before vaccine skin testing. (See PRECAUTIONS section, Testing for Hypersensitivity Re- reconstitution, YF-VAX is a pinkish color. After reconstitution, YF-VAX is a slight pink-brown actions subsection.) Generally, persons who are able to eat eggs or egg products may suspension. -

Vaccines for Preteens
| DISEASES and the VACCINES THAT PREVENT THEM | INFORMATION FOR PARENTS Vaccines for Preteens: What Parents Should Know Last updated JANUARY 2017 Why does my child need vaccines now? to get vaccinated. The best time to get the flu vaccine is as soon as it’s available in your community, ideally by October. Vaccines aren’t just for babies. Some of the vaccines that While it’s best to be vaccinated before flu begins causing babies get can wear off as kids get older. And as kids grow up illness in your community, flu vaccination can be beneficial as they may come in contact with different diseases than when long as flu viruses are circulating, even in January or later. they were babies. There are vaccines that can help protect your preteen or teen from these other illnesses. When should my child be vaccinated? What vaccines does my child need? A good time to get these vaccines is during a yearly health Tdap Vaccine checkup. Your preteen or teen can also get these vaccines at This vaccine helps protect against three serious diseases: a physical exam required for sports, school, or camp. It’s a tetanus, diphtheria, and pertussis (whooping cough). good idea to ask the doctor or nurse every year if there are any Preteens should get Tdap at age 11 or 12. If your teen didn’t vaccines that your child may need. get a Tdap shot as a preteen, ask their doctor or nurse about getting the shot now. What else should I know about these vaccines? These vaccines have all been studied very carefully and are Meningococcal Vaccine safe. -
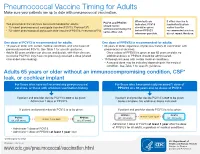
Pneumococcal Vaccine Timing for Adults Make Sure Your Patients Are up to Date with Pneumococcal Vaccination
Pneumococcal Vaccine Timing for Adults Make sure your patients are up to date with pneumococcal vaccination. When both are If either vaccine is PCV13 and PPSV23 Two pneumococcal vaccines are recommended for adults: indicated, PCV13 inadvertently given should not be 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar13®) should be given earlier than the administered during the ® before PPSV23 recommended window, 23-valent pneumococcal polysaccharide vaccine (PPSV23, Pneumovax 23) same office visit. whenever possible. do not repeat the dose. One dose of PCV13 is recommended for adults: One dose of PPSV23 is recommended for adults: 19 years or older with certain medical conditions and who have not 65 years or older, regardless of previous history of vaccination with previously received PCV13. See Table 1 for specific guidance. pneumococcal vaccines. Adults 65 years or older can discuss and decide, with their clinician, – Once a dose of PPSV23 is given at age 65 years or older, no to receive PCV13 if they have not previously received a dose (shared additional doses of PPSV23 should be administered. clinical decision-making). 19 through 64 years with certain medical conditions. – A second dose may be indicated depending on the medical condition. See Table 1 for specific guidance. Adults 65 years or older without an immunocompromising condition, CSF* leak, or cochlear implant For those who have not received any pneumococcal For those who have previously received 1 dose of vaccines, or those with unknown vaccination history PPSV23 at ≥ 65 years and no doses of PCV13 If patient and provider decide PCV13 is not to be given: If patient and provider decide PCV13 is not to be given: Administer 1 dose of PPSV23. -
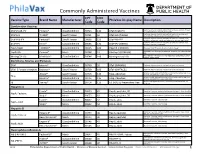
Commonly Administered Vaccines
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular -

Adults with DIABETES Are Among Those Who Need Pneumococcal
Patients with diabetes are at an increased risk for complications from pneumococcal disease. Diabetes may be a unique risk factor for increased incidence of sepsis associated with pneumococcal infection. One of the reasons people with diabetes are at greater risk for pneumococcal disease is that they may have abnormalities in immune function that affect their reaction to infection. Pneumococcal disease causes serious illnesses like pneumonia, meningitis, and sepsis. Pneumococcal disease is serious and deadly. In the US, pneumococcal pneumonia, meningitis, and sepsis kill tens of thousands each year. Pneumococcal disease survivors may suffer hearing loss, seizures, blindness, or paralysis. Pneumococcal vaccination is recommended for all adults with diabetes. Adults with DIABETES Are Among Those Who Need Pneumococcal Vaccination There are two types of pneumococcal vaccine recommended for US adults: a pneumococcal conjugate vaccine (PCV13) and a pneumococcal polysaccharide vaccine (PPSV23). Adults 65 and older, and adults age 19 to 64 years with any of the following need to receive both vaccines: immunocompromising conditions or treatments (e.g., HIV/AIDS, leukemia, lymphoma, Hodgkin disease, radiation therapy); a damaged or missing spleen; cochlear implants; or cerebrospinal fluid leaks. Other adults for whom pneumococcal vaccination is recommended only need PPSV23, but may need more than one dose and will need PCV13 when they, too, reach age 65. Please refer to the Adult Pneumococcal Vaccination Guide or visit cdc.gov/vaccines/vpd-vac/pneumo/ for details on timing of vaccine doses. For more information and resources to educate patients about pneumococcal disease, visit adultvaccination.org/professional-resources/pneumo This initiative is supported by unrestricted educational grants from Merck & Co., Inc. -

Vaccine Hesitancy
Vaccine Hesitancy Dr Brenda Corcoran National Immunisation Office Presentation Outline An understanding of the following principles: • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow – thymus – lymphatic system of ducts and nodes – spleen –blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (antitoxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need boosting How vaccines work • Induce active immunity – Immunity and immunologic memory similar to natural infection but without risk of disease • Immunological memory allows – Rapid recognition and response to pathogen – Prevent or modify effect of disease Live attenuated vaccines Weakened viruses /bacteria – Achieved by growing numerous generations in laboratory – Produces long lasting immune response after one or two doses – Stimulates immune system to react as it does to natural infection – Can cause mild form of the disease (e.g.