Vaccines for Preteens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -
Pneumococcal Vaccine
Vaccines for Primary Care Pneumococcal, Shingles, Pertussis Devang Patel, M.D. Assistant Professor Chief of Service, MICU ID Service University of Maryland School of Medicine Pneumococcal Vaccine Pneumococcal Disease • 2nd most common cause of vaccine preventable death in the US • Major Syndromes – Pneumonia – Bacteremia – Meningitis Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network Streptococcus pneumoniae, 2010 (ORIG) Vaccine Target • Polysaccharide capsule allows bacteria to resist phagocytosis • Antibodies to capsule facilitate phagocytosis • >90 different pneumococcal capsular serotypes • Vaccines contain most common serotypes causing disease Pneumococcal Vaccines Pneumococcal Vaccines • Pneumococcal polysaccharide vaccine (PPSV23; Pneumovax) – Contains capsular polysaccharides – 23 most commonly infecting serotypes • Cause 60% of all pneumococcal infections in adults – Not recommended for children <2 due to poor immunogenicity of polysaccharides Pneumococcal Vaccines • Pneumococcal conjugate vaccine (PCV13, Prevnar) – Polysaccharides linked to nontoxic protein • higher antigenicity – Stimulates mucosal antibody • Eliminates nasal carriage in young children • Herd effect in adults – Reduction in PCV7 serotype disease >90% Prevnar 13 • 2000 - PCV7 approved for infants toddlers • 2010 - PCV13 recommended for infants and toddlers • 2012 – ACIP recommended PCV13 for high- risk adults • 2014 – recommended for adults >65 • 2018 – ACIP will revisit PCV13 use in adults – Childhood vaccines may eliminate -

HPV Vaccine Safety - Vaccine Safety
CDC - HPV Vaccine Safety - Vaccine Safety Skip directly to search Skip directly to A to Z list Skip directly to navigation Skip directly to site content Skip directly to page options CDC Home CDC 24/7: Saving Lives. Protecting People.™ Search The CDC Vaccine Safety Vaccine Safety Vaccines Safety Basics Diphtheria, Tetanus, and Pertussis Vaccines: DTaP, Td, and Tdap Haemophilus Influenzae Type B (Hib) Hib Summary Human Papillomavirus (HPV) FAQs about HPV Vaccine Safety FAQ: Gardasil Vaccine recall JAMA Report Summary Information from FDA and CDC on Gardasil and its Safety (Archived) Measles, Mumps, Rubella (MMR) MMR Vaccine Safety Studies Measles, Mumps, Rubella, Varicella (MMRV) Information on the VSD MMRV Vaccine Safety Study MMRV Vaccine Safety Studies MMRV and Febrile Seizures Rotavirus Varicella Addressing Common Concerns Adjuvants Autism Vaccine not associated with autism CDC Statement: 2004 Pediatrics Paper CDC Statement on Pandemrix Fainting (Syncope) FAQs about Fainting (Syncope) After Vaccination Childhood Vaccines and Febrile Seizures Influenza Season 2012-2013 Influenza Season 2010-2011 GBS GBS and Menactra Meningococcal Vaccine FAQs about GBS and Menactra Meningococcal Vaccine IOM Assessment of Studies on Childhood Immunization Schedule IOM Report on Adverse Effects of Vaccines Pregnancy and Influenza Vaccine Safety Sudden Infant Death Syndrome (SIDS) Thimerosal http://www.cdc.gov/vaccinesafety/vaccines/HPV/index.html[10/13/2014 5:59:00 PM] CDC - HPV Vaccine Safety - Vaccine Safety CDC Study on Thimerosal and Risk of Autism -
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
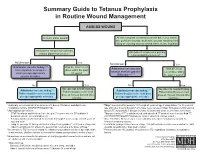
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

COVID-19 and Cancer: from Basic Mechanisms to Vaccine Development Using Nanotechnology
International Immunopharmacology 90 (2021) 107247 Contents lists available at ScienceDirect International Immunopharmacology journal homepage: www.elsevier.com/locate/intimp Review COVID-19 and cancer: From basic mechanisms to vaccine development using nanotechnology Hyun Jee Han a,*, Chinekwu Nwagwu b, Obumneme Anyim c, Chinedu Ekweremadu d, San Kim e a University College London, Department of Neonatology, United Kingdom b Department of Pharmaceutics, University of Nigeria Nsukka, Nigeria c Department of Internal Medicine, University of Nigeria Teaching Hospital Ituku-Ozalla, Enugu, Nigeria d Department of Pharmaceutics and Pharmaceutical Technology Enugu State University of Science and Technology, Nigeria e Basildon and Thurrock University Hospital, United Kingdom ARTICLE INFO ABSTRACT Keywords: Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV- COVID-19 2), is a global pandemic which has induced unprecedented ramifications,severely affecting our society due to the Cancer long incubation time, unpredictably high prevalence and lack of effective vaccines. One of the interesting notions Vaccine development is that there is an association between COVID-19 and cancer. Cancer patients seem to exhibit exacerbated Pharmaceutics conditions and a higher mortality rate when exposed to the virus. Therefore, vaccines are the promising solution Nanotechnology to minimise the problem amongst cancer patients threatened by the new viral strains. However, there are still limitations to be considered, including the efficacy of COVID vaccines for immunocompromised individuals, possible interactions between the vaccine and cancer, and personalised medicine. Not only to eradicate the pandemic, but also to make it more effective for immunocompromised patients who are suffering from cancer, a successful vaccine platform is required through the implementation of nanotechnology which can also enable scalable manufacturing and worldwide distribution along with its faster and precise delivery. -

YF-VAX® Rx Only AHFS Category
YF-VAX® Rx Only Laboratory Personnel AHFS Category: 80:12 Laboratory personnel who handle virulent yellow fever virus or concentrated preparations Rx only of the yellow fever vaccine virus strains may be at risk of exposure by direct or indirect Yellow Fever Vaccine contact or by aerosols. (14) DESCRIPTION CONTRAINDICATIONS ® Hypersensitivity YF-VAX , Yellow Fever Vaccine, for subcutaneous use, is prepared by culturing the YF-VAX is contraindicated in anyone with a history of acute hypersensitivity reaction to any 17D-204 strain of yellow fever virus in living avian leukosis virus-free (ALV-free) chicken component of the vaccine. (See DESCRIPTION section.) Because the yellow fever virus embryos. The vaccine contains sorbitol and gelatin as a stabilizer, is lyophilized, and is used in the production of this vaccine is propagated in chicken embryos, do not administer hermetically sealed under nitrogen. No preservative is added. Each vial of vaccine is YF-VAX to anyone with a history of acute hypersensitivity to eggs or egg products due to supplied with a separate vial of sterile diluent, which contains Sodium Chloride Injection a risk of anaphylaxis. Less severe or localized manifestations of allergy to eggs or to USP – without a preservative. YF-VAX is formulated to contain not less than 4.74 log10 feathers are not contraindications to vaccine administration and do not usually warrant plaque forming units (PFU) per 0.5 mL dose throughout the life of the product. Before vaccine skin testing. (See PRECAUTIONS section, Testing for Hypersensitivity Re- reconstitution, YF-VAX is a pinkish color. After reconstitution, YF-VAX is a slight pink-brown actions subsection.) Generally, persons who are able to eat eggs or egg products may suspension. -
Commonly Administered Vaccines
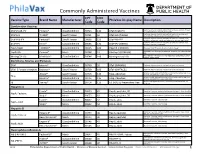
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular -

Meningococcal Vaccine Q & a for Healthcare Providers
Meningococcal Vaccine Q & A for Healthcare Providers School meningococcal vaccine requirements Q1: When did the school meningococcal vaccine requirement take effect? A1: The meningococcal vaccine school requirement took effect on September 1, 2016. Q2: For what grades is meningococcal vaccine required? A2: Meningococcal vaccine is currently required for students entering or attending grades 7 through 12 in public, private and parochial New York State (NYS) schools. Q3: How many doses of meningococcal vaccine are required for grades 7 through 11? A3: One dose of meningococcal conjugate vaccine (MenACWY; sometimes abbreviated as MCV4; brand names Menactra or Menveo) is required for entry into grades 7 through 11. Q4: How many doses of meningococcal vaccine are required for grade 12? A4: A total of two doses of MenACWY vaccine, administered a minimum of 8 weeks apart, are required for entry into grade 12. The second dose must be administered no sooner than 16 years of age. However, if the first dose of MenACWY vaccine was received at 16 years of age or older, then a second dose will not be required. The NYS school immunization requirements allow for a grace period of up to 4 days before the 16th birthday for receipt of the dose. A dose of vaccine received 5 or more days before the 16th birthday will not meet the 12th grade meningococcal vaccine requirement. Q5: Is serogroup B meningococcal vaccine (MenB vaccine) required for grade 12? A5: No, MenB vaccine is not required for school attendance in NYS. In addition, doses of MenB vaccine will not meet the NYS MenACWY vaccine requirement. -

Supplemental Information and Guidance for Vaccination Providers Regarding Use of 9-Valent HPV Vaccine
Supplemental information and guidance for vaccination providers regarding use of 9-valent HPV A 9-valent human papillomavirus (HPV) vaccine (9vHPV, Gardasil 9, Merck & Co.) was licensed for use in females and males in December 2014.1,2,3,4 The 9vHPV was the third HPV vaccine licensed in the United States by the Food and Drug Administration (FDA); the other vaccines are bivalent HPV vaccine (2vHPV, Cervarix, GlaxoSmithKline), licensed for use in females, and quadrivalent HPV vaccine (4vHPV, Gardasil, Merck & Co.), licensed for use in females and males.5 In February 2015, the Advisory Committee on Immunization Practices (ACIP) recommended 9vHPV as one of three HPV vaccines that can be used for routine vaccination of females and one of two HPV vaccines for routine vaccination of males.6 After the end of 2016, only 9vHPV will be distributed in the United States. In October 2016, ACIP updated HPV vaccination recommendations regarding dosing schedules.7 CDC now recommends two doses of HPV vaccine (0, 6–12 month schedule) for persons starting the vaccination series before the 15th birthday. Three doses of HPV vaccine (0, 1–2, 6 month schedule) continue to be recommended for persons starting the vaccination series on or after the 15th birthday and for persons with certain immunocompromising conditions. Guidance is needed for persons who started the series with 2vHPV or 4vHPV and may be completing the series with 9vHPV. The information below summarizes some of the recommendations included in ACIP Policy Notes and provides additional guidance.5-7 Information about the vaccines What are some of the similarities and differences between the three HPV vaccines? y Each of the three HPV vaccines is a noninfectious, virus-like particle (VLP) vaccine. -

Recommended Adult Immunization Schedule
Recommended Adult Immunization Schedule UNITED STATES for ages 19 years or older 2021 Recommended by the Advisory Committee on Immunization Practices How to use the adult immunization schedule (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Determine recommended Assess need for additional Review vaccine types, Control and Prevention (www.cdc.gov), American College of Physicians 1 vaccinations by age 2 recommended vaccinations 3 frequencies, and intervals (www.acponline.org), American Academy of Family Physicians (www.aafp. (Table 1) by medical condition and and considerations for org), American College of Obstetricians and Gynecologists (www.acog.org), other indications (Table 2) special situations (Notes) American College of Nurse-Midwives (www.midwife.org), and American Academy of Physician Assistants (www.aapa.org). Vaccines in the Adult Immunization Schedule* Report y Vaccines Abbreviations Trade names Suspected cases of reportable vaccine-preventable diseases or outbreaks to the local or state health department Haemophilus influenzae type b vaccine Hib ActHIB® y Clinically significant postvaccination reactions to the Vaccine Adverse Event Hiberix® Reporting System at www.vaers.hhs.gov or 800-822-7967 PedvaxHIB® Hepatitis A vaccine HepA Havrix® Injury claims Vaqta® All vaccines included in the adult immunization schedule except pneumococcal 23-valent polysaccharide (PPSV23) and zoster (RZV) vaccines are covered by the Hepatitis A and hepatitis B vaccine HepA-HepB Twinrix® Vaccine Injury Compensation Program. Information on how to file a vaccine injury Hepatitis B vaccine HepB Engerix-B® claim is available at www.hrsa.gov/vaccinecompensation. Recombivax HB® Heplisav-B® Questions or comments Contact www.cdc.gov/cdc-info or 800-CDC-INFO (800-232-4636), in English or Human papillomavirus vaccine HPV Gardasil 9® Spanish, 8 a.m.–8 p.m. -

PROOF of IMMUNIZATION COMPLIANCE NORTHWESTERN STATE UNIVERSITY of LOUISIANA (Louisiana R.S
PROOF OF IMMUNIZATION COMPLIANCE NORTHWESTERN STATE UNIVERSITY OF LOUISIANA (Louisiana R.S. 17:170.1 Schools of Higher Learning) SS Number: _____________________________________________ Date of Birth: Month _________________ Date ___________________ Year ________________ Name: __________________________________________________________________________________________________________________________________ Please Print (Last) (First) (Middle) Address: ________________________________________________________________________________________________________________________________ City: ______________________________________________________ State: ________________________________ ZIP Code: _____________________________ UNIVERSITY REQUIRED IMMUNIZATIONS: Physician or Other Health Care Provider Verification: (See other side) M-M-R (Measles, Mumps, Rubella-2 Doses Required) Tetanus Diphtheria (Td) Pertussis (Tdap) OR First dose: ___________________ Serologic Test: __________________ Td: ___________________ (Date) (Date within 10 years) (Date) OR Second dose: __________________ (Date) Result: _________________________ (Date) Tdap: ___________________ (Date within 10 years) OR □ Born before 1956 Meningitis Vaccine ACYW-135 (TWO doses of meningococcal conjugate vaccination separated by at least eight weeks.) First dose: ____________________________________ Vaccine Type: _______________________________________ (Date) Second dose: __________________________________ Vaccine Type: _______________________________________ (Date) UNIVERSITY REQUIRED IMMUNIZATIONS: -

3.2.3 Gardasil and Autoimmune Diseases
HPV vaccination and autoimmune disease CONFIDENTIAL Medicines Adverse Reactions Committee Meeting date 10 September 2015 Agenda item 3.2.3 Title Gardasil and autoimmune diseases Medsafe For advice/ Submitted by Paper type Pharmacovigilance Team For information Active constituent Medicines Sponsors Human papillomavirus type 6 L1 protein, type 11 Gardasil Bio CSL for MSD L1 protein, type 16 L1 protein and type 18 L1 protein Funding Fully funded for girls aged under 18 years or patients aged under 25 years old with confirmed HIV infection or in transplant patients. Previous MARC Gardasil has only been discussed previously in relation to CARM case meetings reports. International action The EMA have announced an investigation into HPV vaccine and complex regional pain syndrome (CRPS) and postural orthostatic tachycardia syndrome (POTS). This review will complete at the end of the year. Prescriber Update None Schedule Prescription medicine Usage data Over 200,000 girls and women have received at least one dose in NZ Worldwide cumulative exposure post-marketing, to the end of May 2015 was 63.6 million. Cumulative exposure in clinical trials was 29,932 Advice sought The Committee is asked to advise whether: − There is a safety concern relating to development of autoimmune conditions after HPV vaccination Medicines Adverse Reactions Committee: 10 September 2015 Page 1 of 46 HPV vaccination and autoimmune disease CONFIDENTIAL Table of Contents 1.0 PURPOSE .................................................................................................................................