Summary of the WHO Position on Rubella Vaccine- July 2020 This
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -

Proquad, INN-Measles, Mumps, Rubella and Varicella Vaccine (Live)
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT ProQuad powder and solvent for suspension for injection ProQuad powder and solvent for suspension for injection in a pre-filled syringe Measles, mumps, rubella and varicella vaccine (live). 2. QUALITATIVE AND QUANTITATIVE COMPOSITION After reconstitution, one dose (0.5 mL) contains: 1 Measles virus Enders’ Edmonston strain (live, attenuated) ........ not less than 3.00 log10 TCID * 50 1 Mumps virus Jeryl Lynn™ (Level B) strain (live, attenuated) ... not less than 4.30 log10 TCID * 50 2 Rubella virus Wistar RA 27/3 strain (live, attenuated)............... not less than 3.00 log10 TCID * 50 3 Varicella virus Oka/Merck strain (live, attenuated) ................... not less than 3.99 log10 PFU** *50% tissue culture infectious dose **plaque-forming units (1) Produced in chick embryo cells. (2) Produced in human diploid lung (WI-38) fibroblasts. (3) Produced in human diploid (MRC-5) cells. The vaccine may contain traces of recombinant human albumin (rHA). This vaccine contains a trace amount of neomycin. See section 4.3. Excipient(s) with known effect The vaccine contains 16 milligrams of sorbitol per dose. See section 4.4. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder and solvent for suspension for injection Before reconstitution, the powder is a white to pale yellow compact crystalline cake and the solvent is a clear colourless liquid. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications ProQuad is indicated for simultaneous vaccination against measles, mumps, rubella and varicella in individuals from 12 months of age. ProQuad can be administered to individuals from 9 months of age under special circumstances (e.g., to conform with national vaccination schedules, outbreak situations, or travel to a region with high prevalence of measles; see sections 4.2, 4.4, and 5.1). -

Vaccine Information for PARENTS and CAREGIVERS
NATIONAL INSTITUTE FOR COMMUNICABLE DISEASES Division of the National Health Laboratory Service VACCINE INFOR MATION FOR PARENTS & CAREGIVERS First Edition November 2016 Editors-in-Chief Nkengafac Villyen Motaze (MD, MSc, PhD fellow), Melinda Suchard (MBBCh, FCPath (SA), MMed) Edited by: Cheryl Cohen, (MBBCh, FCPath (SA) Micro, DTM&H, MSc (Epi), Phd) Lee Baker, (Dip Pharm) Lucille Blumberg, (MBBCh, MMed (Micro) ID (SA) FFTM (RCPS, Glasgow) DTM&H DOH DCH) Published by: Ideas Wise and Wonderful (IWW) for National Institute for Communicable Diseases (NICD) First Edition: Copyright © 2016 Contributions by: Clement Adu-Gyamfi (BSc Hons, MSc), Jayendrie Thaver (BSc), Kerrigan McCarthy, (MBBCh, FCPath (SA), DTM&H, MPhil (Theol) Kirsten Redman (BSc Hons), Nishi Prabdial-Sing (PhD), Nonhlanhla Mbenenge (MBBCh, MMED) Philippa Hime (midwife), Vania Duxbury (BSc Hons), Wayne Howard (BSc Hons) Acknowledgments: Amayeza, Vaccine Information Centre (http://www.amayeza-info.co.za/) Centre for Communicable Diseases Fact Sheets (http://www.cdc.gov/vaccines/hcp/vis/) World Health Organization Fact Sheets (http://www.who.int/mediacentre/factsheets/en/) National Department of Health, South Africa (http://www.health.gov.za/) Disclaimer This book is intended as an educational tool only. Information may be subject to change as schedules or formulations are updated. Summarized and simplified information is presented in this booklet. For full prescribing information and contraindications for vaccinations, please consult individual package inserts. There has been -
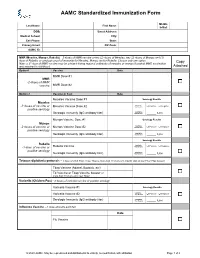
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -

Recommended Adult Immunization Schedule
Recommended Adult Immunization Schedule UNITED STATES for ages 19 years or older 2021 Recommended by the Advisory Committee on Immunization Practices How to use the adult immunization schedule (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Determine recommended Assess need for additional Review vaccine types, Control and Prevention (www.cdc.gov), American College of Physicians 1 vaccinations by age 2 recommended vaccinations 3 frequencies, and intervals (www.acponline.org), American Academy of Family Physicians (www.aafp. (Table 1) by medical condition and and considerations for org), American College of Obstetricians and Gynecologists (www.acog.org), other indications (Table 2) special situations (Notes) American College of Nurse-Midwives (www.midwife.org), and American Academy of Physician Assistants (www.aapa.org). Vaccines in the Adult Immunization Schedule* Report y Vaccines Abbreviations Trade names Suspected cases of reportable vaccine-preventable diseases or outbreaks to the local or state health department Haemophilus influenzae type b vaccine Hib ActHIB® y Clinically significant postvaccination reactions to the Vaccine Adverse Event Hiberix® Reporting System at www.vaers.hhs.gov or 800-822-7967 PedvaxHIB® Hepatitis A vaccine HepA Havrix® Injury claims Vaqta® All vaccines included in the adult immunization schedule except pneumococcal 23-valent polysaccharide (PPSV23) and zoster (RZV) vaccines are covered by the Hepatitis A and hepatitis B vaccine HepA-HepB Twinrix® Vaccine Injury Compensation Program. Information on how to file a vaccine injury Hepatitis B vaccine HepB Engerix-B® claim is available at www.hrsa.gov/vaccinecompensation. Recombivax HB® Heplisav-B® Questions or comments Contact www.cdc.gov/cdc-info or 800-CDC-INFO (800-232-4636), in English or Human papillomavirus vaccine HPV Gardasil 9® Spanish, 8 a.m.–8 p.m. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Vaccine Names and Abbreviations Vaccine Names and Abbreviations Many Vaccines Are Documented in an Abbreviation and Not by Their Full Name
Vaccine Names and Abbreviations Vaccine Names and Abbreviations Many vaccines are documented in an abbreviation and not by their full name. This page is designed to assist you in interpreting both old and new immunization records such as the yellow California Immunization Record, the International Certificate of Vaccination (Military issued shot record) or the Mexican Immunization Card described in the shaded sections. Vaccine Abbreviation/Name What it Means Polio Oral Polio oral poliovirus vaccine (no longer used in U.S.) OPV Orimune Trivalent Polio TOPV Sabin oral poliovirus Inactivated Polio injectable poliovirus vaccine eIPV IPOL IPV Pentacel combination vaccine: DTaP/Hib/IPV Pediarix combination vaccine: diphtheria, tetanus, acellular pertussis, Haemophilus influenzae type b and inactivated poliovirus (DTaP/IPV/Hep B) DTP or DPT combination vaccine: diphtheria, tetanus, pertussis (no longer DTP Tri-Immunol available in U.S.) (Diphtheria, Tetanus, Pertussis) Triple combination vaccine: difteria, tétano, tos ferina (diphtheria, tetanus pertussis) DT combination vaccine: diphtheria and tetanus vaccine (infant vaccine without pertussis component used through age 6) DTaP combination vaccine: diphtheria, tetanus and acellular pertussis DTaP/Tdap Acel-Imune Certiva (Diphtheria, Tetanus, acellular Daptacel Pertussis) Infanrix Tripedia Tdap combination vaccine: tetanus, diphtheria, acellular pertussis Adacel (improved booster vaccine containing pertussis for adolescents Boostrix and adults) DTP-Hib combination vaccine: diphtheria, tetanus, -

Adult Immunizations
Guidelines for Clinical Care Ambulatory Immunizations Guideline Team Adult Immunizations Team Leads Susan F Engert, MD, MPH Population: Adults, >18 years old Pediatrics and Communi- cable Diseases Objectives: Implement an evidence-based strategy for routine adult immunizations. Candia B Laughlin, RN, Key Points MS Routine immunizations for adults are: hepatitis A, hepatitis B, herpes zoster, human papilloma virus, Ambulatory Care Nursing Administration influenza, measles, mumps, rubella, meningococcal, pneumococcal, tetanus, diphtheria, pertussis and Team Members varicella. Below is a summary on priority populations, initial vaccination, and revaccination. Margie C Andreae, MD Use combination vaccines whenever possible to increase the coverage rates for vaccine-preventable Pediatrics and Communi- diseases: Tetanus-diphtheria (Td), Tetanus-diphtheria-acellular pertussis (Tdap), Measles-Mumps- cable Diseases Rubella (MMR), hepatitis A-hepatitis B (Twinrix®). Single antigen vaccines have no safety advantage. Mary K.Barry-Bodine, Live virus vaccines (Herpes Zoster, Measles-Mumps-Rubella, Varicella and Live Attenuated Influenza RN, BSN Vaccine) are contraindicated in persons who are pregnant or may become pregnant in the next four Nursing, Health Centers weeks, or who have immunocompromising conditions. If administering multiple live vaccines, give Susan G Blitz, MD, MPH simultaneously or separate them by 4 weeks. Tuberculosis (PPD) skin test should be administered General Medicine before or on the same day as a live virus vaccine or they need to be spaced 4-6 weeks apart. Katie Barwig, RN, MS This guideline follows recommendations of the federal Advisory Committee on Immunization Practices: Nursing Administration These vaccinations should be performed [strength of recommendation] for indicated populations at risk. Sherry L DeLoach, Evidence for each vaccine is based on randomized controlled trials [level of evidence] in general PharmD population and some subgroups, with findings extrapolated to some subgroups. -

Healthcare Worker Vaccination Recommendations
Healthcare Personnel Vaccination Recommendations1 Vaccine Recommendations in brief Hepatitis B Give 3-dose series (dose #1 now, #2 in 1 month, #3 approximately 5 months after #2). Give IM. Obtain anti-HBs serologic testing 1–2 months after dose #3. Influenza Give 1 dose of influenza vaccine annually. Give inactivated injectable influenza vaccine intramuscularly or live attenuated influenza vaccine (LAIV) intranasally. MMR For healthcare personnel (HCP) born in 1957 or later without serologic evidence of immunity or prior vaccination, give 2 doses of MMR, 4 weeks apart. For HCP born prior to 1957, see below. Give SC. Varicella For HCP who have no serologic proof of immunity, prior vaccination, or history of varicella disease, (chickenpox) give 2 doses of varicella vaccine, 4 weeks apart. Give SC. Tetanus, diphtheria, Give a one-time dose of Tdap as soon as feasible to all HCP who have not received Tdap previously. pertussis Give Td boosters every 10 years thereafter. Give IM. Meningococcal Give 1 dose to microbiologists who are routinely exposed to isolates of N. meningitidis. Give IM or SC. Hepatitis A, typhoid, and polio vaccines are not routinely recommended for HCP who may have on-the-job exposure to fecal material. Hepatitis B level of immunity upon testing should be considered nonimmune) or (b) Healthcare personnel (HCP) who perform tasks that may involve exposure to appropriate vaccination against measles, mumps, and rubella (i.e., 2 doses blood or body fluids should receive a 3-dose series of hepatitis B vaccine at of live measles and mumps vaccines given on or after the first birthday, 0-, 1-, and 6-month intervals. -

Assessment of Perinatal Hepatitis B and Rubella Prevention in New Hampshire Delivery Hospitals
Assessment of Perinatal Hepatitis B and Rubella Prevention in New Hampshire Delivery Hospitals Susan Bascom, BSN; Stephanie Miller, MPH; and Jesse Greenblatt, MD, MPH ABSTRACT. Objective. To evaluate current perfor- renatal health care providers and delivery hos- mance on recommended perinatal hepatitis B and rubella pitals play a crucial role in preventing vertical prevention practices in New Hampshire. transmission of the hepatitis B virus (HBV) and Methods. Data were extracted from 2021 paired moth- P 1 congenital rubella infection. HBV infection is an er–infant records for the year 2000 birth cohort in New established cause of both acute and chronic hepatitis, Hampshire’s 25 delivery hospitals. Assessment was done as well as cirrhosis of the liver2; transmission from a on the following: prenatal screening for hepatitis B and chronically infected woman to her infant accounts rubella, administration of the hepatitis B vaccine birth for ϳ24% of chronic HBV infections in the United dose to all infants, administration of hepatitis B immune 3,4 globulin to infants who were born to hepatitis B surface States. To prevent perinatal HBV infection, the Ad- antigen–positive mothers, rubella immunity, and admin- visory Committee on Immunization Practices (ACIP) istration of in-hospital postpartum rubella vaccine to ru- and the American Academy of Pediatrics (AAP) rec- bella nonimmune women. ommend routine prenatal screening to identify Results. Prenatal screening rates for hepatitis B women who carry the hepatitis B surface antigen (98.8%) and rubella (99.4%) were high. Hepatitis B vac- (HBsAg); newborns who are born to such women cine birth dose was administered to 76.2% of all infants. -

Epilepsy in Children After Pandemic Influenza Vaccination
Siri E. Håberg, MD, PhD, a Kari M. Aaberg, MD, a, b Pål Surén, MD, PhD, a, b Lill Trogstad, MD, PhD,a Sara Ghaderi, MSc, PhD, a EpilepsyCamilla Stoltenberg, MD, PhD, in a, c Per Children Magnus, MD, PhD, a, d Inger JohanneAfter Bakken, MSc, PhDa Pandemic Influenza Vaccination OBJECTIVES: abstract To determine if pandemic influenza vaccination was associated with an increased METHODS: risk of epilepsy in children. Information from Norwegian registries from 2006 through 2014 on all children <18 years living in Norway on October 1, 2009 was used in Cox regression models to estimate hazard ratios for incident epilepsy after vaccination. A self-controlled case series analysis was used to estimate incidence rate ratios in defined risk periods after pandemic RESULTS: vaccination. In Norway, the main period of the influenza A subtype H1N1 pandemic was from October 2009 to December 2009. On October 1, 2009, 1154 113 children <18 years of age were registered as residents in Norway. Of these, 572875 (50.7%) were vaccinated against pandemic influenza. From October 2009 through 2014 there were 3628 new – cases of epilepsy (incidence rate 6.09 per 10000 person-years). The risk of epilepsy was not increased after vaccination: hazard ratio: 1.07; 95% confidence interval: 0.94 1.23. Results from the self-controlled case series analysis supported the finding of no association CONCLUSIONS: between vaccination and subsequent epilepsy. Pandemic influenza vaccination was not associated with increased risk of epilepsy. Concerns about pandemic vaccination causing epilepsy in children seem to be unwarranted. aNorwegian Institute of Public Health, Oslo, Norway; bThe National Center for Epilepsy, Oslo University Hospital, WHT A ’S KNOWN on THIS SUBJECT: Influenza Oslo, Norway; cDepartment of Global Public Health and Community Care, University of Bergen, Bergen, Norway; vaccination has been associated with an increased and dInstitute of Health and Society, University of Oslo, Oslo, Norway risk of febrile seizures in children. -

Recommendations for Immunizations and TB Testing for Health Science Students
Recommendations for Immunizations and TB Testing for Health Science Students Overview Influenza: 1 dose of inactivated Influenza vaccine yearly. Hepatitis B: 3-dose series of hepatitis B vaccine given at 0, 1 and 6 months AND documented quantitative hepatitis B surface antibody titer consistent with immunity after the appropriate vaccine series. Measles/Mumps/Rubella (MMR): 2 doses of MMR vaccine at least 28 days apart after 12 months of age OR 2 doses of measles and 2 doses of Mumps at least 28 days apart after 12 months of age and one dose of rubella after 12 months of age OR laboratory proof of immunity to measles/mumps/rubella. Tetanus/Diphtheria/Pertussis: In addition to primary series, all Health Care Personnel (HCP) should receive 1 dose of Tdap and have documentation of a Td or Tdap within the past 10 years. Tuberculosis Testing: The CDC recommends initial base line testing with a 2-step TB skin test or a blood test for TB infection. Subsequent annual or serial screening is determined by state regulations or risk assessment. Varicella: 2 doses of varicella vaccine given at least 4 weeks apart OR laboratory proof of immunity for those with a history of disease. If titer is negative or equivocal, give 2-dose varicella vaccine series. Do not repeat titer after series completion. Hepatitis B: Students must have a series of 3 hepatitis B vaccines AND a positive (≥10 mIU/mL) serological quantitative Hepatitis B surface antibody titer (anti-HBs or HBsAb) that was performed at least 1-2 months after the 3rd dose of hepatitis B vaccine.