2021 Medicare Vaccine Coverage Part B Vs Part D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RNA-Based Adjuvant CV8102 Enhances the Immunogenicity of a Licensed Rabies Vaccine in a first-In-Human Trial
Vaccine 37 (2019) 1819–1826 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine RNA-based adjuvant CV8102 enhances the immunogenicity of a licensed rabies vaccine in a first-in-human trial Fatma Doener a,1, Henoch S. Hong a,1, Ingo Meyer b,1, Keyvan Tadjalli-Mehr c, Angelika Daehling c, ⇑ Regina Heidenreich a, Sven D. Koch a, Mariola Fotin-Mleczek a, Ulrike Gnad-Vogt c, a Curevac AG, Paul-Ehrlich-Strasse 15, 72076 Tübingen, Germany b CRS Clinical Research Services Mönchengladbach GmbH, 41061 Mönchengladbach, Germany c Curevac AG, Schumannstrasse 27, 60325 Frankfurt, Germany article info abstract Article history: Background: We report the first-in-concept human trial of the safety, tolerability and immunogenicity Received 27 September 2018 when a novel TLR 7/8/RIG I agonist RNA-based adjuvant, CV8102, was administered alone or mixed with Received in revised form 30 January 2019 fractional doses of a licensed rabies vaccine (RabipurÒ) as model antigen. Accepted 3 February 2019 Methods: The primary objective was to assess the safety and reactogenicity of various dose levels of Available online 21 February 2019 CV8102 alone or mixed with RabipurÒ in healthy 18–40 year-old male volunteers. A secondary objective was to assess the immune-enhancing potential of bedside-mixes of CV8102 with fractional doses of Keywords: Ò Rabipur by measuring induction of rabies virus neutralising titres (VNTs). Adjuvant Results: Fifty-six volunteers received 50–100 lg CV8102 alone (n = 11), bedside-mixed CV8102 and RNA Ò Ò Ò Rabies Rabipur (n = 20), or Rabipur alone (n = 25; control). -

Healthcare Personnel Vaccination Recommendations1 Vaccine Recommendations in Brief
Healthcare Personnel Vaccination Recommendations1 Vaccine Recommendations in brief Hepatitis B Give 3-dose series (dose #1 now, #2 in 1 month, #3 approximately 5 months after #2). Give IM. Obtain anti-HBs serologic testing 1–2 months after dose #3. Influenza Give 1 dose of influenza vaccine annually. Give inactivated injectable influenza vaccine intramuscularly or live attenuated influenza vaccine (LAIV) intranasally. MMR For healthcare personnel (HCP) born in 1957 or later without serologic evidence of immunity or prior vaccination, give 2 doses of MMR, 4 weeks apart. For HCP born prior to 1957, see below. Give SC. Varicella For HCP who have no serologic proof of immunity, prior vaccination, or history of varicella disease, (chickenpox) give 2 doses of varicella vaccine, 4 weeks apart. Give SC. Tetanus, diphtheria, Give a one-time dose of Tdap as soon as feasible to all HCP who have not received Tdap previously. pertussis Give Td boosters every 10 years thereafter. Give IM. Meningococcal Give 1 dose to microbiologists who are routinely exposed to isolates of N. meningitidis. Give IM or SC. Hepatitis A, typhoid, and polio vaccines are not routinely recommended for HCP who may have on-the-job exposure to fecal material. Hepatitis B Healthcare personnel (HCP) who perform tasks that may involve exposure to of live rubella vaccine). HCP with 2 documented doses of MMR are not blood or body fluids should receive a 3-dose series of hepatitis B vaccine at recommended to be serologically tested for immunity; but if they are tested 0-, 1-, and 6-month intervals. Test for hepatitis B surface antibody (anti-HBs) and results are negative or equivocal for measles, mumps, and/or rubella, to document immunity 1–2 months after dose #3. -

Rotavirus Vaccine for the Prevention of Rotavirus Gastroenteritis Among Children
March 19, 1999 / Vol. 48 / No. RR-2 Recommendations and Reports Rotavirus Vaccine for the Prevention of Rotavirus Gastroenteritis Among Children Recommendations of the Advisory Committee on Immunization Practices (ACIP) Continuing Education Examination Education Continuing Inside: U.S. DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Disease Control and Prevention (CDC) Atlanta, Georgia 30333 The MMWR series of publications is published by the Epidemiology Program Office, Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services, Atlanta, GA 30333. SUGGESTED CITATION Centers for Disease Control and Prevention. Rotavirus vaccine for the prevention of rotavirus gastroenteritis among children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1999;48(No. RR-2):[inclu- sive page numbers]. Centers for Disease Control and Prevention....................Jeffrey P. Koplan, M.D., M.P.H. Director The material in this report was prepared for publication by National Center for Infectious Diseases.................................. James M. Hughes, M.D. Director Division of Viral and Rickettsial Diseases ................. Brian W. J. Mahy, Ph.D., Sc.D. Director National Immunization Program ...........................................Walter A. Orenstein, M.D. Director Epidemiology and Surveillance Division ...........................John R. Livengood, M.D. Director The production of this report as an MMWR serial publication was coordinated in Epidemiology Program Office.................................... Stephen B. Thacker, M.D., M.Sc. Director Office of Scientific and Health Communications ......................John W. Ward, M.D. Director Editor, MMWR Series Recommendations and Reports................................... Suzanne M. Hewitt, M.P.A. Managing Editor Valerie R. Johnson Project Editor Morie M. Higgins Visual Information Specialist Vol. 48 / No. RR-2 MMWR i Contents Clinical and Epidemiologic Features of Rotavirus Disease............................................. -

(ACIP) General Best Guidance for Immunization
9. Special Situations Updates Major revisions to this section of the best practices guidance include the timing of intramuscular administration and the timing of clotting factor deficiency replacement. Concurrent Administration of Antimicrobial Agents and Vaccines With a few exceptions, use of an antimicrobial agent does not interfere with the effectiveness of vaccination. Antibacterial agents have no effect on inactivated, recombinant subunit, or polysaccharide vaccines or toxoids. They also have no effect on response to live, attenuated vaccines, except BCG vaccines. Antimicrobial or immunosuppressive agents may interfere with the immune response to BCG and should only be used under medical supervision (for additional information, see www.merck.com/product/usa/pi_circulars/b/bcg/bcg_pi.pdf). Antiviral drugs used for treatment or prophylaxis of influenza virus infections have no effect on the response to inactivated influenza vaccine (2). However, live, attenuated influenza vaccine should not be administered until 48 hours after cessation of therapy with antiviral influenza drugs. If feasible, to avoid possible reduction in vaccine effectiveness, antiviral medication should not be administered for 14 days after LAIV administration (2). If influenza antiviral medications are administered within 2 weeks after receipt of LAIV, the LAIV dose should be repeated 48 or more hours after the last dose of zanamavir or oseltamivir. The LAIV dose should be repeated 5 days after peramivir and 17 days after baloxavir. Alternatively, persons receiving antiviral drugs within the period 2 days before to 14 days after vaccination with LAIV may be revaccinated with another approved vaccine formulation (e.g., IIV or recombinant influenza vaccine). Antiviral drugs active against herpesviruses (e.g., acyclovir or valacyclovir) might reduce the efficacy of vaccines containing live, attenuated varicella zoster virus (i.e., Varivax and ProQuad) (3,4). -

362.Full.Pdf
AMERICAN ACADEMY OF PEDIATRICS Committee on Infectious Diseases Policy Statement: Recommendations for the Prevention of Pneumococcal Infections, Including the Use of Pneumococcal Conjugate Vaccine (Prevnar), Pneumococcal Polysaccharide Vaccine, and Antibiotic Prophylaxis ABSTRACT. Heptavalent pneumococcal conjugate vac- lular pertussis; HbOC, Haemophilus influenzae type b conjugate cine (PCV7) is recommended for universal use in chil- vaccine; HIV, human immunodeficiency virus; AOM, acute otitis dren 23 months and younger, to be given concurrently media. with other recommended childhood vaccines at 2, 4, 6, and 12 to 15 months of age. For children 7 to 23 months he purpose of this report is to provide recom- old who have not received previous doses of PCV7, ad- ministration of a reduced number of doses is recom- mendations for use of the heptavalent pneumo- mended. Two doses of PCV7 are recommended for chil- Tcoccal conjugate vaccine (PCV7), Prevnar (Led- dren 24 to 59 months old at high risk of invasive erle Laboratories, Pearl River, NY; Wyeth-Ayerst pneumococcal infection—including children with func- Pharmaceuticals, Marietta, PA), and 23-valent pneumo- tional, anatomic, or congenital asplenia; infection with coccal polysaccharide (23PS) vaccines. In addition, rec- human immunodeficiency virus; and other predisposing ommendations for the continuing use of antibiotic pro- conditions—who have not been immunized previously phylaxis in children with sickle cell disease (SCD) and with PCV7. Recommendations have been made for use of asplenia will be given, and the use of antibiotics and 23-valent pneumococcal polysaccharide (23PS) vaccine in vaccines in children who attend out-of-home care will high-risk children to expand serotype coverage. -

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -

Mmrv Vaccine
VACCINE INFORMATION STATEMENT (Measles, Mumps, Many Vaccine Information Statements are available in Spanish and other languages. MMRV Vaccine Rubella and See www.immunize.org/vis Varicella) Hojas de información sobre vacunas están disponibles en español y en muchos otros What You Need to Know idiomas. Visite www.immunize.org/vis These are recommended ages. But children can get the Measles, Mumps, Rubella and second dose up through 12 years as long as it is at least 1 Varicella 3 months after the first dose. Measles, Mumps, Rubella, and Varicella (chickenpox) can be serious diseases: Children may also get these vaccines as 2 separate shots: MMR (measles, mumps and rubella) and Measles varicella vaccines. • Causes rash, cough, runny nose, eye irritation, fever. • Can lead to ear infection, pneumonia, seizures, brain 1 Shot (MMRV) or 2 Shots (MMR & Varicella)? damage, and death. • Both options give the same protection. Mumps • One less shot with MMRV. • Causes fever, headache, swollen glands. • Children who got the first dose as MMRV have • Can lead to deafness, meningitis (infection of the brain had more fevers and fever-related seizures (about and spinal cord covering), infection of the pancreas, 1 in 1,250) than children who got the first dose as painful swelling of the testicles or ovaries, and, rarely, separate shots of MMR and varicella vaccines on death. the same day (about 1 in 2,500). Rubella (German Measles) Your doctor can give you more information, • Causes rash and mild fever; and can cause arthritis, including the Vaccine Information Statements for (mostly in women). MMR and Varicella vaccines. -

Proquad, INN-Measles, Mumps, Rubella and Varicella Vaccine (Live)
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT ProQuad powder and solvent for suspension for injection ProQuad powder and solvent for suspension for injection in a pre-filled syringe Measles, mumps, rubella and varicella vaccine (live). 2. QUALITATIVE AND QUANTITATIVE COMPOSITION After reconstitution, one dose (0.5 mL) contains: 1 Measles virus Enders’ Edmonston strain (live, attenuated) ........ not less than 3.00 log10 TCID * 50 1 Mumps virus Jeryl Lynn™ (Level B) strain (live, attenuated) ... not less than 4.30 log10 TCID * 50 2 Rubella virus Wistar RA 27/3 strain (live, attenuated)............... not less than 3.00 log10 TCID * 50 3 Varicella virus Oka/Merck strain (live, attenuated) ................... not less than 3.99 log10 PFU** *50% tissue culture infectious dose **plaque-forming units (1) Produced in chick embryo cells. (2) Produced in human diploid lung (WI-38) fibroblasts. (3) Produced in human diploid (MRC-5) cells. The vaccine may contain traces of recombinant human albumin (rHA). This vaccine contains a trace amount of neomycin. See section 4.3. Excipient(s) with known effect The vaccine contains 16 milligrams of sorbitol per dose. See section 4.4. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder and solvent for suspension for injection Before reconstitution, the powder is a white to pale yellow compact crystalline cake and the solvent is a clear colourless liquid. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications ProQuad is indicated for simultaneous vaccination against measles, mumps, rubella and varicella in individuals from 12 months of age. ProQuad can be administered to individuals from 9 months of age under special circumstances (e.g., to conform with national vaccination schedules, outbreak situations, or travel to a region with high prevalence of measles; see sections 4.2, 4.4, and 5.1). -

Yellow Fever Vaccine See Hojas De Información Sobre Vacunas Están Disponibles En Español Y En Muchos Otros What You Need to Know Idiomas
VACCINE INFORMATION STATEMENT Many Vaccine Information Statements are available in Spanish and other languages. Yellow Fever Vaccine See www.immunize.org/vis Hojas de información sobre vacunas están disponibles en español y en muchos otros What You Need to Know idiomas. Visite www.immunize.org/vis 1 What is yellow fever? 3 Yellow fever vaccine Yellow fever is a serious disease caused by the yellow Yellow fever vaccine is a live, weakened virus. It is fever virus. It is found in certain parts of Africa and given as a single shot. For people who remain at risk, a South America. booster dose is recommended every 10 years. Yellow fever is spread through the bite of an infected Yellow fever vaccine may be given at the same time as mosquito. It cannot be spread person to person by direct most other vaccines. contact. Who should get yellow fever vaccine? People with yellow fever disease usually have to be • Persons 9 months through 59 years of age traveling hospitalized. Yellow fever can cause: to or living in an area where risk of yellow fever is • fever and flu-like symptoms known to exist, or traveling to a country with an entry • jaundice (yellow skin or eyes) requirement for the vaccination. • bleeding from multiple body sites • Laboratory personnel who might be exposed to yellow • liver, kidney, respiratory and other organ failure fever virus or vaccine virus. • death (20% - 50% of serious cases) Information for travelers can be found online through CDC (www.cdc.gov/travel), the World Health 2 How can I prevent yellow fever? Organization (www.who.int), and the Pan American Health Organization (www.paho.org). -

Recombivax HB , YF-Vax – Drug Shortages
Recombivax HB®, YF-Vax® – Drug shortages • The drug shortages of Recombivax HB (hepatitis B vaccine, recombinant) and YF-Vax (yellow fever virus strain 17d-204 live antigen) are ongoing. Recombivax HB and YF-Vax have been unavailable for at least 90 days. Product Description NDC # Recombivax HB (hepatitis B vaccine, recombinant) 0.5 mL (5 mcg) 0006-4981-00, 0006- pediatric/adolescent formulation 4093-02, 0006-4093-09 single-dose vials and prefilled syringes Recombivax HB (hepatitis B vaccine, 0006-4995-00, 0006- recombinant) 1 mL (10 mcg) adult 4995-41, 0006-4094-02, formulation single-dose vials and 0006-4094-09 prefilled syringes YF-Vax (yellow fever virus strain 17-d- 49281-0915-01, 49281- 2014 live antigen) single- and multi- 0915-05 dose vials — The shortage of Recombivax HB is due to increased global demand. — The Recombivax HB pediatric/adolescent and adult formulations are estimated to be available in the first half of 2018 and the first half of 2019, respectively. — The Recombivax HB dialysis formulation is available; however, the dose is different than the adult and pediatric/adolescent formulations. — YF-Vax is unavailable because the manufacturer, Sanofi Pasteur, is transitioning production to a new facility in 2018. YF-Vax is estimated to be available by mid-2018. • Recombivax HB is indicated for prevention of infection caused by all known subtypes of hepatitis B virus. — Engerix-B™ (hepatitis B vaccine, recombinant) is another currently available vaccine that carries the same indication as Recombivax HB. Engerix-B is not in shortage. — Heplisav-B™ (hepatitis B vaccine, recombinant) was recently approved and carries the same indication as Recombivax HB. -

USDA-Approved Animal Rabies Vaccines
United States Department of Agriculture (USDA) Approved Animal Rabies Vaccines Table 1. Rabies Vaccines Licensed and Marketed in the United States, 2016 Age at For use Route of Product Name Produced by Marketed by Dose primary Booster vaccination in inoculation vaccination* A) MONOVALENT (Inactivated) RAB RABVAC 1 Boehringer Boehringer Dogs 1 ml 3 months Annually IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months Annually IM or SC Vetmedica Inc Inc License No. 124 RABVAC 3 Boehringer Boehringer Dogs 1 ml 3 months 1 year later & triennially IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months 1 year later & triennially IM or SC Vetmedica Inc Inc Horses 2 ml 3 months Annually IM License No. 124 EQUIRAB with Merck Animal Merck Animal Health Horses 1 ml 4 months Annually IM Havlogen Health License No. 165A DEFENSOR 1 Zoetis Zoetis Dogs 1 ml 3 months Annually IM or SC License No. 190 Cats 1 ml 3 months Annually SC DEFENSOR 3 Zoetis Zoetis Dogs 1 ml 3 months 1 year later & triennially IM or SC License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM NOBIVAC: 1- Zoetis Merck Animal Health Dogs 1 ml 3 months Annually IM or SC Rabies License No. 190 Cats 1 ml 3 months Annually SC NOBIVAC: 3- Zoetis Merck Animal Health Dogs 1 ml 3 months 1 year later & triennially IM or SC Rabies and 3- License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Rabies CA Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM IMRAB 1 Merial, Inc Merial, Inc Dogs 1 ml 3 months Annually SC License No. -
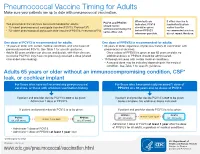
Pneumococcal Vaccine Timing for Adults Make Sure Your Patients Are up to Date with Pneumococcal Vaccination
Pneumococcal Vaccine Timing for Adults Make sure your patients are up to date with pneumococcal vaccination. When both are If either vaccine is PCV13 and PPSV23 Two pneumococcal vaccines are recommended for adults: indicated, PCV13 inadvertently given should not be 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar13®) should be given earlier than the administered during the ® before PPSV23 recommended window, 23-valent pneumococcal polysaccharide vaccine (PPSV23, Pneumovax 23) same office visit. whenever possible. do not repeat the dose. One dose of PCV13 is recommended for adults: One dose of PPSV23 is recommended for adults: 19 years or older with certain medical conditions and who have not 65 years or older, regardless of previous history of vaccination with previously received PCV13. See Table 1 for specific guidance. pneumococcal vaccines. Adults 65 years or older can discuss and decide, with their clinician, – Once a dose of PPSV23 is given at age 65 years or older, no to receive PCV13 if they have not previously received a dose (shared additional doses of PPSV23 should be administered. clinical decision-making). 19 through 64 years with certain medical conditions. – A second dose may be indicated depending on the medical condition. See Table 1 for specific guidance. Adults 65 years or older without an immunocompromising condition, CSF* leak, or cochlear implant For those who have not received any pneumococcal For those who have previously received 1 dose of vaccines, or those with unknown vaccination history PPSV23 at ≥ 65 years and no doses of PCV13 If patient and provider decide PCV13 is not to be given: If patient and provider decide PCV13 is not to be given: Administer 1 dose of PPSV23.