Safety of Immunization During Pregnancy a Review of the Evidence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
FDA Guidance on Establishing Pregnancy Exposure Registries
Guidance for Industry Establishing Pregnancy Exposure Registries U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) August 2002 Clinical/Medical Guidance for Industry Establishing Pregnancy Exposure Registries Additional copies are available from: Office of Training and Communications Division of Communications Management Drug Information Branch, HFD-210 5600 Fishers Lane Rockville, MD 20857 (Tel) 301-827-4573 http://www.fda.gov/cder/guidance/index.htm or Office of Communication, Training, and Manufacturers Assistance (HFM-40) Center for Biologics Evaluation and Research (CBER) 1401 Rockville Pike, Rockville, MD 20852-1448 http://www.fda.gov/cber/guidelines.htm (Fax) 888-CBERFAX or 301-827-3844 (Voice Information) 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) August 2002 Clinical/Medical TABLE OF CONTENTS I. INTRODUCTION................................................................................................................. 1 II. BACKGROUND ...................................................................................................................1 III. WHAT IS A PREGNANCY EXPOSURE REGISTRY? .................................................. 2 IV. WHAT MEDICAL PRODUCTS MAKE GOOD REGISTRY CANDIDATES?........... 3 V. WHEN SHOULD SUCH A REGISTRY BE ESTABLISHED?...................................... -

2018 Infant Mortality Annual Report 2 Ohio Infant Mortality Report 2018 TABLE of CONTENTS
2018 Infant Mortality Annual Report 2 Ohio Infant Mortality Report 2018 TABLE OF CONTENTS EXECUTIVE SUMMARY 4 SECTION 1: GENERAL FINDINGS 5-10 Ohio Infant Mortality Rate by Race and Ethnicity (2016-2018) 5 Trends in Ohio Infant Mortality (2009-2018) 6 Ohio Five-Year Average Infant Mortality Rates by County 8 Neonatal and Postneonatal Mortality Rates 9-10 SECTION 2: A DEEPER LOOK 11-19 Infant Mortality by Duration of Gestation and Birthweight 11-12 Risk Factors among Ohio Infant Deaths 13-14 Leading Causes of Infant Deaths 15-16 Prematurity-Related Infant Deaths 17 External Injury-Related Infant Deaths 18 Deaths to Infants Less Than 24 Weeks Gestation 19 DATA SOURCES AND METHODS 20 DEFINITIONS 21-22 REFERENCES 23 APPENDICES 24-45 Appendix A: The Ohio Equity Institute (OEI) 24-25 Appendix B: Sleep-Related Deaths 26-29 Appendix C: Supplementary Data Tables 30-45 Section 1: County-Level Infant Mortality Data 30-36 Section 2: A Deeper Look 37-45 3 EXECUTIVE SUMMARY Ohio has identified infant mortality as a priority in its 2017-2019 State Health Improvement Plan (SHIP)1. Infant mortality is the death of an infant before his or her first birthday. The Infant Mortality Rate is the number of infant deaths per 1,000 live births. The Infant Mortality Rate not only serves as a key indicator of maternal and infant health but is also an important measure of the health status of a community. In 2018, the infant mortality rate fell to 6.9 from 7.2 in 2017 for all races. -

Low Birthweight
OECD Health Statistics 2021 Definitions, Sources and Methods Low birthweight Number of live births weighing less than 2500 grams as a percentage of the total number of live births. Sources and Methods Australia Source: Australian Institute of Health and Welfare. From 1991: Australia’s mothers and babies reports available to download at https://www.aihw.gov.au/reports- statistics/population-groups/mothers-babies/reports. - From 2013 onwards, the Australian Institute of Health and Welfare has produced the data. - From 1991 to 2012, the National Perinatal Epidemiology and Statistics Unit produced the data on behalf of the Australian Institute of Health and Welfare. Before 1991: State and Territory maternal and perinatal collections. Break in time series in 1991: Before 1991, data refer to selected states and territories only and have total births (live births + stillbirths) as a denominator. Further information: https://www.aihw.gov.au/reports-statistics/population-groups/mothers-babies/overview. Austria Source: Statistics Austria, Gesundheitsstatistisches Jahrbuch (Health Statistics Report), Lebendgeborene nach Geburtsgewicht (Live births by birth weight) (several issues). Further information: http://www.statistik.at/web_en/. Belgium Source: Federal Public Service Economic Affairs - Directorate General for statistical and economic information (former National Statistical Institute). Methodology: Since 2010, the official numbers for livebirths and deaths are coming from the Population National Register (and not exclusively from vital registration). Livebirths and deaths of residents taking place in foreign countries are therefore included in the statistics. Canada Source: Statistics Canada. Canadian Vital Statistics Birth Database. From 1979: Table 13-10-0404-01 (formerly CANSIM 102-4005). 1961-1978: Births, 1991, Cat. No. -
(ACIP) General Best Guidance for Immunization
9. Special Situations Updates Major revisions to this section of the best practices guidance include the timing of intramuscular administration and the timing of clotting factor deficiency replacement. Concurrent Administration of Antimicrobial Agents and Vaccines With a few exceptions, use of an antimicrobial agent does not interfere with the effectiveness of vaccination. Antibacterial agents have no effect on inactivated, recombinant subunit, or polysaccharide vaccines or toxoids. They also have no effect on response to live, attenuated vaccines, except BCG vaccines. Antimicrobial or immunosuppressive agents may interfere with the immune response to BCG and should only be used under medical supervision (for additional information, see www.merck.com/product/usa/pi_circulars/b/bcg/bcg_pi.pdf). Antiviral drugs used for treatment or prophylaxis of influenza virus infections have no effect on the response to inactivated influenza vaccine (2). However, live, attenuated influenza vaccine should not be administered until 48 hours after cessation of therapy with antiviral influenza drugs. If feasible, to avoid possible reduction in vaccine effectiveness, antiviral medication should not be administered for 14 days after LAIV administration (2). If influenza antiviral medications are administered within 2 weeks after receipt of LAIV, the LAIV dose should be repeated 48 or more hours after the last dose of zanamavir or oseltamivir. The LAIV dose should be repeated 5 days after peramivir and 17 days after baloxavir. Alternatively, persons receiving antiviral drugs within the period 2 days before to 14 days after vaccination with LAIV may be revaccinated with another approved vaccine formulation (e.g., IIV or recombinant influenza vaccine). Antiviral drugs active against herpesviruses (e.g., acyclovir or valacyclovir) might reduce the efficacy of vaccines containing live, attenuated varicella zoster virus (i.e., Varivax and ProQuad) (3,4). -
Pneumococcal Vaccine
Vaccines for Primary Care Pneumococcal, Shingles, Pertussis Devang Patel, M.D. Assistant Professor Chief of Service, MICU ID Service University of Maryland School of Medicine Pneumococcal Vaccine Pneumococcal Disease • 2nd most common cause of vaccine preventable death in the US • Major Syndromes – Pneumonia – Bacteremia – Meningitis Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network Streptococcus pneumoniae, 2010 (ORIG) Vaccine Target • Polysaccharide capsule allows bacteria to resist phagocytosis • Antibodies to capsule facilitate phagocytosis • >90 different pneumococcal capsular serotypes • Vaccines contain most common serotypes causing disease Pneumococcal Vaccines Pneumococcal Vaccines • Pneumococcal polysaccharide vaccine (PPSV23; Pneumovax) – Contains capsular polysaccharides – 23 most commonly infecting serotypes • Cause 60% of all pneumococcal infections in adults – Not recommended for children <2 due to poor immunogenicity of polysaccharides Pneumococcal Vaccines • Pneumococcal conjugate vaccine (PCV13, Prevnar) – Polysaccharides linked to nontoxic protein • higher antigenicity – Stimulates mucosal antibody • Eliminates nasal carriage in young children • Herd effect in adults – Reduction in PCV7 serotype disease >90% Prevnar 13 • 2000 - PCV7 approved for infants toddlers • 2010 - PCV13 recommended for infants and toddlers • 2012 – ACIP recommended PCV13 for high- risk adults • 2014 – recommended for adults >65 • 2018 – ACIP will revisit PCV13 use in adults – Childhood vaccines may eliminate -

Proquad, INN-Measles, Mumps, Rubella and Varicella Vaccine (Live)
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT ProQuad powder and solvent for suspension for injection ProQuad powder and solvent for suspension for injection in a pre-filled syringe Measles, mumps, rubella and varicella vaccine (live). 2. QUALITATIVE AND QUANTITATIVE COMPOSITION After reconstitution, one dose (0.5 mL) contains: 1 Measles virus Enders’ Edmonston strain (live, attenuated) ........ not less than 3.00 log10 TCID * 50 1 Mumps virus Jeryl Lynn™ (Level B) strain (live, attenuated) ... not less than 4.30 log10 TCID * 50 2 Rubella virus Wistar RA 27/3 strain (live, attenuated)............... not less than 3.00 log10 TCID * 50 3 Varicella virus Oka/Merck strain (live, attenuated) ................... not less than 3.99 log10 PFU** *50% tissue culture infectious dose **plaque-forming units (1) Produced in chick embryo cells. (2) Produced in human diploid lung (WI-38) fibroblasts. (3) Produced in human diploid (MRC-5) cells. The vaccine may contain traces of recombinant human albumin (rHA). This vaccine contains a trace amount of neomycin. See section 4.3. Excipient(s) with known effect The vaccine contains 16 milligrams of sorbitol per dose. See section 4.4. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder and solvent for suspension for injection Before reconstitution, the powder is a white to pale yellow compact crystalline cake and the solvent is a clear colourless liquid. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications ProQuad is indicated for simultaneous vaccination against measles, mumps, rubella and varicella in individuals from 12 months of age. ProQuad can be administered to individuals from 9 months of age under special circumstances (e.g., to conform with national vaccination schedules, outbreak situations, or travel to a region with high prevalence of measles; see sections 4.2, 4.4, and 5.1). -

Summary of the WHO Position on Rubella Vaccine- July 2020 This
Summary of the WHO position on Rubella Vaccine- July 2020 This document replaces the WHO position paper on rubella vaccine published in the Weekly Epidemiological Record in July 2011. It incorporates the most recent developments in the field of rubella vaccines to provide updated guidance on the introduction and use of rubella-containing vaccines (RCVs) in national immunization schedules. It specifically updates guidance on co- administration of rubella vaccine with yellow fever (YF) vaccine and updates data and the WHO position on the control and elimination of rubella. Background Rubella is of public health importance because of the teratogenic potential of infections acquired during pregnancy. Rubella virus is generally recognized as the most common infectious cause of birth defects, accounting for an estimated 100 000 infants born with congenital rubella syndrome (CRS) each year worldwide. Infection with rubella virus within 12 days of conception and early pregnancy (usually within the first 8–10 weeks) may result in miscarriage, fetal death or CRS. For the rest of the population, rubella is an acute, usually mild viral infection transmitted by respiratory droplets, which affects susceptible children and adults worldwide. A number of live, attenuated rubella vaccines are currently available. Most rubella vaccines are available in combination with other vaccine antigens such as measles, mumps and varicella (MR, MMR, MMRV, respectively) and also in a monovalent formulation. WHO position In light of the global burden of CRS, the proven efficacy, effectiveness and safety of RCVs and regional elimination goals, WHO recommends that countries introduce RCVs into their national immunization programmes. This recommendation includes the opportunity offered by accelerated measles elimination activities to achieve both goals. -

Adult Vaccines
What do flu, whooping cough, measles, shingles and pneumonia have in common? 1 They’re viruses that can make you very sick. 2 Vaccines can help prevent them. Protect yourself and those you care about. Get vaccinated at a network pharmacy near you. • Ask your pharmacist which vaccines are right for you. • Find out if your pharmacist can administer the recommended vaccinations. • Many vaccinations are covered by your plan at participating retail pharmacies. • Don’t forget to present your member ID card to the pharmacist at the time of service! The following vaccines are available and can be administered by pharmacists at participating network pharmacies: • Flu (seasonal influenza) • Meningitis • Travel Vaccines (typhoid, yellow • Tetanus/Diphtheria/Pertussis • Pneumonia fever, etc.) • Hepatitis • Rabies • Childhood Vaccines (MMR, etc.) • Human Papillomavirus (HPV) • Shingles/Zoster See other side for recommended adult vaccinations. The vaccinations you need ALL adults should get vaccinated for1: • Flu, every year. It’s especially important for pregnant women, older adults and people with chronic health conditions. • Tetanus, diphtheria and pertussis (whooping cough). Adults should get a one-time dose of the Tdap vaccine. It’s different from the tetanus vaccine (Td), which is given every 10 years. You may need additional vaccinations depending on your age1: Young adults not yet vaccinated need: Human papillomavirus (HPV) vaccine series (3 doses) if you are: • Female age 26 or younger • Male age 21 or younger • Male age 26 or younger who has sex with men, who is immunocompromised or who has HIV Adults born in the U.S. in 1957 or after need: Measles, mumps, rubella (MMR) vaccine2 Adults should get at least one dose of MMR vaccine, unless they’ve already gotten this vaccine or have immunity to measles, mumps and rubella Adults born in the U.S. -
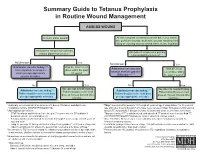
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -
Hiv Prevention in Maternal Health Services Programming Guide
PREVENTING HIV,PROMOTING REPRODUCTIVE HEALTH HIV PREVENTION IN MATERNAL HEALTH SERVICES PROGRAMMING GUIDE HIV Prevention in Maternal Health Services: Programming Guide © 2004 UNFPA and EngenderHealth. All rights reserved. United Nations Population Fund 220 East 42nd Street New York, NY 10017 U.S.A. www.unfpa.org EngenderHealth 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible through financial support provided by UNFPA. Design: Deb Lake Typesetting: ConsolidatedGraphics Cover design: Cassandra Cook Cover photo credits: Liz Gilbert, on behalf of the David and Lucile Packard Foundation Printing: Automated Graphics Systems, Inc. ISBN 0-89714-694-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication data are available from the publisher. CONTENTS Acknowledgements v • Making Services Friendlier for Stigmatised Populations 55 Introduction 1 • Universal Precautions 57 • Why Was This Guide Developed? 3 • Safer Delivery Practises 58 • What Is Covered in This Guide? 5 • Staff Training 59 • How Was This Guide Developed? 6 • Facilitative Supervision 61 • Who Is This Guide For? 7 • Programme Resources 62 • How Can This Guide Be Used? 8 • How Is This Guide Organised? 8 Chapter 3: Training Topics 67 Chapter 1: Programme Planning 11 • Basic HIV and STI Orientation 69 • Planning Process 13 • Group Education Strategies 70 • Step 1: Needs Assessment 14 • Core Counselling -

Conventional Gasoline
Conventional Gasoline M a t e r i a l S a f e t y D a t a S h e e t 1. PRODUCT AND COMPANY IDENTIFICATION Product Name: Conventional Gasoline MSDS Code: 251720 Synonyms: Gasoline, Unleaded, Conventional (All Grades); Gasoline, Low Sulfur Unleaded (All Grades) Intended Use: Fuel Responsible Party: ConocoPhillips 600 N. Dairy Ashford Houston, Texas 77079-1175 Customer Service: 800-640-1956 Technical Information: 800-255-9556 MSDS Information: Phone: 800-762-0942 Email: [email protected] Internet: http://w3.conocophillips.com/NetMSDS/ Emergency Telephone Numbers: Chemtrec: 800-424-9300 (24 Hours) California Poison Control System: 800-356-3219 2. HAZARDS IDENTIFICATION Emergency Overview NFPA DANGER! Extremely Flammable Liquid and Vapor Skin Irritant Aspiration Hazard Appearance: Clear to amber Physical Form: Liquid Odor: Gasoline Potential Health Effects Eye: Contact may cause mild eye irritation including stinging, watering, and redness. Skin: Skin irritant. Contact may cause redness, itching, a burning sensation, and skin damage. Prolonged or repeated contact can defat the skin, causing drying and cracking of the skin, and possibly dermatitis (inflammation). Not acutely toxic by skin absorption, but prolonged or repeated skin contact may be harmful (see Section 11). Inhalation (Breathing): Low to moderate degree of toxicity by inhalation. Ingestion (Swallowing): Low degree of toxicity by ingestion. ASPIRATION HAZARD - This material can enter lungs during swallowing or vomiting and cause lung inflammation and damage. Signs and Symptoms: Effects of overexposure may include nausea, vomiting, flushing, blurred vision, tremors, respiratory failure, signs of nervous system depression (e.g., headache, drowsiness, dizziness, loss of coordination, disorientation and fatigue), unconsciousness, convulsions, death. -

YF-VAX® Rx Only AHFS Category
YF-VAX® Rx Only Laboratory Personnel AHFS Category: 80:12 Laboratory personnel who handle virulent yellow fever virus or concentrated preparations Rx only of the yellow fever vaccine virus strains may be at risk of exposure by direct or indirect Yellow Fever Vaccine contact or by aerosols. (14) DESCRIPTION CONTRAINDICATIONS ® Hypersensitivity YF-VAX , Yellow Fever Vaccine, for subcutaneous use, is prepared by culturing the YF-VAX is contraindicated in anyone with a history of acute hypersensitivity reaction to any 17D-204 strain of yellow fever virus in living avian leukosis virus-free (ALV-free) chicken component of the vaccine. (See DESCRIPTION section.) Because the yellow fever virus embryos. The vaccine contains sorbitol and gelatin as a stabilizer, is lyophilized, and is used in the production of this vaccine is propagated in chicken embryos, do not administer hermetically sealed under nitrogen. No preservative is added. Each vial of vaccine is YF-VAX to anyone with a history of acute hypersensitivity to eggs or egg products due to supplied with a separate vial of sterile diluent, which contains Sodium Chloride Injection a risk of anaphylaxis. Less severe or localized manifestations of allergy to eggs or to USP – without a preservative. YF-VAX is formulated to contain not less than 4.74 log10 feathers are not contraindications to vaccine administration and do not usually warrant plaque forming units (PFU) per 0.5 mL dose throughout the life of the product. Before vaccine skin testing. (See PRECAUTIONS section, Testing for Hypersensitivity Re- reconstitution, YF-VAX is a pinkish color. After reconstitution, YF-VAX is a slight pink-brown actions subsection.) Generally, persons who are able to eat eggs or egg products may suspension.